血清甲状旁腺激素水平与3~5期慢性肾脏病患者左室肥厚的相关性
2017-01-17高小芳张亚璞李建东
常 欢, 高小芳, 张亚璞, 陈 航, 郭 莉, 李建东
(1.河北大学, 河北 保定 071000; 2.河北大学附属医院 肾内科, 河北 保定 071000)
血清甲状旁腺激素水平与3~5期慢性肾脏病患者左室肥厚的相关性
常 欢1, 高小芳1, 张亚璞1, 陈 航2*, 郭 莉2, 李建东2
(1.河北大学, 河北 保定 071000; 2.河北大学附属医院 肾内科, 河北 保定 071000)
目的: 探讨血清全段甲状旁腺激素(iPTH)水平与3~5期慢性肾脏病(CKD)患者左室肥厚(LVH)的相关性。方法: 将60例首诊未行血液透析的患者按CKD的3、4、5期分为A、B、C组,超声心动图测量其射血分数(EF)、左室舒张末期内径(LVDd)、左室收缩末期内径(LVDs)、室间隔厚度(IVST)及左室后壁厚度(LVPTW),计算左室心肌重量指数(LVMI);患者入院时抽取空腹静脉血,采用全自动生化分析仪测定血清肌酐(Scr)、尿素氮(BUN)及钙(Ca2+)、磷(P)浓度,采用血细胞分析仪测定血红蛋白(HGB)、红细胞比容(HCT),采用电化学发光分析法测定血清iPTH水平;采用Spearman对血液学指标与LVMI、血清 iPTH与心功能指标的相关进行分析。结果: 3组CDK患者Scr、BUN、血清P、iPTH、LVDd、LVDs、IVST、LVPTW及LVMI随CDK分期的增加而升高,血清Ca2+、HGB、HCT及EF随CDK分期的增加而降低,Scr、BUN、iPTH、LVDd 、LVMI及EF在3组间两两比较差异有统计学意义(P<0.05),血清P、血清Ca2+、HGB、HCT、LVDs、LVPTW及IVST在3~4期CKD组与CKD5期组比较,差异有统计学意义(P<0.05);Spearman结果显示,患者血清Scr、BUN及P与LVMI呈正相关(r=0.638、0.600、0.499,P<0.01),HGB与LVMI和HCT呈负相关(r=-0.583、-0.598,P<0.01),血清Ca与LVMI无相关性(r=-0.347,P>0.01);血清iPTH水平与LVDd、LVDs及LVMI呈正相关(r=0.642、0.548、0.577,P<0.01),与IVST、LVPTW无相关性(r=0.014、0.052,P均>0.01),与EF呈负相关(r=-0.604,P<0.01)。结论: 3~5期CKD患者都可能发生左室肥厚,iPTH水平可能是影响左室结构的重要因素。
慢性肾脏病; 甲状旁腺激素; 左室肥厚; 心肌重量指数; 继发性甲状旁腺功能亢进
近年来慢性肾脏病(chronic kidney disease,CKD)的患病率有明显上升趋势,目前我国CKD的患病率为10.8%[1]。心血管病变是CKD患者常见的并发症和主要死因,尤其进入终末期肾脏病阶段,患者心血管事件及动脉粥样硬化性心血管病的发生比普通人群升高15~20倍,死亡率也增高,占尿毒症死因的45%~60%[1-2]。继发性甲状旁腺功能亢进患者血清全段甲状旁腺激素(iPTH)水平的升高可导致患者骨骼的严重损害,同时出现不同程度的皮肤瘙痒、软组织异位钙化、周围神经病变及肌肉萎缩[3-4]。本研究通过测定3~5期CKD患者射血分数(EF)、左室舒张末期内径(LVDd)、左室收缩末期内径(LVDs)、室间隔厚度(IVST)、左室后壁厚度(LVPTW),计算左室心肌重量指数(LVMI),同时测定血清肌酐(Scr)、尿素氮(BUN)及钙(Ca2+)、磷(P)及iPTH水平和血红蛋白(HGB)、红细胞比容(HCT),分析血清iPTH水平与左室肥厚指标的相关性,报道如下。
1 资料与方法
1.1 一般资料
选取2015年1月~2016年10月住院治疗的3~5期CKD期患者各20例,所有对象均为CKD首诊,未行血液透析治疗,男31例,女29例,24~79岁,平均(50.61±13.10)岁;慢性肾小球肾炎38例,糖尿病肾病15例,多囊肾2例,狼疮性肾炎2例,乙肝相关性肾损害1例,原因不明2例。排除急、慢性心血管、先天性心脏病、主动脉瓣狭窄患者,排除恶性高血压难以控制患者,排除慢性阻塞性肺疾病患者及其他异常物质沉积和遗传代谢性疾病引起的心肌肥厚患者。根据美国肾脏基金会制定的指南[1,5]将患者分为CKD3期组、CKD4期组及CKD5期组,分期以肾小球滤过率(GRF)为标准,CKD 3期GRF 30~59 mL/(min·1.73 m2), CKD4期GRF 15~29 mL/(min·1.73 m2),CKD 5期GRF<15 mL/(min·1.73 m2)为。3组CDK患者性别比、年龄、收缩压、舒张压、身高、体重等基础资料比较,差异无统计学意义(P>0.05),具有可比性。见表1。
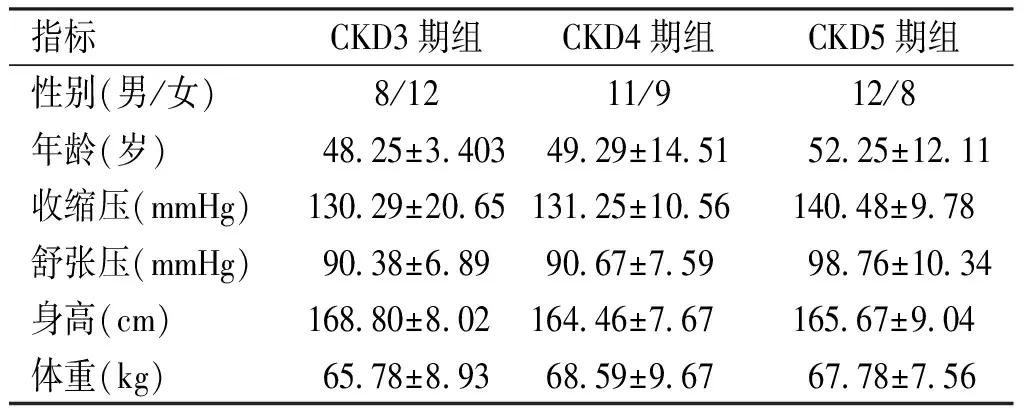
表1 3组CDK患者性别比、年龄、收缩压、 舒张压、身高、体重比较Tab.1 Comparison of sex ratio, age, systolic blood pressure, diastolic blood pressure, height and weight between the 3 groups of CDK patients
1.2 方法
1.2.1 心功能指标测定及LVM计算 采用西门子S2000彩色多普勒超声诊断仪行超声心动图检查,探头频率为2~4 MHz,测定患者EF、LVDd、LVDs、IVST及LVPTW,计算左室心肌重量指数(LVMI)[6-7]。LVMI=左室心肌重量(LVM)/体表面积(BSA),LVM=1.04×[(LVDd﹢IVST﹢LVPTW)3-LVDd3]-13.6,BSA=0.006 1×身高(cm)﹢0.012 8×体重(kg)-0.152 9;男性LVMI>125 g/m2,女性LVMI>110 g/m2诊断为左室肥厚。
1.2.2 血液学指标 3组患者均于入院时抽取清晨空腹静脉血测定血清Scr、BUN、Ca2+、P及iPTH水平和全血HGB及HCT采用西斯美康全自动生化分析仪测定血清Scr、BUN、Ca2+、P含量,贝克曼血细胞分析仪测定全血的HGB及HCT,电化学发光分析法测定血清iPTH水平。
1.3 统计学方法

2 结果
2.1 Scr、BUN、Ca2+、P及iPTH、HGB及HCT水平
3组CDK患者Scr、BUN、P及iPTH水平随CDK分期的增加而升高,Scr、BUN、及iPTH水平在3组患者间两两比较差异有统计学意义(P<0.05),CKD3期组、CKD4期组患者的血清P水平低于CKD5期,差异有统计学意义(P<0.05); Ca2+、HGB及HCT水平随CDK分期的增加而降低,仅在3~4期CKD组与CKD5期组比较差异有统计学意义(P<0.05)。见表2。
2.2 EF、LVDd、LVDs、IVST、LVPTW及LVMI
3组CDK患者EF随CDK分期的增加而降低,两两比较差异有统计学意义(P<0.05);LVDd、LVDs、IVST及LVPTW及LVMI随CDK分期的增加而升高,仅LVDd 及LVMI在3组间两两比较差异有统计学意义(P<0.05),CKD3期组、CKD4期组的LVDs、LVPTW及IVS与CKD5期比较,差异有统计学意义(P<0.05)。见表3。

表2 3组CKD患者Scr、BUN、Ca2+、P及iPTH、 HGB及HCT水平Tab.2 Scr, BUN, Ca2+, P, HGB, HCT and iPTH levels in 3 groups of patients with CKD
(1)与CKD3期组比较,P<0.05;(2)与CKD4期组比较,P<0.05

表3 3组CKD患者EF、LVDd、LVDs、IVST、 LVPTW及LVMI比较Tab.3 Comparison of EF, LVDd, LVDs, IVST, LVPTW and LVMI in 3 groups of patients with CKD
(1)与CKD3期组比较,P<0.05;(2)与CKD4期组比较,P<0.05
2.3Spearman相关分析
Spearman分析结果显示,患者血清Scr、BUN及P与LVMI呈正相关(r=0.638、0.600、0.499,P<0.01),HGB与LVMI和HCT呈负相关(r=-0.583、-0.598,P<0.01),血清Ca2+与LVMI无相关性(r=-0.347,P>0.01)。血清iPTH水平与LVDd、LVDs及LVMI呈正相关(r=0.642、0.548、0.577,P<0.01),与IVST、LVPTW无相关性(r=0.014、0.052,P>0.01),与EF呈负相关(r=-0.604,P<0.01)。
3 讨论
心血管疾病(CVD)是影响CKD患者预后的主要因素[1]。根据欧美国家文献统计,终末期肾脏病和接受肾移植患者的CVD死亡率占其总死亡率的40%~45%[8-9]。在我国也是致死的首要原因[10]。CKD患者高血压、小动脉硬化及主动脉硬化、细胞外液容量增加、贫血等均可增加患者左心室压力负荷这些因素长期相互作用,可使左心室心肌细胞发生肥大,临床上主要表现为左室肥厚(LVH)[2,11]。有研究发现PTH通过甲状旁腺素相关蛋白受体作用于心肌细胞而导致细胞内Ca离子浓度升高,激活蛋白激酶C,引起代谢异常及心肌肥大[12]。也有学者发现PTH可引起血管紧张素Ⅱ升高,诱导多种原癌基因在心肌细胞高表达,进而导致心肌细胞与间质细胞肥大、增生及纤维化[13]。
CKD早期患者CVD的发生率呈逐渐升高趋势[14]。本文研究发现,15%的CKD3期患者出现LVH,到CKD5期明显增多,LVH患者高达85%,与上述文献相符。本研究还发现所有CKD患者EF呈下降趋势,但CKD5期患者表现较为显著,CKD3-4期下降趋势不明显;随着CKD的进展,HGB、HCT逐渐降低、血P水平逐渐升高,CKD5期患者出现显著的贫血及高磷血症,CKD3期与CKD4期之间虽有变化,但差异无统计学意义,可能与本文研究样本量小、单中心等有关。现已证实,贫血、细胞外液容量增加、透析方式、蛋白尿、炎症与营养不良、氧化应激、高同型半胱氨酸血症、钙磷代谢紊乱及促凝血因子等是引起CVD的非传统危险因素[2]。本研究的结果还显示,Scr、BUN、P与LVMI呈正相关,HGB、HCT与LVMI呈负相关。与上述观点相符。同时,本研究iPTH与LVDd、LVDs、LVMI呈正相关,与EF呈负相关,提示iPTH可能是左室肥厚相关危险因素之一。
综上,CKD患者在CKD3期即可出现左室肥厚,iPTH水平与左室肥厚密切相关,是影响左室结构的重要因素之一,临床工作中应重视CKD早期非透析患者心脏指标的检测,积极寻找导致LVH的原因,同时检测iPTH水平,根据iPTH水平进行早期干预,积极调节钙磷代谢、纠正代谢性酸中毒及贫血等,避免继发性甲状旁腺功能亢进症(SHPT)的发生,预防CKD患者心血管并发症的发生,降低死亡率。
[1] 葛均波,徐永健.内科学[M].8版.北京:人民卫生出版社, 2014:524-525.
[2] 王海燕.肾脏病学[M].3版.北京:人民卫生出版社, 2008:1883.
[3] Cunningham J,Locatelli F,Rodriguez M,et al. secondary hyperparathyroidism:pathogenesis,disease progression,and therapeutic options[J]. Clin J Am Soc Nephrol, 2011 (4):913.
[4] Shackley BS,Nguyen TP,Shivkumar K,et al. Idiopathic massive myocardial calcification:a case report and review of the literature[J]. Cardiovasc Pathol, 2011(20):79-83.
[5] 全国eGFR课题协作组.MDRD方程在我国慢性肾脏病患者中的改良和评估[J].中华肾脏病杂志, 2006 (10):589-595.
[6] Devereux RB,Reichek N. Echocardiographic determination of left ventricular mass in man. Anatomic validation of the method[J]. Circulation, 1977 (4):613-618.
[7] Stevenson PH.Height-weight-surface formula for the estimation of surface area in Chinese subject[J].Chin j Physiol, 1937 (3):327-334.
[8] Investigators ET,Chertow GM,Block DA,et al.Effect of cinacalcet on cardiovascular disease in patients undergoing dialysis[J].N Engl J Med, 2012(367):2482-2494.
[9] Daimon M,Watanabe H,Abe Y,et al.Gender differences in age-related changes in left and right ventricular geometries and functions[J].Circ J, 2011(75):2840-2846.
[10]中华医学会肾脏病分会透析移植登记工作组.1999年度全国透析移植登记报告[J].中华肾脏病杂志, 2001(17):77-78.
[11]Hruska KA,Choi ET,Memon I,et al.Cardiovascular risk in chronic kidney disease(CKD):the CKD-mineral bone disorder (CKD-MBD)[J].Pediatr Nephrol, 2010(25):769-778.
[12]朱潮涌,张萍,陈江华.甲状旁腺激素对维持性血液透析患者心肌损伤及心脏结构与功能的影响[J].全科医学临床与教育, 2010 (8):628-631.
[13]Freeman J,Dodd JD,Ridge CA,et al.“Porcelain heart”cardiomyopathy secondary to hyperparathyroidism:radiographic,echocardiographic and cardiac CT appearances[J].J Cardiovasc Comput Tomogr, 2010(4):402-404.
[14]Hassan KI,Hassan S,Anwar S,et al. Predictors of left ventricular hypertrophy and their cutoffs in peritoneal dialysis patients[J].Int Heart, 2015 (2):186-191.
(2016-11-01收稿,2016-12-03修回)
中文编辑: 吴昌学; 英文编辑: 刘 华
Correlation between Serum Parathyroid Hormone and Left Ventricular Hypertrophy in Patients with Stage 3~5 Chronic Kidney Disease
CHANG Huan1, GAO Xiaofang1, ZHANG Yapu1, CHEN Hang2, GUO Li2, LI Jiandong2
(1.HebeiUniversity,Baoding071000,Hebei,China; 2.DepartmentofNephrology,theAffiliatedHospitalofHebeiUniversity,Baoding071000,Hebei,China)
Objective: To investigate the correlation between serum parathyroid hormone and left ventricular hypertrophy in patients with chronic kidney disease stage 3~5. Methods: 60 cases of patients with CKD who didn't undergo hemodialysis in first diagnosis were divided into A, B, and C group according to pathological stage 3, 4 and 5, respectively. Echocardiography was used to measure ejection fraction (EF), left ventricular end diastolic diameter (LVDd), left ventricular end systolic diameter (LVDs), interventricular septal thickness (IVST) and left ventricular posterior wall thickness (LVPTW), and the left ventricular mass index (LVMI) was calculated. Patients' fasting venous blood was collected in admission to hospital. The automatic biochemical analyzer was adopted to detect serum creatinine(Scr), urea nitrogen (BUN), calcium (Ca2+) concentration and phosphorus(P) concentration. The blood cell analyzer was adopted to detect hemoglobin(HGB), hematocrit (HCT) and optical analysis of electrochemistry was adopted to detect serum iPTH level. Spearman was used to analyze the correlation between hematological parameters and LVMI, serum iPTH and cardiac function indexes. Results: The Scr, BUN, serum P, iPTH, LVDd, LVDs, IVST, LVPTW and LVMI increased with CDK staging increased while serum calcium (Ca2+) HGB, HCT and EF decreased with CDK staging increased in the three groups. There were statistically significant differences in Scr, BUN, iPTH, LVDd, LVMI and EF between the three groups (P<0.05). There were statistically significant differences in serum P, serum Ca2+, HGB, HCT, LVDS, LVPTW and IVST between and CKD 3~4 stage and CKD stage 5 (P<0.05). Spearman results showed that Scr, BUN and P were positively correlated with LVMI (r=0.638, 0.600, 0.499,P<0.01), HGB was negatively correlated with LVMI and HCT (r=-0.583,-0.598,P<0.01), and there was no correlation between serum Ca2+and LVMI (r=-0.347,P>0.01). Serum iPTH levels were positively correlated with LVMI, LVDd and LVDs (r=0.642, 0.548, 0.577,P<0.01), not correlated with IVST, LVPTW (r=0.014, 0.052,P>0.01), and negatively correlated with EF(r=-0.604 ,P<0.01). Conclusion: Left ventricular hypertrophy may occur in patients with CKD stage 3~5, and the iPTH level may be an important factor affecting the left ventricular structure.
chronic kidney disease; parathyroid hormone; left ventricular hypertrophy; cardiac ponderal index; secondary hyperparathyroidism
时间:2016-12-15
http://www.cnki.net/kcms/detail/52.1164.R.20161215.1534.023.html
R692.5
A
1000-2707(2016)12-1478-04
10.19367/j.cnki.1000-2707.2016.12.026
*通信作者 E-mail:chenhang65@sina.com
