肝动脉化疗栓塞治疗乙型肝炎相关性肝癌的预后影响
2017-01-06汪艳陈乐
汪艳,陈乐
(黄冈市中心医院感染科,湖北 黄冈 438000)
肝动脉化疗栓塞治疗乙型肝炎相关性肝癌的预后影响
汪艳,陈乐
(黄冈市中心医院感染科,湖北 黄冈 438000)
目的 探讨肝动脉化疗栓塞治疗乙型肝炎相关性肝癌的预后影响因素。方法 对行肝动脉化疗栓塞治疗的150例患者临床资料进行回顾性分析,观察肝动脉化疗栓塞治疗3年后患者生存率,并对肝动脉化疗栓塞治疗乙型肝炎相关性肝癌的预后影响因素采用单因素分析及Logistic多因素分析。 结果 (1)150例乙型肝炎相关性肝癌患者经肝动脉化疗栓塞治疗3年后,存活64例,死亡86例, 3年生存率为42.67%,死亡率为57.33%。(2)单因素分析得出:假包膜形成、癌灶数目多、门脉癌栓、肿瘤直径大、胸腔转移、腹腔转移均为肝动脉化疗栓塞治疗乙型肝炎相关性肝癌的危险因素为肝动脉化疗栓塞治疗乙型肝炎相关性肝癌的保护因素,均差异有统计学意义(P<0.05)。(3)经Logistic多因素回归分析得出:假包膜形成、癌灶多发、门脉癌栓、肿瘤直径≥5 cm、胸腔转移、腹腔转移均为肝动脉化疗栓塞治疗乙型肝炎相关性肝癌的危险因素。结论 假包膜形成、癌灶多发、门脉癌栓、肿瘤直径≥5 cm、胸腔转移、腹腔转移均为肝动脉化疗栓塞治疗乙型肝炎相关性肝癌的危险因素。
乙型肝炎相关性肝癌;肝动脉化疗栓塞治疗;危险因素
乙型肝炎相关性肝癌病情进展迅速,但起病具有隐匿性,因此一旦确诊绝大多数患者已出现胸腹部等远处转移情况,从而使得无法手术治疗,失去最佳治疗时机,预后差[1]。目前,乙型肝炎相关性肝癌的主要治疗方法为肝动脉化疗栓塞,已被临床广泛应用[2]。近年来,如何更好的治疗乙型肝炎相关性肝癌已逐渐成为临床医生研究的热点[3]。为此笔者回顾性分析行肝动脉化疗栓塞治疗的150例患者临床资料,现将结果报告如下。
1 资料与方法
1.1 临床资料 回顾性分析2010年2月至2012年10月在黄冈市中心医院进行肝动脉化疗栓塞治疗的150例患者临床资料,其中男性83例,女性67例;年龄16~81岁,平均(46.97±11.22)岁;其中癌灶单发者99例,癌灶多发者51例;假包膜形成者54例,无假包膜形成者96例;存在门脉癌栓者39例,未见门脉癌栓者111例。本研究获得黄冈市中心医院伦理委员会批准,患者或近亲属签署了知情同意书。
1.2 方法
1.2.1 肝动脉化疗栓塞治疗 选择Seldinger 技术进行肝肠系膜上动脉与总动脉常规造影术,观察门静脉充盈状态及肝脏内部肿瘤供血状况。采用夹心式进行局部化疗栓塞,注入羟基喜树碱、氟脲嘧啶、丝裂霉素、表阿霉素及顺铂等药物。药物剂量根据肝功能情况、肿瘤分布及肿瘤大小而定。
1.2.2 随访 全部患者均建立详细的资料档案,出院后通过电话、邮件、登门等方式定时进行随访。
1.3 观察指标 (1)观察肝动脉化疗栓塞治疗3年后患者生存率;(2)单因素分析肝动脉化疗栓塞治疗乙型肝炎相关性肝癌的预后相关因素,其中包括年龄、性别、假包膜形成、癌灶数目、门脉癌栓、肿瘤大小、胸腔转移、腹腔转移及化疗次数;(3)经Logistic多因素回归分析肝动脉化疗栓塞治疗乙型肝炎相关性肝癌的预后相关因素。

2 结果
2.1 肝动脉化疗栓塞治疗3年后患者生存率 150例乙型肝炎相关性肝癌患者经肝动脉化疗栓塞治疗3年后,存活64例,死亡86例, 3年生存率为42.67%,死亡率为57.33%。
2.2 单因素分析肝动脉化疗栓塞治疗乙型肝炎相关性肝癌的预后相关因素 单因素分析得出:假包膜形成、癌灶数目多、门脉癌栓、肿瘤直径大、胸腔转移、腹腔转移均为肝动脉化疗栓塞治疗乙型肝炎相关性肝癌的危险因素(P<0.05),见表1。

表1 单因素分析肝动脉化疗栓塞治疗乙型肝炎相关性肝癌的预后相关因素/例
2.3 Logistic多因素分析肝动脉化疗栓塞治疗乙型肝炎相关性肝癌的预后相关因素 经Logistic多因素回归分析得出:假包膜形成、癌灶多发、门脉癌栓、肿瘤直径≥5 cm、胸腔转移、腹腔转移均为肝动脉化疗栓塞治疗乙型肝炎相关性肝癌的危险因素,见表2。
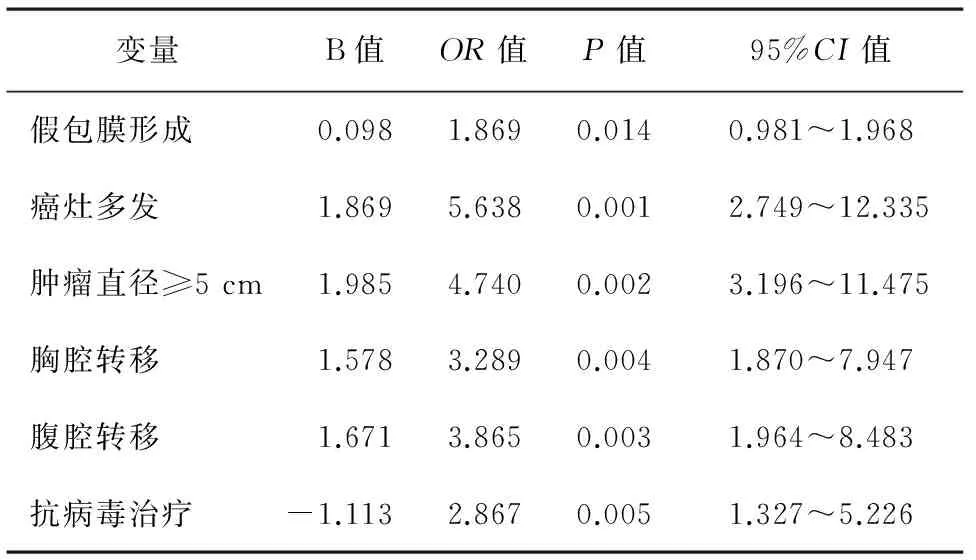
表2 Logistic多因素分析肝动脉化疗栓塞治疗乙型肝炎相关性肝癌的预后相关因素
3 讨论
原发性肝癌属于我国临床上常见的恶性肿瘤,该病进展迅速,起病隐匿,一旦确诊绝大多数患者已出现远处转移,从而失去手术最佳治疗时机[4-9]。目前,作为不能进行手术切除以及手术复发者,肝动脉化疗栓塞治疗能否有效改善乙型肝炎相关性肝癌患者的预后仍存在争议[10]。有相关研究[11-13]显示,进行肝动脉化疗栓塞治疗的乙型肝炎相关性肝癌患者的中位生存时间明显高于保守治疗患者。但亦有相关研究[14]显示,虽然肝动脉化疗栓塞治疗能够抑制肿瘤生长,但对于提高患者生存率未见显著效果。本研究结果显示,150例乙型肝炎相关性肝癌患者经肝动脉化疗栓塞治疗3年后,存活64例,死亡86例, 3年生存率为42.67%,死亡率为57.33%。
经本研究结果显示并总结肝动脉化疗栓塞治疗乙型肝炎相关性肝癌的预后影响因素,具体如下:(1)假包膜形成:假包膜形成者的3年生存率为24.07%,显著低于未见假包膜形成者的53.13%,差异有统计学意义(P<0.05),此结果表明,存在假包膜不利于肝动脉化疗栓塞治疗乙型肝炎相关性肝癌的预后;(2)癌灶数目:通过对比癌灶单发与多发情况得出,癌灶多发者3年生存率为21.57%,显著低于癌灶单发者的53.54%,比较差异有统计学意义(P<0.05),癌灶多发严重影响乙型肝炎相关性肝癌的预后;(3)肿瘤直径:肿瘤越大,肝动脉化疗栓塞治疗的预后越差,乙型肝炎相关性肝癌的3年生存率越低;(4)胸腹腔转移:若出现胸腔或腹腔转移,肿瘤则更难控制,严重治疗预后,生存率显著降低。
综上所述,假包膜形成、癌灶多发、门脉癌栓、肿瘤直径≥5 cm、胸腔转移、腹腔转移均为肝动脉化疗栓塞治疗乙型肝炎相关性肝癌的危险因素。
[1] Zhou ZG,Zheng XR,Zhou Q,et al.Impact of oral anti-hepatitis B therapy on the survival of patients with hepatocellular carcinoma initially treated with chemoembolization[J].Cancer,2015,33(5):205-216.
[2] Chen XH,Heng B.Risk factors for residual tumor after resection of hepatocellular carcinoma[J].World Journal of Gastroenterology,2011,17(14):1889-1894.
[3] Lance C,McLennan G,Obuchowski N,et al.Comparative analysis of the safety and efficacy of transcatheter arterial chemoembolization and yttrium-90 radioembolization in patients with unresectable hepatocellular carcinoma[J].JVIR,2011,22(12):1697-1705.
[4] Group KL.2014 Korean Liver Cancer Study Group-National Cancer Center Korea Practice Guideline for the Management of Hepatocellular Carcinoma[J].Korean Journal of Radiology,2015,16(3):465-522.
[5] Toyoda H,Kumada T,Tada T,et al.Transarterial chemoembolization for hepatitis B virus-associated hepatocellular carcinoma:improved survival after concomitant treatment with nucleoside analogues[J].J Vasc Interv Radiol,2012,23(3):317-322.
[6] 蔡轶伦,张庆红,姚咏明.肝癌患者术后手术部位感染的危险因素分析[J].中华医院感染学杂志,2013,23(23):5724-5726.
[7] Yan Q,Ni J,Zhang GL,et al.Efficacy of postoperative antiviral combined transcatheter arterial chemoembolization therapy in prevention of hepatitis B-related hepatocellular carcinoma recurrence[J].Chinese Medical Journal,2013,126(5):855-859.
[8] Nishikawa H,Osaki Y,Inuzuka T.Branched-chain amino acid treatment before transcatheter arterial chemoembolization for hepatocellular carcinoma[J].World Journal of Gastroenterology,2012,18(12):56-59.
[9] Jiang JH,Guo Z,Lu HF,et al.Adjuvant transarterial chemoembolization after curative resection of hepatocellular carcinoma:Propensity score analysis[J].World Journal of Gastroenterology Wjg,2015,21(15):4627-4634.
[10] Chau GY.Resection of hepatitis B virus-related hepatocellular carcinoma:Evolving strategies and emerging therapies to improve outcome[J].World Journal of Gastroenterology,2014,20(35):12473-12484.
[11] Yu SJ,Kim YJ.Hepatitis B viral load affects prognosis of hepatocellular carcinoma[J].World J Gastroenterol,2014,20(34):12039-12044.
[12] Lao,XM,Luo G,Ye LT,et al.Effects of antiviral therapy on hepatitis B virus reactivation and liver function after resection or chemoembolization for hepatocellular carcinoma[J].Liver International,2013,33(4):595-604.
[13] Hai Q,Wang J.Liver resection in hepatitis B related-hepatocellular carcinoma:Clinical outcomes and safety in elderly patients[J].World Journal of Gastroenterology,2014,20(21):6620-6625.
[14] Zhiping H,Peng Z,Haiqing W,et al.Comparing outcomes of two vascular inflow occlusion techniques and treatment without vascular occlusion during major hepatectomy in patients with Hepatitis B-related hepatocellular carcinoma[J].Plos One,2014,9(9):e107303.
Prognostic impact of transcatheter arterial chemoembolization in the treatment of hepatitis B associated hepatocellular carcinoma
WANG Yan,CHEN Le
(DepartmentofInfectiousDiseases,HuanggangCentralHospital,Huanggang,Hubei438000,China)
Objective To investigate the prognostic factors of hepatic artery chemoembolization in the treatment of hepatitis B associated hepatocellular carcinoma.Methods Clinical data of 150 cases undergoing hepatic artery chemotherapy embolization were retrospectively analyzed.Three-year survival rate of the patients was observed,and prognostic influence factors were analyzed using single factor analysis and Logistic multivariate regression analysis.Results Three years after the treatment,of 150 cases of HBV related hepatocellular carcinoma patients,64(42.67%)cases survived,and 86(57.33%)cases died.The single factor analysis showed that pseudocapsule formation,tumor number,tumor thrombus in the portal vein,diameter of tumor,pleural and peritoneal metastases were risk factors of hepatic artery chemoembolization in the treatment of hepatitis B virus associated hepatocellular carcinoma.The differences were statistically significant(P<0.05).The Logistic multivariate regression analysis showed that pseudocapsule formation,cancer lesions,portal vein tumor thrombus,tumor diameter greater than 5 cm,pleural and peritoneal metastases were risk factors of hepatic arterial chemoembolization in the treatment of hepatitis B virus associated hepatocellular carcinoma.Conclusions Formation of pseudocapsule,multiple tumor,portal vein tumor thrombus,tumor diameter greater than or equal to 5 cm,pleural metastasis,and peritoneal metastasis are risk factors of transcatheter arterial chemoembolization in the treatment of hepatitis B virus related hepatocellular carcinoma(HCC).
Hepatitis B related hepatocellular carcinoma;Transcatheter arterial chemoembolization;Risk factor
10.3969/j.issn.1009-6469.2016.11.046
2016-04-12,
2016-08-23)