Lp-PLA2表达差异程度是否可作为脑卒中患者颈动脉内膜剥脱术围手术期风险的标志物评估
2016-12-09刘晓佳伍健明张协军张秋生黄贤键
刘晓佳 伍健明 张 猛 何 毅 张协军 张秋生 黄贤键
广东深圳市第二人民医院神经外科 深圳 518035
Liu Xiaojia,Wu Jianming,Zhang Meng,He Yi,Zhang Xiejun,Zhang Qiusheng,Huang Xianjian
Departmentof Neurosurgery,Shenzhen Second People’s Hospital,Shenzhen 518035,China
Lp-PLA2表达差异程度是否可作为脑卒中患者颈动脉内膜剥脱术围手术期风险的标志物评估
刘晓佳 伍健明△张 猛 何 毅 张协军 张秋生 黄贤键
广东深圳市第二人民医院神经外科 深圳 518035
目的 分析脑卒中患者颈动脉内膜剥脱术(CEA)前后血浆Lp-PLA2水平变化,并评估Lp-PLA2表达差异程度与围手术期并发症风险的关系。方法 选取CEA治疗的脑卒中患者44例,检测术前1周和术后4周Lp-PLA2蛋白的表达水平,并进行2 a随访,统计围手术期并发症和脑卒中、血管再狭窄等复发情况。结果 对缺血性脑卒中的相关危险因素进行Logistic回归分析,结果显示,以缺血性脑卒中是否发病为应变量,相关危险因素,如年龄、性别、吸烟史、高血压、糖尿病、Lp-PLA2为自变量,得到多元回归方程:缺血性脑卒中=-2.361+0.796吸烟+0.005 Lp-PLA2。由此得出,Lp-PLA2是缺血性脑卒中的危险因素(P<0.05)。术前1周和术后4周Lp-PLA2蛋白表达水平显示,其中表达差异大31例,表达差异小13例,并进行2 a随访。最终发现,表达差异程度大患者出现脑卒中(P<0.05)和再狭窄(P<0.05)的几率明显降低。结论 Lp-PLA2是缺血性脑卒中的独立预测因子,且Lp-PLA2表达水平差异可作为脑卒中患者开展CEA围手术期风险预测标志物。
颈动脉内膜剥脱术;Lp-PLA2;脑梗死
LiuXiaojia,WuJianming,ZhangMeng,HeYi,ZhangXiejun,ZhangQiusheng,HuangXianjian
DepartmentofNeurosurgery,ShenzhenSecondPeople’sHospital,Shenzhen518035,China
颈动脉内膜切除术(CEA)[1-3]和近年来发展的颈动脉支架成形术(CAS)[4-7]是目前治疗的颈动脉狭窄的标准手术。CEA可明显降低有缺血症状且颈动脉狭窄程度超过50%患者脑卒中的发生率。本研究利用卒中筛查的人群优势以及已熟练开展的CEA手术,结合血清学检测Lp-PLA2水平及完善的临床资料收集(术前和围手术期等),进而评估手术前后Lp-PLA2表达水平差异程度是否可作为围手术期和远期复发风险评估的标志物。
1 对象与方法
1.1 病例选择 研究共纳入44例脑卒中患者,病理诊断符合1995年全国第4届脑血管疾病学术会议修订脑梗死诊断标准。所有患者均经神经系统及MRI等检查确认。除外椎基底动脉系统的脑梗死、动脉炎、先天发育异常、糖尿病性、血液成分及血液流变学所致的脑梗死以及合并冠心病和外周血管病等患者。男23例,女21例;年龄(59.21±8.72)岁;高血压38例(86.36%),糖尿病11例(25.00%),吸烟史19例(43.18%);Lp-PLA2(27.6±8.52)mmol/L。
1.2 超声复查 先作横向探测,将B超探头置于颈根部并向头侧方向移动:(1)需要测量血管的内径;(2)识别膨大部位、颈内和颈外动脉所在具体位置;(3)监测CCA、ICA和ECA管壁四周所处部位;接着,取颈前侧位再作纵向探测,从颈根部沿着颈总动脉血管的长轴作纵向扫查并越过膨大的部分,显示颈内和颈外动脉的长轴:(1)测量内膜中层的厚度;(2)测量斑块长度和厚度,并观察其表面和内部的特性;(3)用CDFI显示血管内血流的方向、血管充盈情况和狭窄及阻塞的部位;(4)行脉冲多普勒检查,观察血流流速曲线,并行参数测定。
1.3 血浆Lp-PLA2水平的测定 于术前1周和术后4周空腹采血4 mL,作抗凝处理,标本采集后25 min内于2~8 ℃情况下1 000×g离心15 min,分离上血清液,置于Ep管内,统一编号并保存于-80 ℃条件下。利用免疫增强比浊法测定血浆中Lp-PLA2含量,具体操作流程按试剂盒说明书进行。全部标本均一次性成批检测,以减小批间差和测量误差等。并进行随访,统计围手术期和2 a长期并发症。
1.4 统计学方法 采用SPSS 19.0统计软件处理数据。计数资料采用χ2检验,双侧α=0.05,P<0.05为差异有统计学意义。
2 结果
2.1 术前MRI和术后切下组织 如图1所示。
2.2 缺血性脑卒中相关危险因素的Logistic回归分析 对缺血性脑卒中的相关危险因素进行Logistic回归分析,结果显示,以缺血性脑卒中是否发病作为应变量,相关危险因素,如年龄、性别、吸烟史、高血压、糖尿病、Lp-PLA2为白变量,得到多元回归方程:缺血性脑卒中=-2.361+0.796吸烟+0.005 Lp-PLA2。由此得出,Lp-PLA2是缺血性脑卒中的危险因素(P<0.05)。见表1。

图1 A:动脉管壁MRI增强扫描显示左侧颈内动脉起始部狭窄99%(箭头所示);B:CEA手术切除的颈动脉斑块

表1 缺血性脑卒中相关危险因素的Logistic回归分析
2.3 CEA手术前后Lp-PLA2蛋白表达水平差异程度与围手术期并发症的关系 术前1周和术后4周Lp-PLA2蛋白表达水平,其中表达差异大31例,表达差异小13例,随访2 a示,其中围手术期和长期并发症主要包括血肿、脑卒中、心梗、血栓形成、高灌注综合征、神经损伤、喉头水肿和再狭窄。表达差异程度大患者出现脑卒中(P<0.05)和再狭窄(P<0.05)的几率明显降低。见表2。
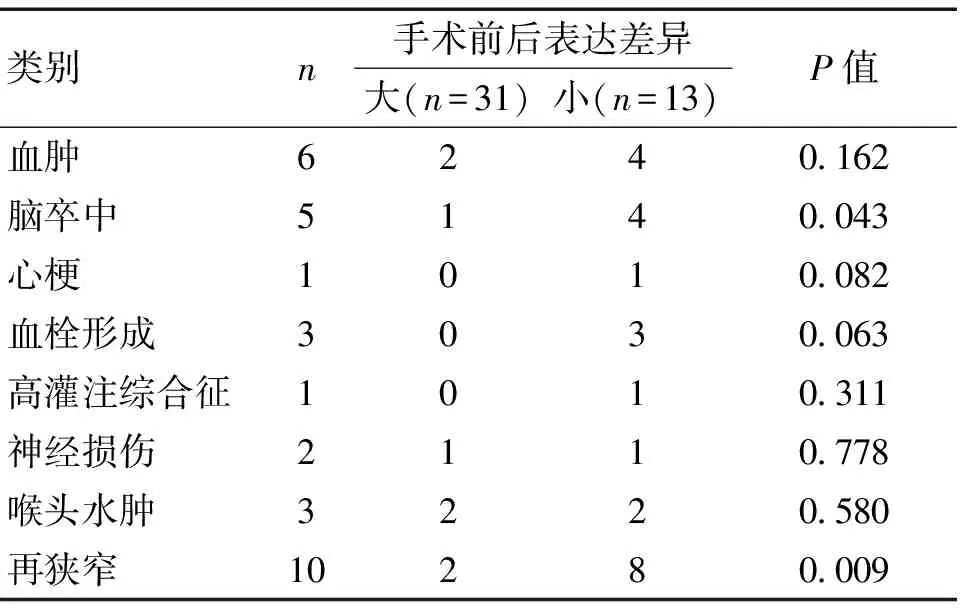
表2 CEA手术前后Lp-PLA2蛋白表达水平差异程度与围手术期并发症的关系
3 讨论
缺血性脑卒中(ischemic strokes,IS)是指因脑部血液循环障碍,脑实质缺血、缺氧所致的局限性脑组织缺血性坏死或软化,具有高发病率、高复发率和高致残率等特征[8-9]。新近研究发现,Lp-PLA2作为磷脂酶A2超家族的成员,是一种由441个氨基酸组成的分子量为45 kD的蛋白质,该蛋白参与斑块破裂以及动脉血栓形成等诸多过程,目前已被确认为预测缺血性脑卒中风险及预后的敏感标志物[10]。
CEA和CAS是目前治疗的颈动脉狭窄的标准手术[11-12]。循证医学研究证据表明,CEA可明显降低有缺血症状(即短暂性脑缺血发作、卒中)且颈动脉狭窄≥50%病人脑卒中的发生率[13-14]。但对中重度颈动脉狭窄(狭窄≥50%)无症状患者而言,是否采取手术治疗目前仍有较大争议[15]。如果此部分患者颈动脉斑块不稳定,发生卒中的风险很高,是手术干预的重要指征[16-17]。但现有的检测手段包括超声、CT、MRI、血管造影以及血清学检测,难以准确判断颈动脉斑块的稳定性[18],从而给临床治疗方式的选择带来很大困难[19]。因此,迫切需要寻找新的诊断标识评估颈动脉斑块的稳定性。
本研究结果提示,Lp-PLA2是缺血性脑卒中的危险因素(P<0.05)。此外,表达差异程度大患者,出现脑卒中和再狭窄的几率明显降低。在彻底切除斑块后,Lp-PLA2表达水平可降至最低水平,反之,降低水平不大,复发的可能性也就增加。
在一项临床试验(NASCET)中,研究人员对500例病人的术前血管影像学检测结果与术后斑块组织病理分析结果作了详细比较发现,血管影像学检出不稳定斑块定的灵敏度只有45.9%,特异性74.0%,总体阳性预测价值71%。由此可见,现有手段对不稳定斑块的检出率不到50%,假阳性率高达30%。这对临床治疗方式的选择(手术或药物治疗)带来很大困难,大大降低了颈动脉斑块筛查预防卒中发生的效率。
综上,Lp-PLA2是缺血性脑卒中的独立危险因素,且CEA前后血浆Lp-PLA2变化差异程度可作为脑卒中和血管再狭窄预测的潜在标志物。
[1] Kuzhuget RA,Karpenko AA,Kamenskaya OV,et al.Ways to improve immediate and remote results of carotid endarterectomy[J].Angiol Sosud Khir,2016,22(1):111-117.
[2] Merckelbach S,Leunissen T,Vrijenhoek J,et al.Clinical Risk Factors and Plaque Characteristics Associated with New Development of Contralateral Stenosis in Patients Undergoing Carotid Endarterectomy[J].Cerebrovasc Dis,2016,42(1/2):122-130.
[3] Mitsuoka H.Carotid Endarterectomy Using Intraluminal Double Baloon Shunt[J].Nihon Geka Gakkai Zasshi,2016,117(1):58-59.
[4] Moore WS,Popma JJ,Roubin GS,et al.Carotid angiographic characteristics in the CREST trial were major contributors to periprocedural stroke and death differences between carotid artery stenting and carotid endarterectomy[J].J Vasc Surg,2016,63(4):851-857;858.e1.
[5] Spacek M,Stechovsky C,Horvath M,et al.Evaluation of cerebrovascular reserve in patients undergoing carotid artery stenting and its usefulness in predicting significant hemodynamic changes during temporary carotid occlusion[J].Physiol Res,2016,65(1):71-79.
[6] Imahori T,Hosoda K,Fujita A,et al.Long-Term Outcomes of Carotid Endarterectomy and Carotid Artery Stenting for Carotid Artery Stenosis:Real-World Status in Japan[J].J Stroke Cerebrovasc Dis,2016,25(2):360-367.
[7] Gonzalez A,Moniche F,Cayuela A,et al.Effect of CYP2C19 Polymorphisms on the Platelet Response to Clopidogrel and Influence on the Effect of High Versus Standard Dose Clopidogrel in Carotid Artery Stenting[J].Eur J Vasc Endovasc Surg,2016,51(2):175-186.
[8] Artoni A,Bucciarelli P,Martinelli I.Cerebral Thrombosis and Myeloproliferative Neoplasms[J].Curr Neurol Neurosci Rep,2014,14(11):496-496.
[9] Bousser MG,Crassard I.Cerebral venous thrombosis,pregnancy and oral contraceptives[J].Thromb Res,2012,130(Suppl 1):S19-S22.
[10] Aitoufella H,Mallat Z,Tedgui A.Lp-PLA2 and sPLA2:cardiovascular biomarkers[J].Med Sci,2014,30(5):526-531.
[11] Yamashiro S,Arakaki R,Kise Y,et al.Emergency operation for aortic dissection with ischemic stroke[J].Asian Cardiovasc Thorac Ann,2014,22(2):208-211.
[12] Yu SC,Zou WX,Soo YO,et al.Evaluation of Carotid Angioplasty and Stenting for Radiation-Induced Carotid Stenosis[J].Stroke,2014,45(5):1 402-1 407.
[13] Endarterectomy for asymptomatic carotid artery stenosis.Executive Committee for the Asymptomatic Carotid Atherosclerosis Study[J].JAMA,1995,273(18):1 421-1 428.
[14] Halliday A,Mansfield A,Marro J,et al.Prevention of disabling and fatal strokes by successful carotid endarterectomy in patients without recent neurological symptoms:randomised controlled trial[J].Lancet,2004,363(9420):1 491-1 502.
[15] Dharmarajah B,Thapar A,Salem J,et al.Impact of risk scoring on decision-making in symptomatic moderate carotid atherosclerosis[J].Br J Surg,2014,101(5):475-480.
[16] van Lammeren GW,den Ruijter HM,Vrijenhoek JE,et al.Time Dependent Changes in Atherosclerotic Plaque Composition in Patients Undergoing Carotid Surgery[J].Circulation,2014,129(22):2 269-2 276.
[17] Noyes AM,Thompson PD.A systematic review of the time course of atherosclerotic plaque regression[J].Atherosclerosis,2014,234(1):75-84.
[18] Jin XQ,Wu XW,Lu ZQ,et al.The stability of the atherosclerotic plaque depends on the extent of injured endothelium:results from a novel model of ischemia/reperfusion induced atherosclerosis in carotid artery of rats[J].Zhonghua Xin Xue Guan Bing Za Zhi,2013,41(12):1 040-1 044.
[19] Toklueva LR,Balakhonova TV,Strazden E,et al.Possibilities of instrumental methods of diagnosis of unstable atherosclerotic plaques of carotid arteries[J].Angiol Sosud Khir,2013,19(3):37-44.
(收稿2016-06-23)
Evaluation of whether the degree of Lp-PLA2 expression differences can be used as the biomarker for predicting the perioperative risks during CEA for cerebral apoplexy patients
Objective To analyze the Lp-PLA2 expression difference before and after carotid endarterectomy(CEA),and evaluate the association between the degree of expression differences and risk of perioperative complications.Methods These patients who were diagnosed as cerebral apoplexy and adopted CEA surgery,were enrolled in the present cohort.The Lp-PLA2 expression was examined one week before and four weeks after surgery.In addition,the two years follow-up was also conducted,and the complications during perioperative period,cerebral apoplexy and vascular restenosis during the two years follow-up were also recorded.Results A total of 44 patients were enrolled,and the Logistic regression test was performed,by which the cerebral arterial thrombosis was treated as dependent variant and the related risk factors,such as age,sex,smoking status,hypertension,diabetes and Lp-PLA2 were regarded as independent variable,the multiple regression equation was demonstrated as:cerebral arterial thrombosis=-2.361+0.796 smoking status+0.005 Lp-PLA2.Therefore,we can conclude that the Lp-PLA2 was a risk factor for cerebral arterial thrombosis(P<0.05).In addition,we also recorded the Lp-PLA2 expression levels one week before surgery and four weeks after surgery,and identified that a total of 31 cases were of high variability,while 13 cases were of lower variability.After two years’ follow-up,we revealed that these patients with high variability of Lp-PLA2 expression were of significant lower risk to get cerebral apoplexy and restenosis(P<0.05).Conclusion Lp-PLA2 is an independent risk factor for cerebral arterial thrombosis,and the degree of expression differences can be used to predict the risk of perioperative risk during CEA.
Carotid endarterectomy;Lp-PLA2;Cerebral infarction
深圳市科技计划项目(JCYJ20140414170821291)
R743.33
A
1673-5110(2016)23-0011-03
△通讯作者:伍建明,主任医师,E-mail:wujianmingsz@163.com
