Effects of Tai Ji Quan training on gait kinematics in older Chinese women with knee osteoarthritis:A randomized controlled trial
2016-10-24QinggungZhuLingynHungXieWuLinWngYunyZhngMinFngYuLiuJingXinLi
Qinggung Zhu,Lingyn Hung,Xie Wu,Lin Wng,Yuny Zhng,Min Fng,Yu Liu,*,Jing Xin Li,c,*
aKey Laboratory of Exercise and Health Sciences of Ministry of Education,Shanghai University of Sport,Shanghai 200438,China
bDepartment of Physical Therapy with Chinese Massage,Yueyang Hospital of Integrated Traditional Chinese and Western Medicine,Shanghai University of Traditional Chinese Medicine,Shanghai 200437,China
cSchool of Human Kinetics,Faculty of Health Sciences,University of Ottawa,Ottawa K1N 6N5,Canada
Effects of Tai Ji Quan training on gait kinematics in older Chinese women with knee osteoarthritis:A randomized controlled trial
Qingguang Zhua,b,†,Lingyan Huanga,†,Xie Wua,Lin Wanga,Yunya Zhanga,Min Fangb,Yu Liua,*,Jing Xian Lia,c,*
aKey Laboratory of Exercise and Health Sciences of Ministry of Education,Shanghai University of Sport,Shanghai 200438,China
bDepartment of Physical Therapy with Chinese Massage,Yueyang Hospital of Integrated Traditional Chinese and Western Medicine,Shanghai University of Traditional Chinese Medicine,Shanghai 200437,China
cSchool of Human Kinetics,Faculty of Health Sciences,University of Ottawa,Ottawa K1N 6N5,Canada
Background:Although Tai Ji Quan has been shown to relieve pain and improve functional mobility in people with knee osteoarthritis(OA),little is known about its potential benefits on gait characteristics among older Chinese women who have a high prevalence of both radiographic and symptomatic knee OA.This study aims to assess the efficacy of a tailored Tai Ji Quan intervention on gait kinematics for older Chinese women with knee OA.
Methods:A randomized controlled trial involving 46 older women in Shanghai,China,with clinically diagnosed knee OA.Randomized(1:1)participants received either a 60 minTai Ji Quan session(n=23)3 times weekly or a 60 min bi-weekly educational session(n=23)for 24 weeks. Primary outcomes were changes in gait kinematic measures from baseline to 24 weeks.Secondary outcomes included changes in scores on the Western Ontario and McMaster University Osteoarthritis Index(WOMAC)and Short Physical Performance Battery(SPPB).
Results:After 24 weeks theTai Ji Quan group demonstrated better performance in gait velocity(mean difference,8.40 cm/s,p=0.01),step length(mean difference,3.52 cm,p=0.004),initial contact angle(mean difference,2.19°,p=0.01),and maximal angle(mean difference,2.61°,p=0.003)of flexed knees during stance phase compared to the control group.In addition,the Tai Ji Quan group showed significant improvement in WOMAC scores(p<0.01)(mean difference,-4.22 points in pain,p=0.002;-2.41 points in stiffness,p<0.001;-11.04 points in physical function,p=0.006)and SPPB scores(mean difference,1.22 points,p<0.001).
Conclusion:Among older Chinese women with knee OA,a tailored Tai Ji Quan intervention improved gait outcomes.The intervention also improved overall function as indexed by the WOMAC and SPPB.These results support the use of Tai Ji Quan for older Chinese adults with knee OA to both improve their functional mobility and reduce pain symptomatology.
©2016 Production and hosting by Elsevier B.V.on behalf of Shanghai University of Sport.This is an open access article under the CC BY-NC-ND license(http://creativecommons.org/licenses/by-nc-nd/4.0/).
Gait;Pain;Physical function;Rheumatic diseases;Tai Chi Quan
1.Introduction
The incidence of knee osteoarthritis(OA),an articular pathology,increases with age,1with older adults being the most frequently affected.In China,epidemiological studies have shown a high prevalence of knee OA among middle-aged and older Chinese.2-5For example,a cross-sectional study in Beijing indicated that 15%of women and 5.6%of men aged 60 years and over had symptomatic knee OA.2The study further showed that when compared with Caucasian women of the same age living in the US(i.e.,from Framingham,MA),older women in Beijing had a roughly 50%higher prevalence of both radiographic and symptomatic knee OA and a twofold higher prevalence of bilateral cases.2,3From a global public health perspective,knee OA is considered a major cause of chronic disability,particularly for older adults who often experience deterioration in physical function,thereby impacting their quality of life and requiring medical treatments that add significant costs to the healthcare system.6,7
Peer review under responsibility of Shanghai University of Sport.
†These two authors contributed equally to this work.
http://dx.doi.org/10.1016/j.jshs.2016.02.003
2095-2546/©2016 Production and hosting by Elsevier B.V.on behalf of Shanghai University of Sport.This is an open access article under the CC BY-NC-ND license(http://creativecommons.org/licenses/by-nc-nd/4.0/).
Exercise,which has been shown to help alleviate symptoms and improve physical function,8is recommended in all clinical guidelines9-12as a non-pharmacological approach for managing and treating knee OA.However,many forms of physical activity are either very intense or highly monotonous,making them difficulttoimplementandmaintaininpractice.Oneapproachthat doesnothavethesedisadvantagesisTaiJiQuan(alsoknownasTai ChiChuanandTaiChi).ThistraditionalChinesepracticehaslong beenusedtocultivateandnurturephysicalandmentalwell-being,prevent chronic disease progression,and enhance fitness.13Research increasingly shows that many OA signs and symptoms,suchasreducedjointmobility,poorbalance,pain,increasedjoint stiffness,andlimitedphysicalfunction,canbeamelioratedbyTai Ji Quan training.5,14-20The accumulating evidence has led the AmericanCollegeofRheumatologytorecommendTaiJiQuanas a treatment option for patients with knee OA.12
Duetothedegradationofthekneejoint,peoplewithkneeOA exhibit gait impairments such as reduced walking speed,shorter steplength,anddecreasedknee-jointmotion,21-24characteristics that could have a significant impact on their ability to perform routine daily activities.Previous randomized controlled trials(RCTs),however,have rarely utilized objective measures to quantifychangesingaitcharacteristics18,19followingTaiJiQuan training.Therefore,the extent to which this modality promotes functional gait characteristics remains to be further evaluated. Furthermore,the need to establish its treatment efficacy is of high public health importance in China,where no RCTs have been conducted among Chinese women.Finally,no RCTs have been conducted specifically using tailored Tai Ji Quan movementstoevaluateitstherapeuticbenefitsforthosewithkneeOA.
To fill these gaps,we designed an RCT to determine the efficacy of a specifically tailored Tai Ji Quan training intervention to enhance objectively quantified gait kinematic outcomes among older Chinese women with knee OA.On the basis of prior research,18we hypothesized that a tailored Tai Ji Quan intervention would improve spatiotemporal gait and knee range-of-motion outcomes.
2.Methods
2.1.Trial design
Thestudyusedaparallel-groupRCTdesigntocompareaTai Ji Quan intervention with a health education control across a 24-week period.The trial included a 3-time-per-week intervention with classes conducted in local community centers.The study design and protocols(assessment,group assignment,and training)havebeendescribedelsewhere.25Thetrialprotocolwas approvedbytheEthicsCommitteeoftheShanghaiUniversityof Sport and was performed in accordance with theWorld Medical Association Declaration of Helsinki-Ethical Principles for MedicalResearchinvolvingHumanSubjects.Awritteninformed consent was received from all participants.Chinese ClinicalTrial Registry(June 16,2013):ChiCTR-TRC-13003264.
2.2.Study population and participants
Chinese women were the targeted study population because they have been shown to have a high prevalence of symptomatic and radiographic knee OA.2-5Major inclusion criteria for participating included(1)having a clinical diagnosis of knee OA per the criteria provided by the American College of Rheumatology,26diagnosed through the use of knee radiographs and physical examination,(2)being between 60 and 70 years of age,and(3)being available 3 times a week over a 24-week period.In addition,a radiographic assessment of the erect anterior-posterior and medial-lateral views of both knees was conducted with classification made on the anterior-posterior and tibial-femoral radiographs using the Kellgren-Lawrence(K/L)grading scale(0-4)for knee OA,27in which a grade of≥1 was regarded as knee OA.Individuals who met the KL 1-3 grade standard were recruited.
Exclusion criteria included(1)having had lower limb surgery,(2)having other orthopedic problems of the hip,knee,or ankle,(3)having a neurological disease(e.g.,Parkinson’s,dementia,vertigo,or cerebral apoplexy),or(4)engaging in a current program of regular exercise.Also excluded were individuals who were unable to stand or walk and those who had received other forms of therapy in the preceding 2 months. Finally,those who expected to have major changes in their medication regimen or who were part of a rehabilitation program during the study were also excluded.
Participants were recruited between January and March in 2013 through contacts with community leaders and presentations at various community centers.A follow-up appointment was made for those who responded to the study promotion and indicated an interest in participating.These individuals were asked to visit a designated research facility where a detailed knee OA screening procedure and baseline assessments were conducted.Those who qualified per the study eligibility criteria were subsequently assigned to either the Tai Ji Quan group(TG)or the control group(CG).Intervention began within 1 week after the baseline assessment was completed.
2.3.Randomization and blinding
The individuals who met the eligibility criteria were allocated in a 1:1 ratio using a computer-generated random sequence with a permutated block size of 4.All assignments were made by a research staff member who was not directly involved in the trial.The assessors who conducted the outcome measures were blind to group allocation and were unaware of the study hypotheses.All statistical analyses were performed with masking maintained.
2.4.Intervention
2.4.1.Tai Ji Quan group
Individuals in this group participated in a 60 min session 3 times weekly for 24 weeks.The training protocol included 8 Tai Ji Quan forms:“Withdraw and push”,“Fan through the back”,“Wave hands like clouds”,“Lift hand”,“Brush knee and twist steps”,“Step back to repulse monkey”,“Fair lady works at shuttles”,and“Golden pheasant stands with one leg(right and left)”.All 8 forms were adapted primarily from a 24-form practice routine.28To avoid over-strenuous activities around the knee joints,modifications were made to specifically focus onreducing and avoiding sustained unilateral weight bearing,dynamic rotation of the knee joints,and excessive knee flexion(i.e.,low stance).The overall training protocol followed an easy-to-difficult progression,beginning with standing postures that focused on vertical body alignment,centering of the body mass,multi-directional weight shifting,and gentle and lowfriction load-bearing knee flexion and extension exercises.
The protocol included 3 distinctive phases,with the first phase(Weeks 1-2)focusing on fundamental Tai Ji Quan preparatory movement exercises(e.g.,weight shifting,heel strike,knee flexion and extension,push-off with the toes,stepping in various directions,and meditation and rhythmic breathing techniques).The second phase(Weeks 3-4)focused on learning and practicing forms with their associated movements.The third phase(Weeks 5-24)emphasized practicing and reinforcing the sequence and precision of the forms with variations in practice configuration(i.e.,change in directions).
Interventionmovementswerecloselyintegratedwith rhythmic breathing.Each exercise session included a 5 min warm-up,a 50 min practice,and a 5 min cool-down period.Two instructors with more than 15 years of training and an academic specialization in Tai Ji Quan delivered the intervention.A nationally recognized academic and professional specialist in Tai Ji Quan curriculum and teaching trained the 2 instructors and monitored the fidelity of the intervention delivery on a weekly basis.
2.4.2.Control group
Participants in this group attended one 60 min wellness education lecture bi-weekly.In addition,a 10-15 min weekly check-in phone call was made by research staff members to monitor each participant’s weekly activities,including levels of physical activity and changes in knee pain status and medication use.Each group session consisted of a 40 min lecture and a 20 min discussion on topics related to diagnostic criteria of knee OA,diet and nutrition,pain management and control,wellness and lifestyle changes,physical therapies,and management of medication use.Orthopedic surgeons,nutritionists,and health consultants from local universities and hospitals delivered the lectures.Participants were asked to maintain their regular daily activities and not to start any new exercise programs.
2.5.Study procedures and assessment
At baseline and again at 24 weeks,participants visited the laboratory at the Shanghai University of Sport,where study assessors blinded to study conditions took information related to demographics(age,education),clinical profiles(duration of knee pain,chronic conditions),anthropometric measures(height,weight),and study outcome measures(temporal-spatial gait parameters and physical function).A standardized report form was used to document adverse reactions throughout the 24-week intervention period.The form assessed unanticipated or undesirable experiences or reactions to the intervention exercises or laboratory-based assessment,including any falls,muscle discomfort,and exacerbations of knee-pain symptoms.
2.6.Outcome measures
2.6.1.Primary outcomes
The primary outcomes were changes in gait kinematics of the lower limbs from baseline to 24 weeks,including(1)velocity(cm/s),(2)step length(cm),(3)initial contact angle(°)of the flexed knee,and(4)maximal angle(°)of the flexed knee during the stance phase of walking.Participants were instructed to walk along a 12 m walkway(120×90 cm,length×width)at a comfortable pace,with gait cycles for each limb recorded for 3 trials per established protocol at our laboratory.Threedimensional kinematic data on walking were collected using a 16-camera infrared motion analysis system(Vicon;Oxford Metrics,Oxford,UK).The lower extremity kinematics(velocity,step length,joint angles)were determined from markers placed on the ankles,knees,and hips and estimated joint center displacement data.29The mean value from the 3 trials was calculated for each of the four measures.
2.6.2.Secondary outcomes
Secondary outcomes included measures of the Western OntarioMcMasterUniversitiesOsteoarthritisIndex(WOMAC)30and the Short Physical Performance Battery(SPPB).31The WOMAC,which has been shown to be reliable,valid,and sensitive to change in knee OA populations,30consists of 24 questionsassessedona10 cmvisualanalogscalethatmeasures3 domains:pain(5 items),stiffness(2 items),and functional limitation(17 items).The SPPB,which has psychometric evidence establishedforolderadults,31iscomposedof3tests:(1)3increasinglychallengingstandingbalancetests,(2)ashort-distance(4 m)walk at a normal pace,and(3)standing 5 times from a seated positioninachair.Eachtestwasscoredonanordinalscaleranging from0(worstperformance)to4(bestperformance).Atotalscore wasconstructedusingthesumofthe3tests(rangedfrom0to12),with higher scores indicating better physical performance.
2.7.Sample size
The study was aimed at assessing the efficacy of a tailored Tai Ji Quan intervention on gait kinematics for older Chinese women with knee OA by detecting a between-group difference on the primary outcome of gait velocity in 24 weeks.Based on unpublished data from a prior pilot trial,it was expected that the Tai Ji Quan intervention would result in an 8 cm/s improvement relative to the CG(TG=135 cm/s,CG=127 cm/s,SD=8). With a 5%significance level and 80%power,17 participants per group(34 total)would be needed to provide 80%power. With an anticipated 20%attrition rate,42 total participants were needed.
2.8.Statistical analysis
Baseline demographic and outcome measures across the 2 groups were compared using analysis of variance for continuous variables,the χ2test for categorical variables,or independent t test for proportions.Results were presented as mean±SD or percentages for all outcome measures.Main analyses,based on the intention-to-treat principle,were performed to examine change from baseline using independentt test with a 95%confidence interval(CI).A paired Student’s t test was also performed to compare within-group differences. Scores on gait kinematics were collapsed across both limbs to form an average score in the final analysis.Sensitivity analyses adjusting for potential baseline confounders,including body mass index(BMI),duration of knee pain(in months),chronic conditions,and severity of knee OA as measured by radiography,were also performed.
A 95%CI was reported with each mean value.To adjust for multiple testing,Bonferroni corrections were made with an α level of 0.01 or less(2-sided)in determining statistical significance.Analyses were performed using SPSS 17.0 software(SPSS Inc.,Chicago,IL,USA)
3.Results
Fig.1providesaflowchartforstudyparticipationandfollowup.A total of 135 individuals responded to the study promotion. Of these individuals,89 were excluded for various reasons. Forty-six individuals were qualified and subsequently randomized into either the TG(n=23)or the educational CG(n=23). Thirty-three participants(72%)were in high knee-OA grades(i.e.,KL 2-3).Participant characteristics at baseline across the 2 study groups are presented in Table 1.There were no differences between the 2 groups on baseline characteristics.
The 24-week primary and secondary outcomes were completed by 21 of 23 participants(91%)in the TG and 19 of 23 participants(90%)in the educational CG(Fig.1).No adverse events(i.e.,falls,significant joint pain or injury,cardiac arrest)were observed during the 24-week study period.

Table 1 Baseline characteristics of the study participants.
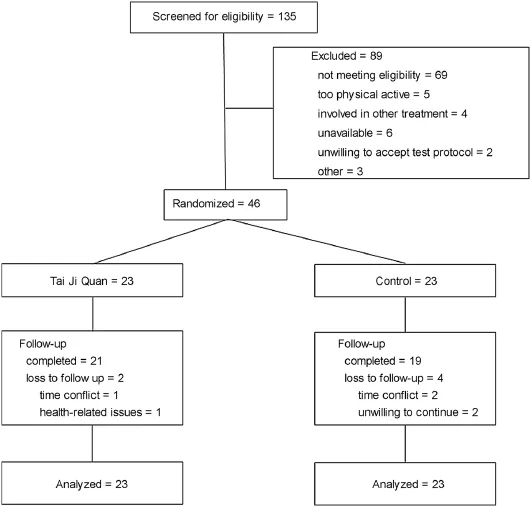
Fig.1.Flow chart for study participation.
The average attendance rate(defined as the mean percentage of the exercise or education sessions that were completed by participants within each study group)across the 24-weekintervention period was 87%for the TG and 78%for the CG. Six participants(n=2 in Tai Ji Quan,n=4 in control)withdrew from the study.Table 2 presents descriptive statistics on the primary outcomes.At 24 weeks,relative to the CG the TG showed greater improvement in gait velocity(8.40 cm/s,p=0.01)and step length(3.52 cm,p=0.004).In addition,compared to the CG theTG increased significantly in the initial contact angle(2.19°,p=0.012)and maximal angle at the knee joint during the stance phase(2.61°,p=0.003).Sensitivity analyses showed the outcome results were not affected by baseline characteristics(i.e.,BMI,duration of knee pain,or severity of knee OA).

Table 2 Changes in gait kinematics from baseline to the 24-week follow-up(mean±SD).
After 24 weeks,compared to the CG the TG demonstrated a significantly greater decrease in knee pain(-4.22 points,p=0.002),knee stiffness(-2.41 points,p<0.001),and functional limitation(-11.04 points,p=0.006).Similarly,compared to those in the CG,participants in the TG showed a significantly greater improvement in SPPB scores(1.22 points,p<0.001)(Table 3).
4.Discussion
In this RCT we examined whether a tailored Tai Ji Quan interventionwouldimprovegaitkinematicsandphysicalfunction amongapopulationofChineseolderadultwomendiagnosedwith knee OA.The findings from this 24-week intervention revealed that individuals receivingTai Ji Quan training showed significant improvements in gait velocity,stride length,initial contact angle of the knee,and maximal angle of the knee compared to those in the educational control.The study also showed that Tai Ji Quan participants had a meaningful improvement in physical function as measured by both the WOMAC(>35%improvement in all 3 subscale measures from baseline)and SPPB(>1.0).31The intervention was shown to be well tolerated by the participants as evidencedbytheabsenceofanyadverseeventsandalowattrition rate.

Table 3 Changes in secondary outcome measures of WOMAC and SPPB from baseline to the 24-week follow-up(point,mean±SD).
ComparedtotheCG,theTGdemonstratedimprovedrangeof motionatthekneejointduringthestancephaseofgait.Although the mechanism(s)by which the intervention improved gait outcomes remains to be determined,the changes may be attributed to the specific characteristics inherent in the training protocol that focus on controlling posture and strengthening muscles around major joints(hip,knees,and ankles).Specifically,these exercisesincludeposturalalignment(standingandtransitioning to upright poses,knee alignment in the support phase of gait),pre-movement preparation(expectant weight-shifting),movement initiation(stepping with hip flexion,knee extension,plantar-and dorsi-flexion),lateral and diagonal performance of forms(strengthening hip adduction and external rotation),and slow and controlled unipedal standing positions(strengthening leg muscles with unilateral weight-bearing).
The gait kinematics findings from this study are congruent with those reported from an uncontrolled study in the US,which showed,among other outcomes,improved stride length and frequency,and gait velocity.18Taken together,the emerging research indicates not only encouraging evidence for therapeutic application but also points to the possibility of incorporating this program for prevention among those with significant risk factors for developing knee OA.
The study has some notable strengths.First,our study represents the first known RCT that specifically targeted a female Chinese population with a high prevalence of knee OA.2-5It is also the first study to use a specifically tailored Tai Ji Quan routine to treat women with knee OA.This is an important effort since not allTai Ji Quan-based movements are considered functionally appropriate and safe for people with knee OA.A tailored training approach is recommended for evaluating specific health benefits of Tai Ji Quan.32Finally,the use of the laboratory-based gait measures enhanced the objectivity of the study outcomes.
There are also some important limitations in this trial that future research should address.First,the fact that only selfselected older Chinese women with knee OA participated in our studylimitsthegeneralizabilityofthefindingstootherpopulation groups with knee OA.Second,the intervention contact time across the 2 study conditions was not equivalent due to logistical constraints,so participants in the Tai Ji Quan intervention may have improved because of their additional exposure time.Third,since the study lacked an exercise control condition,future studies should include a comparable exercise control group with equaltimeallocatedtoeachcondition.Finally,studiesthatinclude a follow-up assessment after a period of time beyond the active intervention would help determine whether the benefits of Tai Ji Quan can be maintained beyond the initial training sessions.
The study points to the need for continued research to delineate the mechanism(s)through which the Tai Ji Quan intervention produced effects on gait.Since our gait measures were limited in scope,they preclude an in-depth analysis of the therapeutic effects of Tai Ji Quan for people with knee OA.For example,with the improved range of motion at the knee joint,the biomechanical impact of heel-landing on the knee joint during the stance phase of gait remains to be explored.In addition,because knee OA affects both medial and lateral compartments of the tibiofemoral joint among Chinese adults,3future studies should examine the potential biomechanical influence of ankle and hip joint kinetics after completion of a Tai Ji Quan intervention on change in pain and gait outcomes in people with either medial or lateral knee OA.
5.Conclusion
Among older Chinese women with knee OA,a tailored,24-weekTai Ji Quanintervention was shown to be efficaciousin improving gait and other physical health outcomes.With the increase in the aging population in China and the accompanying high prevalence of knee OA,additional trials with more rigorous design and methodology are needed to understand the full potential of Tai Ji Quan for improving biomechanical characteristics and functional mobility as well as reducing pain symptomatology in knee OA patients.
Acknowledgments
The authors would like to thank all participants for their full cooperation and support during the conduct of this study,as well as the MartialArts Department of the Shanghai University of Sport for its assistance in providing technical support and teaching of the intervention classes.The authors would also like to thank the administrative departments of the communitybased organizations and local government agencies(especially the People’s Government of Wu Jiao Chang in the Yangpu District in Shanghai),as well as Mrs.Zhihua Lu,for their assistance in recruiting study participants.
This study was funded by the Shanghai City Committee of Science and Technology Key Project(No.12490503200)and the National Science Foundation for Distinguished Young Scholars of China(No.81025022).
YL and JXL contributed to the conception,protocol development,and design of the study.QZ and LH participated in data acquisition,analysis,and interpretation.XW,LW,YZ,and MF contributed to data acquisition,gait kinematics testing,and data interpretation.All authors have contributed significantly to the various stages in the writing of this manuscript and approved the final version of the paper.All authors agree with the order of presentation of the authors.
Competing interests
None of the authors declare competing financial interests.
1.Nguyen US,Zhang Y,Zhu Y,Niu J,Zhang B,Felson DT.Increasing prevalence of knee pain and symptomatic knee osteoarthritis:survey and cohort data.Ann Intern Med 2011;155:725-32.
2.Zhang Y,Xu L,Nevitt MC,Aliabadi P,Yu W,Qin M,et al.Comparison of the prevalence of knee osteoarthritis between the elderly Chinese population in Beijing and whites in the United States:the Beijing osteoarthritis study.Arthritis Rheum 2001;44:2065-71.
3.Felson DT,Nevitt MC,Zhang Y,Aliabadi P,Baumer B,Gale D,et al.High prevalence of lateral knee osteoarthritis in Beijing Chinese compared with Framingham Caucasian subjects.Arthritis Rheum 2002;46:1217-22.
4.Kang X,Fransen M,Zhang Y,Li H,Ke Y,Lu M,et al.The high prevalence of knee osteoarthritis in a rural Chinese population:the Wuchuan osteoarthritis study.Arthritis Rheum 2009;61:641-7.
5.Jiang L,Rong J,Zhang Q,Hu F,Zhang S,Li X,et al.Prevalence and associated factors of knee osteoarthritis in a community-based population in Heilongjiang,Northeast China.Rheumatol Int 2012;32:1189-95.
6.Bijlsma JW,Berenbaum F,Lafeber FP.Osteoarthritis:an update with relevance for clinical practice.Lancet 2011;377:2115-26.
7.Peat G,McCarney R,Croft P.Knee pain and osteoarthritis in older adults:a review of community burden and current use of primary health care.Ann Rheum Dis 2001;60:91-7.
8.Fransen M,McConnell S,Harmer AR,Van der Esch M,Simic M,Bennell KL.Exercise for osteoarthritis of the knee:a Cochrane systematic review. Br J Sports Med 2015;49:1554-7.
9.McAlindon TE,Bannuru RR,Sullivan MC,Arden NK,Berenbaum F,Bierma-Zeinstra SM,et al.OARSI guidelines for the non-surgical management of knee osteoarthritis.Osteoarthritis Cartilage 2014;22:363-88.
10.Jevsevar DS.Treatment of osteoarthritis of the knee evidence-based guideline(2nd ed.).J Am Acad Orthop Surg 2013;21:571-6.
11.Australian Government National Health and Medical Research Council. Guideline for the non-surgical management of hip and knee osteoarthritis. Availableat:https://www.nhmrc.gov.au/_files_nhmrc/publications/ attachments/cp117-hip-knee-osteoarthritis.pdf;[accessed 01.02.2016].
12.Hochberg MC,Altman RD,April KT,Benkhalti M,Guyatt G,McGowan J,et al.American College of Rheumatology 2012 recommendations for the use of nonpharmacologic and pharmacologic therapies in osteoarthritis of the hand,hip,and knee.Arthritis Care Res(Hoboken)2012;64:465-74.
13.Guo YC,Qiu PX,Liu TG.Tai Ji Quan:an overview of its history,health benefits,and cultural value.J Sport Health Sci 2014;3:3-8.
14.Brismée JM,Paige RL,Chyu MC,Boatright JD,Hagar JM,McCaleb JA,et al.Group and home-based Tai Chi in elderly subjects with knee osteoarthritis:a randomized controlled trial.Clin Rehabil 2007;21:99-111.
15.Lauche R,Langhorst J,Dobos G,Cramer H.A systematic review and meta-analysis of Tai Chi for osteoarthritis of the knee.Complement Ther Med 2013;21:396-406.
16.Lee HJ,Park HJ,Chae Y,Kim SY,Kim SN,Kim ST,et al.Tai Chi Qigong for the quality of life of patients with knee osteoarthritis:a pilot,randomized,waiting list controlled trial.Clin Rehabil 2009;23:504-11.
17.Lee MS,Pittler MH,Ernst E.Tai chi for osteoarthritis:a systematic review. Clin Rheumatol 2008;27:211-8.
18.Shen CL,James CR,Chyu MC,Bixby WR,Brismée JM,Zumwalt MA,et al.Effects of Tai Chi on gait kinematics,physical function,and pain in elderly with knee osteoarthritis—a pilot study.Am J Chin Med 2008;36:219-32.
19.Song R,Lee EO,Lam P,Bae SC.Effects of Tai Chi exercise on pain,balance,muscle strength,and perceived difficulties in physical functioning in older women with osteoarthritis:a randomized clinical trial.J Rheumatol 2003;30:2039-44.
20.Wang C,Schmid CH,Hibberd PL,Kalish R,Roubenoff R,Rones R,et al. Tai Chi is effective in treating knee osteoarthritis:a randomized controlled trial.Arthritis Rheum 2009;61:1545-53.
21.Bejek Z,Paróczai R,Illyés A,Kiss RM.The influence of walking speed on gait parameters in healthy people and in patients with osteoarthritis.Knee Surg Sports Traumatol Arthrosc 2006;14:612-22.
22.Elbaz A,Mor A,Segal G,Debi R,Shazar N,Herman A.Novel classification of knee osteoarthritis severity based on spatiotemporal gait analysis.Osteoarthritis Cartilage 2014;22:457-63.
23.Huang SC,Wei IP,Chien HL,Wang TM,Liu YH,Chen HL,et al.Effects of severity of degeneration on gait patterns in patients with medial knee osteoarthritis.Med Eng Phys 2008;30:997-1003.
24.Zeni JA,Higginson JS.Differences in gait parameters between healthy subjects and persons with moderate and severe knee osteoarthritis:a result of altered walking speed?Clin Biomech 2009;24:372-8.
25.Wang XQ,Huang LY,Liu Y,Li JX,Wu X,Li HP,et al.Effects of Tai Chi program on neuromuscular function for patients with knee osteoarthritis:study protocol for a randomized controlled trials.Trials 2013;14:375. doi:10.1016/j.medengphy.2008.02.006
26.Altman R,Asch E,Bloch D,Bole G,Borenstein D,Brandt K,et al. Developmentofcriteriafortheclassificationandreportingof osteoarthritis.Classification of osteoarthritis of the knee.Arthritis Rheum 1986;29:1039-49.
27.Kellgren JH,Lawrence JS.Radiographic assessment of osteo-arthrosis. Ann Rheum Dis 1957;16:494-502.
28.China Sports Editorial Board.Simplified“Taijiquan”.Beijing:China Sports Editorial Board;1980.[in Chinese].
29.Kadaba MP,Ramakrishnan HK,Wootten ME.Measurement of lower extremity kinematics during level walking.J Orthop Res 1990;8:383-92.
30.Bellamy N,Buchanan WW,Goldsmith CH,Campbell J,Stitt LW. Validation study of WOMAC:a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee.J Rheumatol 1988;15:1833-40.
31.Guralnik JM,Simonsick EM,Ferrucci L,Glynn RJ,Berkman LF,Blazer DG,et al.A short physical performance battery assessing lower extremity function:association with self-reported disability and prediction of mortality and nursing home admission.J Gerontol 1994;49:M85-94.
32.Li F.Transforming traditional Tai Ji Quan techniques into integrated movement therapy-Tai Ji Quan:moving for better balance.J Sport Health Sci 2014;3:9-15.
.
E-mail addresses:yuliu@sus.edu.cn(Y.Liu);jli@uottawa.ca(J.X.Li)
s’contributions
15 September 2015;revised 9 December 2015;accepted 18 December 2015 Available online 15 February 2016
杂志排行
Journal of Sport and Health Science的其它文章
- Physical activity and health in the presence of China’s economic growth:Meeting the public health challenges of the aging population
- Physical activity and cognitive function among older adults in China:A systematic review
- Recruitment of older adults into randomized controlled trials:Issues and lessons learned from two community-based exercise interventions in Shanghai
- Associations between individual and environmental factors and habitual physical activity among older Chinese adults:A social-ecological perspective
- Exercise-induced rhabdomyolysis mechanisms and prevention:A literature review
- Scientific evidence is just the starting point:A generalizable process for developing sports injury prevention interventions
