颈椎前路融合术后非融合节段退变性疾病的回顾性研究
2016-09-07郭炳路宋科冉陈巧灵陈增海王大鹏王慧金培唐家广
郭炳路 宋科冉 陈巧灵 陈增海 王大鹏 王慧 金培 唐家广
颈椎前路融合术后非融合节段退变性疾病的回顾性研究
郭炳路 宋科冉 陈巧灵 陈增海 王大鹏 王慧 金培 唐家广
目的 探讨颈椎前路减压融合术后非融合节段病变(non-fusion segment disease,NFSD)的发生率和原因。方法 回顾性分析 1998 年 1 月至 2011 年 1 月,在解放军总医院第一附属医院行颈椎前路减压融合术的 171 例的临床资料,其中男 97 例,女 74 例,年龄 31~72 岁,平均(51.90±9.28)岁。探讨症状性NFSD 的发生率和临床参数(患者初次手术时的年龄及融合节段数)及影像学参数(患者初次手术前后的颈椎曲度、术前 C5水平 Pavolv 比值,以及术前颈椎 MRI 显示非融合节段椎间盘退变的程度)之间的关系。结果本组 171 例中 16 例(9.36%)术后出现了 NFSD。其中 12 例为融合部位邻近节段病变,4 例为融合部位非邻近节段病变。NFSD 组患者术后颈椎曲度明显小于非 NFSD 组患者 [(7.38±12.37)° vs.(17.26±9.75)°,P<0.001 ]。NFSD 组患者融合节段数为 1.63 个,而非 NFSD 组患者为 2.27 个(P=0.002)。NFSD 组患者非融合节段椎间盘退变程度明显重于非 NFSD 组患者 [ MRI 得分(2.63±0.62)vs.(1.62±0.99),P=0.008 ]。结论 颈椎前路融合术后症状性 NFSD 的发生有多种因素。术后颈椎曲度、非融合节段椎间盘退变程度以及融合节段数都参与 NFSD 的发生。
颈椎;脊柱融合术;颈椎病;非融合节段病变
50 年前,Robinson 和 Smith[1]采用颈椎前路椎间盘切除减压融合(anterior cervical discectomy and fusion,ACDF)治疗颈椎病后,大量随访结果表明该方法能有效改善脊髓型和神经根型颈椎病的临床症状。然而,影像学长期随访结果显示融合部位邻近节段退行性变的发生率可高达 50%~60%[2-3]。而引起新症状的邻近节段退变,即邻近节段病变(adjacent segment disease,ASD)的发生率约为7%~15%[4-7]。ASD 的发生是由于融合邻近节段椎间盘内压力增高还是椎间盘自然退变的结果,或者是其它因素所致目前尚不清楚。回顾性分析 1998 年 1 月至 2011 年 1 月,因颈椎间盘突出和颈椎病在解放军总医院第一附属医院行颈椎前路减压融合的171 例的临床随访资料,以探讨颈椎前路融合术后非融合节段(包括融合部位的邻近节段和非邻近节段)病变(non-fusion segment disease,NFSD)的发生率及原因。
资料与方法
一、一般资料
本组 171 例,其中男 97 例,女 74 例,年龄 31~72 岁,平均(51.90±9.28)岁。其中 31 例行单间隙融合,80 例行 2 个间隙融合,53 例行 3 个间隙融合,7 例行 4 个间隙融合。参考 Smith-Robinson 技术进行颈椎前路减压融合[1]。对于 2 个节段以上的病变,采用 ACDF 和(或)椎体次全切除减压融合。所有患者都至少经过 3 个月的保守治疗。术前摄颈椎 X 线片及 MRI 明确病变节段。术后 1 天佩戴颈托下床行走,术后 8 周门诊复查 X 线片。
二、临床与影像学分析
以门诊复查的方式采集临床资料,包括患者临床症状的变化,神经系统检查和影像学检查结果。对随访期间出现新神经症状的患者进行了颈椎 MRI检查。诊断非融合节段病变的依据为:出现新的与病变节段相一致的神经根性疼痛或脊髓受压症状,颈椎 MRI 显示同一节段出现神经根或脊髓压迫性损害。随访的临床参数包括:患者初次手术时的年龄及融合节段数。影像学参数包括:患者初次手术前后的颈椎曲度、术前 C5水平 Pavolv 比值以及术前颈椎 MRI 显示非融合节段椎间盘退变的程度。站立位拍摄颈椎侧位 X 线片,测量 C2椎体上缘到 C7椎体下缘之间的颈椎曲度。术后测量患者末次随访时的颈椎曲度。为方便对比不同患者非融合节段椎间盘退变程度,采用 5 分法对颈椎 MRI 非融合节段退变明显的间隙进行评分。0 分:椎间盘无退变;1 分:椎间盘退变未突出,硬膜囊未受压;2 分:椎间盘退变突出,硬膜囊轻度受压;3 分:椎间盘退变突出,硬膜囊下间隙消失;4 分:椎间盘退变突出,脊髓受压。
三、统计学处理
结 果
本组随访时间 3~13 年,平均(6.70±3.16)年。16 例(9.36%)术后出现 NFSD。其中男 9 例,女7 例。12 例为融合部位 ASD,4 例为融合部位非邻近节段病变。从第一次手术到 NFSD 症状出现的时间为 1~13 年,平均(5.00±2.83)年。NFSD 组初次手术的年龄、术前颈椎曲度、C5水平 Pavolv 比值与非 NFSD 组比较,差异无统计学意义(P=0.350,0.112,0.286)。NFSD 组患者术后颈椎曲度、融合节段数、术前 MRI 评分与非 NFSD 组比较,差异有统计学意义(P<0.001,P=0.02,P=0.008)(表 1)。典型病例见图 1、2。
表1 NFSD组和非NFSD组患者临床和影像学资料比较(± s)Tab.1 Differences of clinical and radiological parameters between NFSD group and disease-free group(± s)
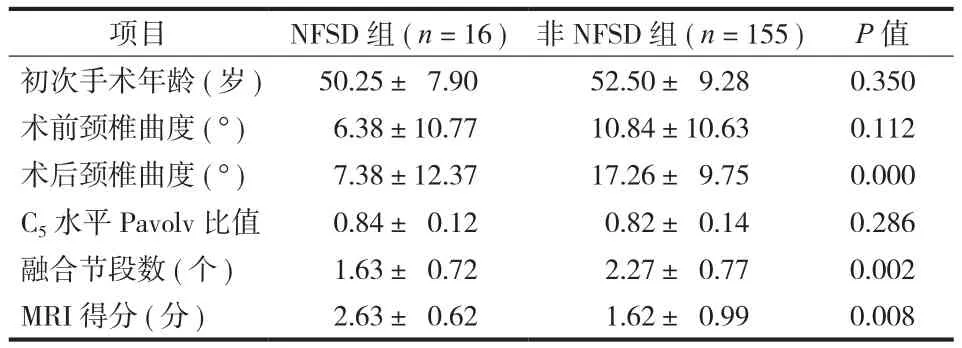
表1 NFSD组和非NFSD组患者临床和影像学资料比较(± s)Tab.1 Differences of clinical and radiological parameters between NFSD group and disease-free group(± s)
项目 NFSD 组(n = 16)非 NFSD 组(n = 155) P 值初次手术年龄(岁) 50.25± 7.90 52.50± 9.28 0.350术前颈椎曲度(°) 6.38±10.77 10.84±10.63 0.112术后颈椎曲度(°) 7.38±12.37 17.26± 9.75 0.000 C5水平 Pavolv 比值 0.84± 0.12 0.82± 0.14 0.286融合节段数(个) 1.63± 0.72 2.27± 0.77 0.002 MRI 得分(分) 2.63± 0.62 1.62± 0.99 0.008
讨 论
该研究表明,颈椎前路减压融合术后颈椎曲度、术前非融合节段椎间盘退变程度、融合间隙数都与 NFSD(包括融合部位邻近节段疾病和融合部位非邻近节段疾病)有关,表明 NFSD 的发生为多因素。
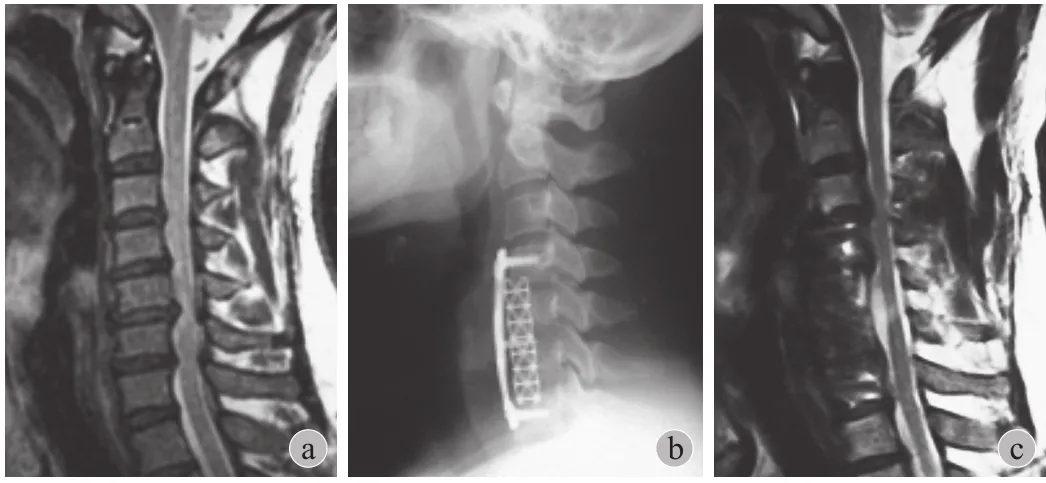
图1 患者,男,47 岁,多节段颈椎间盘突出,入院后行 C4~7减压融合术后,临床症状得到明显改善,术后 6 年出现了与C3~4相关的髓性症状,MRI 显示该水平的椎间盘退变以及大的椎间盘突出压迫脊髓 a:术前 T2加权像颈椎 MRI 提示 C3~4,C4~5,C5~6,C6~7硬膜囊受压凹陷;b:术后 X 线片示 C4~73 个节段的融合;c:术后 6 年颈椎 MRI 示 C4~7减压彻底,但C3~4节段脊髓明显受压Fig.1 A 47-year-old male with multilevel cervical intervertebral disc herniation. Anterior cervical decompression and fusion were performed and significant immediate improvement in clinical symptom was achieved. However, 6 years post-op new onset myelopathy referable to the C3-4level had developed. MRI showed disc degeneration at this level and a large disc herniation compressing the spinal cord a: Preoperative T2-weighted MRI showed an indentation of dura mater at C3-4, C4-5, C5-6, and C6-7levels; b: Radiograph after the operation showed 3 levels fusion from C4-7; c: MRI at 6 years after the operation indicated complete decompression from C4-7levels, but C3-4level showed significant spinal cord compression
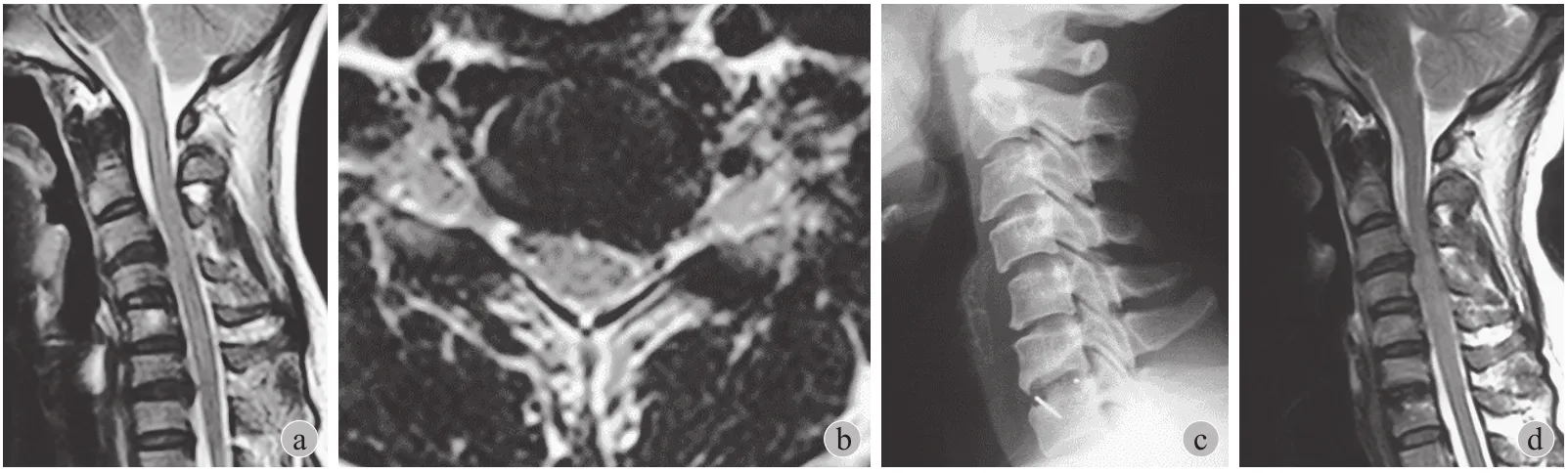
图2患者,女,39岁,C6~7椎间盘突出。考虑到患者的症状主要是由于 C6~7水平压迫所致,行颈椎前路间盘切除减压融合(ACDF),疼痛和麻木症状立刻得到缓解。患者术后 1 年出现严重颈部疼痛,轻度步态异常。MRI 显示C3~4水平明显的脊髓压迫 a~b:术前矢状位和横断位 T2加权像显示 C6~7节段左侧椎间盘突出,神经根受压;c:X 线片显示 C6~7融合;d:术后 1 年 T2加权像颈椎 MRI 显示 C6~7节段减压彻底,但 C3~4节段脊髓受压明显
Fig.2 A 39-year-old female with C6-7cervical intervertebral disc herniation. Considering the C6-7compression was the responsible level, anterior cervical discectomy and fusion(ACDF)were performed, immediately relieving pain and numbness. However, 1 year post-op the patient presented with severe neck pain and a little gait disturbance. MRI showed obvious spinal cord compression at the C3-4level a - b: Preoperative T2-weighted MRI showed left nerve root compression at C6-7level and disc degeneration at C3-4level; c: Radiograph after the operation showed C6-7fusion; d:MRI at 1 year after the operation indicated complete decompression at C6-7, but severe spinal cord compression could be seen at C3-4level
有关颈椎曲度和 ASD 关系的报道不多。Katsuura 等[8]发现颈椎前路融合术后 43% 的邻近节段退变患者就诊时颈椎曲度不良。融合后 77% 的颈椎后凸位患者邻近节段椎间盘发生了退行性变。Kumar 等[9]研究了腰椎矢状位失衡和 ASD 的关系,发现矢状失衡和(或)骶骨垂直倾斜角大的患者邻近节段退变发生率为 50%,远远高于正常矢状位力线和正常骶骨垂直倾斜角患者。生物力学研究结果也证实矢状位力线对邻近节段退变的发生有影响[10]。笔者临床研究结果也支持这一观点,NFSD 患者颈椎前凸角度明显小于非 NFSD 患者,表明融合后颈椎曲度影响NFSD 的发生,保持正常颈椎曲度可能会降低 NFSD的发生。
笔者的研究发现,术前颈椎 MRI 显示 NFSD 组患者非融合节段椎间盘退变程度高于非 NFSD 组,该结果与 Hilibrand 等[6]的结果相似。其对 374 例行颈椎前路融合术的患者进行了长期随访,发现术前邻近节段影像学退变明显与术后 ASD 的发生相关。在 Ishihara 等[11]的一个研究中,ACDF 患者术后症状性邻近节段退变高发于术前脊髓造影或 MRI 检查提示该节段存在非症状性椎间盘退变的患者。该结果证明出现 ASD 的部分原因是持续发生的自然退变的结果,而不单纯是融合后的并发症。因颈椎外伤行融合的患者 ASD 的发生率远远低于因退行性变而行融合的患者,该结果也进一步支持了自然退变是导致 ASD 的一个重要原因。
笔者的随访临床资料显示,4 例出现了症状性的非邻近节段疾病,术前 MRI 显示在这些节段都存在椎间盘退行性改变,这一结果进一步支持了自然退变在 NFSD 发生中的重要作用。这与 Frymoyer 等[12]的研究相似,其对大量腰椎融合患者进行了临床研究,发现融合邻近节段和非邻近节段的退变程度相似。保留节段运动能预防邻近节段退变的理念促使了人工颈椎间盘(total disc arthmplasty,TDA)的出现。然而,在一个前瞻性随机对照 FDA 器械临床研究豁免试验中,Jawahar 等[13]发现 TDA 和ACDF 在 ASD 的发生中没有明显差别,但在腰椎间盘退变患者中,颈椎 ASD 的发生明显增加,该论文 2010 年被 Spine Journal 评为杰出论文。临床工作中,学者们已经发现大多数接受颈椎病手术的患者不只存在单节段病变。但考虑到引起症状的节段(责任节段)减压后患者症状明显缓解,多数医生不愿意将有退变的但不引起临床症状的节段(无辜节段)减压融合。然而,一些患者的确会出现 NFSD。因此,很难决断那些“无辜节段”是否需要融合。尽管不提倡无理论根据的增加融合节段,临床上确实发现那些退变明显的非责任节段在术后不久就退变加重并产生新的临床症状,因此有时增加融合节段确实能够降低 ASD 的发生。笔者的研究证明非NFSD 组平均融合 2.27 节段,而 NFSD 组平均融合节段为 1.63 个。另外,Hillibrand 等[6]也报道多节段融合后 ASD 的发生率降低。一般认为多节段融合更增加了邻近节段的负担,容易引发 ASD 的发生,然而临床研究的结果恰恰相反。这些结果表明 ASD 的发生不仅仅是由于融合的结果,自然退变也起着重要的作用。因此多节段融合能够提供一定程度的保护作用。
总之,笔者的研究结果表明, NFSD 的发生有着多种因素。术后颈椎曲度、非症状节段椎间盘退变的程度,以及融合节段数在 NFSD 的发生中都起着重要作用。为预防 NFSD 的发生,在行颈椎前路融合时应考虑到这些因素。
[1] Robinson RA, Smith GW. Anterolateral cervical disc removal and interbody fusion for cervical disc syndrome. Bull John Hopkins Hosp, 1955, 96:223-224.
[2] Teramoto T, Ohmori K, Takatsu T, et al. Long-term results of the anterior cervical spondylodesis. Neurosurgery, 1994,35(1):64-68.
[3] Goffin J, van Loon J, Van Calenbergh F, et al. Long-term results after anterior cervical fusion and osteosynthetic stabilization for fractures and/or dislocations of the cervical spine. J Spinal Disord, 1995, 8(6):500-508.
[4] Bohlman HH, Emery SE, Goodfellow DB, et al. Robinson anterior cervical discectomy and arthrodesis for cervical radiculopathy. Long-term follow-up of one hundred and twenty-two patients. J Bone Joint Surg Am, 1993, 75(9):1298-1307.
[5] Gore DR, Sepic SB. Anterior cervical fusion for degenerated or protruded discs. A review of one hundred forty-six patients. Spine, 1984, 9(7):667-671.
[6] Hilibrand AS, Carlson GD, Palumbo MA, et al. Radiculopathy and myelopathy at segments adjacent to the site of a previous anterior cervical arthrodesis. J Bone Joint Surg Am, 1999, 81(4):519-528.
[7] Lunsford LD, Bissonette DJ, Jannetta PJ, et al. Anterior surgery for cervical disc disease. Part1: treatment of lateral cervical disc herniation in 253 cases. J Neurosurg, 1980, 53(1):1-11.
[8] Katsuura A, Hukuda S, Saruhashi Y, et al. Kyphotic malalignment after anterior cervical fusion is one of the factors promoting the degenerative process in adjacent intervertebral levels. Eur Spine J, 2001, 10(4):320-324.
[9] Kumar M, Baklanov A, Chopin D, et al. Correlation between sagittal plane changes and adjacent segment degeneration following lumbar spine fusion. Eur Spine J, 2001, 10(4):314-319.
[10] Oda I, Cunningham BW, Buckley RA, et al. Does spinal kyphotic deformity influence the biomechanical characteristics of the adjacent motion segments? An in vivo animal model. Spine, 1999, 24(20):2139-2146.
[11] Ishihara H, Kanamori M, Kawaguchi Y, et al. Adjacent segment disease after anterior cervical body fusion. Spine J, 2004, 4(6):624-628.
[12] Frymoyer JW, Hanley E, Howe J, et al. Disc excision and spine fusion in the management of lumbar disc disease: a minimum ten-year follow up. Spine, 1978, 3(1):1-6.
[13] Jawahar A, Cavanaugh DA, Kerr EJ, et al. Total disc arthroplasty does not affect the incidence of adjacent segment degeneration in cervical spine: results of 93 patients in three prospective randomized clinical trials. Spine J, 2010, 10(12):1043-1048.
(本文编辑:王萌)
Non-fusion segment disease after the anterior cervical arthrodesis: a retrospective study
GUO Bing-lu, SONG Ke-ran, CHEN Qiao-ling, CHEN Zeng-hai, WANG Da-peng, WANG Hui, JIN Pei, TANG Jia-guang. Orthopaedic Department of Gaobeidian Hospital, Gaobeidian, Hebei, 074000, PRC
TANG Jia-guang, Email: tangjiaguang2013@163.com
Objective To investigate the incidence and causes of non-fusion segment disease(NFSD), both adjacent and non-adjacent to the fused segment, after the anterior cervical arthrodesis. Methods This is a retrospective cohort study. Between January 1998 and January 2011, 171 patients who had anterior cervical decompression and fusion for the intervertebral disc herniation and cervical spondylosis were followed clinically. There were 97 males and 74 females, and the average age at the operation was(51.90 ± 9.28)years(range: 31 - 72 years). We evaluated the correlation between the incidence of symptomatic non-fusion segment disease and the following clinical parameters(age at the operation, fusion levels)and radiological parameters(preoperative and postoperative cervical spine alignment, Pavlov’s ratio at the C5level, and preoperative existence of a non-fusion segment degeneration on magnetic resonance imaging). Results Of the 171 patients reviewed, 16 patients had non-fusion segment disease(9.36%),12 patients had adjacent segment disease and 4 had non-adjacent segment disease. Postoperative cervical lordosis in the non-fusion segment disease group was significantly smaller than that of the disease-free group [(7.38 ± 12.37)° vs.(17.26 ± 9.75)°, P < 0.001 ]. Fusion levels in the NFSD group were 1.63 whereas 2.27 in disease-free group(P = 0.002). The incidence of disc degeneration in non-fused segments was more severe in the NFSD group than in the disease-free group [(2.63 ± 0.62)vs.(1.62 ± 0.99), P = 0.008 ]. Conclusions The incidence of symptomatic non-fusion segment disease after the anterior cervical arthrodesis has multifactorial causes. Postoperative cervical lordosis, disc degeneration in non-fusion segments, and the number of fusion levels are all factors in the incidence of NFSD.
Cervical vertebrae; Spinal fusion; Cervical spondylosis; Non-fusion segment disease
10.3969/j.issn.2095-252X.2016.08.012 中图分类号:R681.5
074000 河北,高碑店市医院骨科(郭炳路、陈增海、王大鹏、王慧、金培);100048 北京,解放军总医院第一附属医院骨科(宋科冉、陈巧灵、唐家广)
唐家广,Email: tangjiaguang2013@163.com
(2016-03-22)