超声内镜对ERCP术前不明原因胆总管扩张的应用探讨
2016-07-13张莉王震宇王光霞王庆
张莉,王震宇,王光霞,王庆
超声内镜对ERCP术前不明原因胆总管扩张的应用探讨
张莉1,王震宇1,王光霞1,王庆1
目的探讨超声内镜(EUS)在逆行胆胰管造影术(ERCP)前对不明原因胆总管扩张的诊断价值。方法60例不明原因胆总管扩张患者,经腹部超声(TUS)、CT和(或)磁共振胰胆管造影(MRCP)检查提示胆总管扩张、可疑胆胰病变但原因不明,ERCP术前行EUS检查诊断,并以ERCP、手术病理及随访确诊的结果为最终诊断。结果经ERCP确诊为胆总管下端结石者39例,EUS诊断38例,另1例EUS诊为胆总管下端肿瘤。ERCP及手术病理确诊为胆总管下端肿瘤10例、胆管内乳头状瘤2例、壶腹部肿瘤2例;EUS诊断结果分别为11例、0例及3例,其中1例确诊为胆总管下端结石者EUS提示为胆总管下端肿瘤,2例确诊为胆管内乳头状瘤患者EUS将其中1例诊断为炎性狭窄,另1例诊断为壶腹部肿瘤。术后随访确诊为十二指肠乳头炎性狭窄7例,EUS诊断结果为8例,其中1例术后随访并经ERCP病理确诊为胆管内乳头状瘤。诊断正确率95%(57/60)。结论EUS对不明原因胆总管扩张的定位及定性诊断均有很高的诊断价值,特别是能提高胆总管下端结石确诊率,高于MRCP检查,并能指导选择性地进行ERCP,提高治疗效果,减少风险。
胆胰管造影术,内窥镜逆行;超声内镜;胆总管扩张
胆胰系统复杂的解剖结构使得胆胰结合部病变的术前鉴别诊断变得困难,目前诊断主要依赖于影像学检查。经腹部超声(transabdominal ultrasound,TUS)是一种快速、非侵入性的检查方式,但常常因气体、脂肪组织等干扰使胆道下端图像较难判定;电子计算机断层扫描(computed tomography,CT)具有非侵入性的优势,但存在X线辐射问题;且TUS和CT判断胆管扩张原因的特异度不高。逆行胰胆管造影术(endoscopic retrograde cholangiopancreatography,ERCP)被认为是诊断胆道系统疾病的金标准,但其具有侵入性,且存在术后发生胰腺炎等严重并发症的潜在风险[1]。磁共振胰胆管造影(magnetic resonance cholangiopancreatography,MRCP)可较准确地反映胆道系统的状态,但受胆道充盈的影响,仅对胆道异常图像敏感,亦无法提供组织学诊断,存在一定的局限性[2]。在TUS、CT、MRCP等未明确诊断情况下,盲目地进行ERCP或者手术治疗,更易对患者造成伤害。超声内镜(endoscopic ultrasonography,EUS)可提高对胆胰结合部病变的检出率及诊断率,且有可能获得组织病理学诊断结果,确定病变侵及的深度、恶性病变的远处分期情况,从而提高术前胆管扩张微小病变的诊断率,减少相关并发症的发生率[3]。本研究旨在就可疑胆胰病变且胆总管扩张原因不明患者的EUS诊断的相关资料进行回顾性分析,探讨EUS对此类患者的临床诊断价值。
1 对象与方法
1.1研究对象选取2014年9月—2015年9月就诊于我院内镜中心,经腹部超声、CT和(或)MRCP检查初步诊断为可疑胆胰病变但原因不明的胆总管扩张患者60例,男36例,女24例,年龄为(61.7±12.1)岁。多数患者因右上腹痛就诊,均有不同程度的血、尿胆红素增高,部分伴恶心,伴或不伴皮肤巩膜黄染。
1.2方法EUS采用富士超声内镜系统SU-7000及环阵扫描超声电子内镜(EG-530UR,频率为5~12 MHz),应用直接接触法或水囊法加脱气水充盈法[4]。ERCP采用富士高清数字化电子内镜系统EPX-4450HD及ED-530XT电子十二指肠镜,行ERCP确定疾病类型并治疗。以ERCP、手术病理及随访确诊的结果为金标准,考察EUS诊断的差异。
2 结果
2.1诊断结果比较经ERCP确诊为胆总管下端结石者39例,EUS诊断38例,另1例EUS提示下端有中等回声团,后方不伴声影,诊断为胆总管下端肿瘤。ERCP及手术病理确诊为胆总管下端肿瘤10例、胆管内乳头状瘤2例、壶腹部肿瘤2例;EUS诊断结果分别为11例、0例及3例,其中1例最终确诊为胆总管下端结石者EUS误诊为胆总管下端肿瘤,2例最终确诊为胆管内乳头状瘤患者EUS将其中1例诊断为炎性狭窄,另1例诊断为壶腹部肿瘤。术后随访确诊为十二指肠乳头炎性狭窄7例,EUS诊断结果为8例,其中1例术后随访并经ERCP病理确诊为胆管内乳头状瘤。诊断正确率为95%(57/60),见表1。
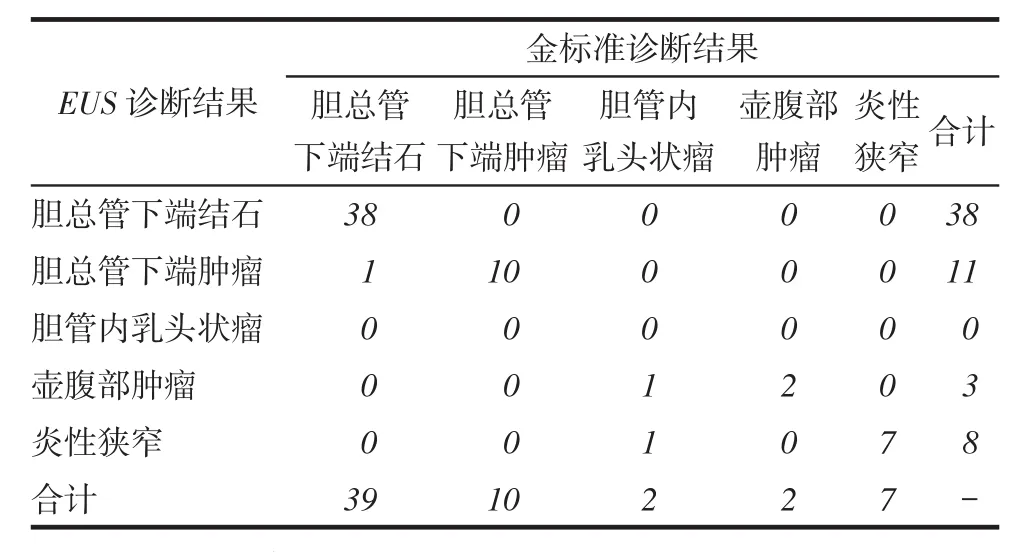
Tab.1 Comparison of the diagnostic results between EUS and gold standard表1 EUS与金标准诊断结果比较
2.2典型病例
例1男,56岁。主因右上腹不适半个月余,于2015年2月25日入本院。患者半个月前出现右上腹不适、纳差,无皮肤巩膜黄染、腹部无压痛、反跳痛,3 d前于外院CT提示胆总管下端小结节,胆囊增大:保守治疗,无明显好转。既往体健。本院TUS提示胆总管扩张(下端气体干扰显示不清)伴胆囊炎、胆囊内胆汁淤积。查MRCP提示胆总管轻度扩张,胆囊增大伴胆汁淤积,见图1A;血清胆红素轻度增高。2015年2月28日行EUS提示胆总管下端有中等回声团,后方声影不明显,考虑为胆总管下端肿瘤,见图1B;遂行ERCP插管造影下端充盈缺损影,见图1C;经内镜乳头括约肌切开术(endoscopic sphincterotomy,EST)后见一透亮结石排出,见图1D。最终诊断为胆总管下端小结石。患者ERCP 1周后行腹腔镜胆囊切除,治愈出院。
例2女,66岁。主因右上腹痛伴皮肤巩膜黄染1个月,于2015年7月10日入本院。患者1个月前出现右上腹痛伴皮肤巩膜黄染,小便色黄,腹部轻压痛、无反跳痛及肌紧张。入院检查:TUS提示胆总管轻度扩张,下段气体干扰显示不清,疑诊断为胆囊结石;CT提示胆管下端小结节,疑诊断为胆囊结石,见图2A;MRCP提示胆总管下端狭窄,疑诊断为胆囊结石,见图2B;血清总胆红素增高(49 μmol/L),直接胆红素增高(36 μmol/L),血肿瘤标志物甲胎蛋白(AFP)、癌胚抗原(CEA)均在正常范围。2015年7 月16日行EUS提示胆管下端侧生性中低回声团,见图2C;行ERCP中EST后可见壶腹背侧黏膜充血,见图2D。2015年7月24日病理检测结果最终确诊为腺癌,后行手术治疗。
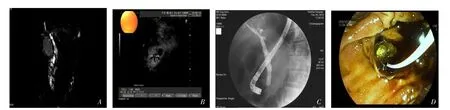
A:MRCP显示胆管扩张;B:EUS示胆总管下端中强回声,不伴声影;C:ERCPX线下下端密度减低影;D:ERCP镜下见小结石排出Fig. 1 Pictures showingendoscopic diagnosis and treatment process of small stones at the lower common bile duct图1 胆总管下端小结石诊治过程
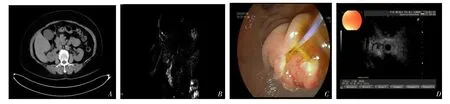
A:CT显示胆管下端小结节;B:MRCP示胆总管扩张伴下端狭窄;C:EUS显示胆总管下端侧生性中低回声团;D:ERCP中EST后病理证实为壶腹部腺癌Fig. 2 Pictures showingendoscopic diagnosis and treatment process of periampullary adenocarcinoma图2 壶腹部占位的诊治过程
3 讨论
临床中术前TUS、CT、MRCP等影像学检查胆总管扩张原因不明时,是否需要行有创的ERCP诊疗或手术治疗已成为临床棘手问题。EUS对微小病变比TUS、CT、MRI的病变检出率高,且不受肠气干扰,可在胃肠道腔内近距离观察胆胰结合部病变。Del Pozo等[5]研究显示,与ERCP、MRCP比较,EUS不仅能显示胆管、胰管形态、病变的范围,还能观察胆管及管腔外病变情况,是消化道及胆胰疾病诊断和分期的重要影像工具。另有研究显示,EUS对胆总管结石诊断的敏感性、特异性、准确率分别为94%~100%、80%~99%、93%~99%[6-8]。EUS的优点为侵入创伤性小、安全,可探测到常规TUS不能观察到的胆泥,对直径<5 mm小结石的敏感性高于CT、MRCP[9]。在英国国民健康服务(national health service,UK NHS)中,MRCP被认为是诊断胆总管结石的最经济的诊断方式,但对于被B超和CT漏诊的细小结石,治疗性ERCP在EUS检查后可有选择性地进行,从而避免十二指肠乳头的切开及可能并发症的发生[7]。中华医学会消化内镜分会2010年制定了ERCP诊治指南,也明确了EUS在治疗性ERCP中的应用价值[1]。但由于胆管结石成分构成、胆汁浓稠程度及所处位置的影响,对于回声不强、声影不明显的中等回声团,EUS的诊断存在一定的局限。本组中EUS诊断胆总管结石38例,而经ERCP确诊为胆总管下端结石并行EST和取石术者为39例,其中1例患者EUS提示下端中等回声团,后方不伴声影,诊断为胆总管下端肿瘤,后行ERCP诊断,行EST后在大量墨绿色胆汁涌出过程中发现1枚透亮结石。
通常情况下,CT对肝内、肝门区病变的诊断准确性优于EUS,对胆管内较小肿瘤显示较ERCP、MRCP差;对低位及壶腹部胆胰系肿瘤的显示需要薄层扫描,对由炎症或肿瘤所致胆管同轴型增厚定性较为困难。MRCP检查能直接客观地反映生理状态下胆胰管大小,可显示近、远侧梗阻及多发梗阻,但图像重建后小病变易被掩盖,对壶腹部改变显示较差;ERCP检查能清晰显示肝内外胆管全貌,并能在内镜下对十二指肠乳头区黏膜进行直接观察和活检[2]。EUS对胆管下端肿瘤诊断的阴性预测值高达100%;对于直径>3 cm病变的诊断敏感性可高达100%,而且大多数文献报道对于直径2~3 cm或更小的占位性病变的诊断敏感性EUS明显高于CT、MRCP[4,10-12]。李生等[10]研究显示,对于胆管下端狭窄、壶腹癌等病变,可以通过EUS从不同的角度扫查来观察病变的整体形态,有利于得出较为准确的临床诊断,可使部分患者避免行风险较高的ERCP。EUS对胰腺癌诊断准确性也明显高于其他检查方法[11]。对于十二指肠乳头、壶腹部肿瘤,EUS还可以通过内镜图像进行直观地观察,诊断准确率优于其他影像学检查[12]。本组病例2的术前影像学诊断均无病变提示,仅仅提示胆总管扩张,因此无法做出下一步治疗的计划,而通过术前EUS的诊断,行ERCP并局部活检最终确诊为腺癌。
目前,EUS对于壶腹、胆管下端病变的诊断病例数量尚少,区分壶腹、胆管下端良恶性病变的能力并不强。本例ERCP中病理诊断的2例胆管乳头状瘤患者,EUS并未能准确诊断,1例EUS提示壶腹部低回声团,诊断为壶腹部肿瘤;而另1例患者EUS诊断为炎性狭窄,术后6个月患者还出现梗阻性黄疸,复查MRCP、ERCP病理后最终确诊为胆管内乳头状瘤。因此,EUS的定位及定性诊断仍需提高。胆管远端炎性狭窄临床无法通过单纯的影像学检查确诊,EUS虽然可以比较明确地定位胆管狭窄的部位和程度,但准确性并不高,将EUS联合应用于诊断过程中,可以大大提高临床诊断的敏感性和特异性[13]。本组经随访最终确诊7例为乳头炎性狭窄。研究认为,虽然乳头炎性狭窄无特异EUS表现,但EUS对非肿瘤性疾病,如炎症性狭窄、局限性胰头炎等诊断结果较为准确[14]。
综上所述,EUS对不明原因胆总管扩张的定位及定性诊断均有很高的诊断价值,特别是能提高胆总管下端结石的确诊率,高于腹部B超、CT和(或)MRCP检查,并能指导选择性地进行ERCP,提高治疗效果,减少风险。
[1]The ERCP group,Chinese Society of Digestive Endoscopy,CSDE Practice Guidline:ERCP(2010)I[J]. Chin J Dig Endosc,2010,27 (3):113-118.[中华医学会消化内镜分会ERCP学组. ERCP诊治指南(2010版)(一)[J].中华消化内镜杂志,2010,27(3):113-118]. doi:10.3760/cma.j.issn.1007-5232.2010.03.001.
[2]Holm AN,Gerke H. What should be done with a dilated bile duct?[J]. Curr Gastroenterol,2010,12(2):150- 156. doi:10.1007/ s11894-010-0094-3.
[3]De Angelis C,Marietti M,Bruno M,et al. Endoscopic ultrasound in common bile duct dilatation with normal liverenzymes[J]. World J Gastrointest Endosc,2015,7(8):799-805. doi:10.4253/wjge.v7. i8.799. Review.
[4]Rana SS,Bhasin DK,Sharma V,et al. Role of endoscopic ultrasound in evaluation of unexplained common bile duct dilatation on magnetic esonance cholangiopancreatography[J]. Ann Gastroenterol,2013,26(1):66-70.
[5]Del Pozo D,Tabernero S,Poves E,et al.Usefulness of endoscopic ultrasonography in the clinical suspicion of biliary disease[J]. Rev Esp Enferm Dig,2011,103(7):345-348.
[6]Prachayakul V,Aswakul P,Bhunthumkomol P,et al. Diagnostic yield of endoscopic ultrasonography in patients with intermediate or high likelihood of choledocholithiasis:a retrospective study from one university-based endoscopy center[J]. BMC Gastroenterology,2014,14:165-170. doi:10.1186/1471-230X-14-165.
[7]Morris S,Gurusamy KS,Sheringham J,et al. Cost-Effectiveness analysis of endoscopic ultrasound versus magnetic resonance cholangiopancreatography in patients with suspected common bile duct stones[J]. PLoS One,2015,23,10(3):e0121699. doi:10.1371/journal. pone.0121699. g001.
[8]Ding SH,Guo HJ,Liu J,et al. Clinical value of endoscopic ultrasonography in the diagnosis of choledocholithiasis[J]. Hainan Medical Journal,2012,23(11):92-93.[丁世华,郭海建,刘俊,等.超声内镜诊断胆总管结石的临床价值[J].海南医学,2012,23(11):92-93]. doi:10.3969/j.issn.1003-6350.2012.11.039.
[9]Zhou Y,Chen X. Meta-analysis:endoscopic ultrasonography and endoscopic retrograde cholangiopancreatography in the diagnosis of choledocholithiasis[J]. Chin J Gastroenterol Hepatol,2008,17 (2):129-132.[周艳,陈翔.荟萃分析:超声内镜和ERCP诊断胆总管结石的比较[J].胃肠病学和肝病学杂志,2008,17(2):129-132]. doi:10.3969/j.issn.1006- 5709.2008.02.011.
[10]Li S,Ding BJ,Yang Y,et al. Preliminary application of endoscopic ultransonography before endoscopic retrograde cholangiopancreato graphy in suspected choledochopancreatic diseases[J]. Chin J Gastroenterol Hepatol,2013,22(4):321-323.[李生,丁百静,杨勇,等.超声内镜在可疑胆胰疾病ERCP术前的初步应用[J].胃肠病学和肝病学杂志,2013,22(4):321-323]. doi:10.3969/j.issn.1006-5709.2013.04.008.
[11]Chang KJ,Erickson RA,Chak A,et al. EUS compared with endoscopy plus transabdominal US in the initial diagnostic evaluation of patients with upper abdominal pain[J]. Gastrointest Endosc,2010,72(5):967-974. doi:10.1016/j.gie.2010.04.007.
[12]Sofi AA,Javid G,Zargar S,et al. Comparative evaluation of ERCP and endosonography in the diagnosis of extrahepatic biliary obstruction and a suggested algorithm[J]. Turk J Gastroenterol,2012,23(2):135-140. doi:10.4318/tjg.2012.0320.
[13]Zhang L,Wang ZY,Li HX.Value of endoscopic ultrasonography for differential diagnosis of benign and malignant bile duct distal stenosis[J]. Chin J Dig Endosc,2015,32(4):250-252.[张莉,王震宇,李焕喜,等.超声内镜鉴别诊断胆管下端狭窄良恶性的临床研究[J].中华消化内镜杂志,2015,32(4):250-252]. doi:10.3760/cma.j.issn.1007-5232.2015.04.008.
[14]Hao F,Qin MF,Li N. Endoscopic ultrasonography for inflammatory distal biliary stricture:Analysis of 165 cases[J]. World Chinese Journal of Digestology,2013,21(28):3008-3012.[郝芳,秦鸣放,李宁.超声内镜治疗胆道远端炎性狭窄临床分析165例[J].世界华人消化杂志,2013,21(28):3008-3012]. doi:10.11569/ wcjd.v21.i28.3008.
(2016-03-28收稿2016-04-26修回)
(本文编辑陆荣展)
The application of endoscopic ultrasonography in the diagnosis of unexplained bile duct expansion before endoscopic retrograde cholangiopancreatography
ZHANG Li1,WANG Zhenyu1,WANG Guangxia2,WANG Qing1
1 Endoscopic Diagnosis and Treatment Center,2 Ultrasonic Diagnostic Center,Tianjin Nankai Hospital,Tianjin 300100,China Corresponding Author E-mail:13312129889@163.com
Objective To evaluate the diagnostic value of endoscopic ultrasonography(EUS)for unexplained bile duct expansion in patients before retrograde cholangiopancreatography(ERCP). Methods Sixty patients with unknown causes of bile duct dilatation were included in this study. Patients were examined by abdominal ultrasound(TUS),CT and(or)magnetic resonance imaging(MRCP)suggesting the dilatation of common bile duct,suspecting biliary pancreatic disease with unknown cause. EUS diagnosis was performed before ERCP surgery. The final diagnosis was confirmed by ERCP,pathology and follow-up diagnosis. Results Thirty-nine patients were diagnosed as distal bile duct stone by ERCP,38 were diagnosed by EUS,and one case was diagnosed as common bile duct bottom tumors by EUS. There were 10 cases were diagnosed as common bile duct bottom tumors by ERCP and surgical pathology,2 cases were diagnosed as biliary papillomatosis,2 cases were diagnosed as periampullary carcinoma. There were 11,0 and 3 cases were diagnosed by EUS. One case was diagnosed as distal bile duct stone,which was diagnosed as common bile duct bottom tumor by EUS. Two cases were diagnosed as papillary tumor of the bile duct,one of which was diagnosed as inflammatory stenosis,another one was diagnosed as periampullary carcinoma by EUS. Results of postoperative follow-up confirmed that 7 cases were duodenal papilla inflammatory stenosis. Eight cases were diagnosed by EUS,one of them was followed up and pathologically diagnosed as biliary papillomatosis by ERCP. The diagnostic accuray was 95%(57/60). Conclusion EUS has higher value in the diagnosis of unexplained bile duct expansion,which especially can improve the diagnostic rate of distal bile duct stone compared with that of MRCPdetection,and can guide selectively ERCP,improve the therapeutic effect,and reduce its risk.
cholangiopancreatography,endoscopic retrograde;endoscopic ultrasonography;common bile duct expansion
R445.1
A
10.11958/20160220
1天津市,天津市南开医院内镜诊断和治疗中心(邮编300100),2超声诊断中心
张莉(1980),女,主治医师,天津中医药大学博士研究生,主要从事消化内镜诊疗
E-mail:13312129889@163.com
