ST段抬高型心肌梗死患者院内发生持续性室性心动过速/心室颤动的临床特点及其影响因素研究
2016-06-28刘文娴曹佳宁
姚 靖,刘文娴,曹佳宁
·论著·
ST段抬高型心肌梗死患者院内发生持续性室性心动过速/心室颤动的临床特点及其影响因素研究
姚 靖,刘文娴,曹佳宁
100029北京市,首都医科大学附属北京安贞医院-北京市心肺血管疾病研究所(姚靖,刘文娴,曹佳宁);北京市海淀医院 北京大学第三医院海淀院区(姚靖)
【摘要】目的分析ST段抬高型心肌梗死(STEMI)患者院内发生持续性室性心动过速(SVT)/心室颤动(VF)的临床特点及其影响因素。方法连续收集2011年8月—2013年8月首都医科大学附属北京安贞医院心内科监护病房收治的STEMI患者2 343例,入院后连续心电监测72 h以上,按照是否发生院内SVT/VF分为SVT/VF组(n=183)和无SVT/VF组(n=2 160)。回顾性分析两组患者的临床资料,记录其一般资料、实验室检查指标、冠状动脉病变及急诊血运重建情况、院内治疗情况、院内临床事件发生情况及TIMI危险评分,并采用多因素二分类logistic回归分析筛选STEMI患者院内发生SVT/VF的影响因素。结果两组患者年龄、吸烟率、高血压病史阳性率、糖尿病病史阳性率、脑血管疾病病史阳性率、陈旧性心肌梗死病史阳性率、经皮冠状动脉介入治疗(PCI)史阳性率、冠状动脉旁路移植术(CABG)史阳性率、发病至入院时间比较,差异均无统计学意义(P>0.05);SVT/VF组患者男性所占比例、冠心病家族史阳性率、心率、Killip分级Ⅲ~Ⅳ级者所占比例及左心室射血分数≤35%者所占比例高于无SVT/VF组,收缩压和舒张压低于无SVT/VF组(P<0.05)。SVT/VF组患者血红蛋白水平、中性粒细胞分数、肌酸激酶同工酶水平及估算肾小球滤过率(eGFR)<60 ml·min-1·(1.73 m2)-1者所占比例高于无SVT/VF组(P<0.05);两组患者肌钙蛋白I水平、血清K+≤3.5mmol/L者所占比例及低密度脂蛋白水平比较,差异无统计学意义(P>0.05)。SVT/VF组患者共142例完成急诊冠状动脉造影,无SVT/VF组患者共1 171例完成急诊冠状动脉造影,其中SVT/VF组患者左主干病变发生率高于无SVT/VF组、左回旋支病变发生率低于无SVT/VF组(P<0.05);两组患者左前降支、右冠状动脉病变及血管狭窄70%以上≥2支发生率比较,差异无统计学意义(P>0.05)。SVT/VF组患者前壁梗死发生率和行急诊PCI者所占比例率高于非SVT/VF组(P<0.05);两组患者下壁/右室梗死发生率比较,差异无统计学意义(P>0.05)。两组患者无一例行急诊CABG。SVT/VF组患者行静脉溶栓者所占比例、利尿剂使用率、血管活性药物使用率、行主动脉内球囊反搏(IABP)辅助治疗及持续肾脏替代治疗者所占比例高于非 SVT/VF组,β-受体阻滞剂使用率低于非 SVT/VF组,β-受体阻滞剂开始使用时间晚于非 SVT/VF组(P<0.05);两组患者阿司匹林、二磷酸腺苷(ADP)受体抑制剂、血管紧张素转换酶抑制剂/血管紧张素Ⅱ受体阻滞剂(ACEI/ARB)、硝酸酯类药物使用率及住院时间比较,差异无统计学意义(P>0.05)。A组患者心源性休克发生率和院内病死率均高于B组(P<0.05)。SVT/VF组患者TIMI危险评分高于非SVT/VF组,TIMI危险评分为8~14分者院内SVT/VF发生率高于TIMI危险评分为0~7分者(P<0.05)。多因素二分类logistic回归分析结果显示,左心室射血分数≤35%〔OR=3.58,95%CI(2.36,5.44)〕、eGFR<60 ml·min-1·(1.73 m2)-1〔OR=3.30,95%CI(2.36,4.63)〕、行急诊PCI〔OR=2.92,95%CI(2.05,4.18)〕及TIMI危险评分为8~14分〔OR=5.96,95%CI(4.03,8.80)〕是STEMI患者发生院内SVT/VF的危险因素,使用β-受体阻滞剂〔OR=0.55,95%CI(20.40,0.76)〕是STEMI患者发生院内SVT/VF的保护因素(P<0.05)。结论院内发生SVT/VF的STEMI患者多为男性,入院时心率快、血压低,心肾功能差,心源性休克及死亡发生风险高。使用β-受体阻滞剂的STEMI患者院内SVT/VF发生率较低,且心肾功能差、行急诊PCI及TIMI危险评分为8~14分的STEMI患者院内SVT/VF发生率较高,应引起临床重视。
【关键词】心肌梗死;心动过速,室性;心室颤动;影响因素分析
姚靖,刘文娴,曹佳宁.ST段抬高型心肌梗死患者院内发生持续性室性心动过速/心室颤动的临床特点及其影响因素研究[J].实用心脑肺血管病杂志,2016,24(5):11-18.[www.syxnf.net]
Yao J,Liu WX,Cao JN.Clinical features of nosocomial sustained ventricular tachycardia/ventricular fibrillation in patients with ST-segment elevation myocardial infarction and the influencing factors[J].Practical Journal of Cardiac Cerebral Pneumal and Vascular Disease,2016,24(5):11-18.
流行病学资料显示,ST段抬高型心肌梗死(ST-segment elevation myocardial infarction,STEMI)是目前导致患者院内死亡的主要原因之一,其病死率约为9.4%[1],且合并恶性心律失常是STEMI患者早期死亡的重要原因[2-3]。随着近年来诊疗技术的发展,STEMI患者病死率有所下降,但合并恶性心律失常的STEMI患者病死率仍较高。STEMI可并发多种心律失常,其中以室性心律失常较多见,包括持续性室性心动过速(sustained ventricular tachycardia,SVT)和心室颤动(ventricular fibrillation,VF)。临床研究显示,STEMI患者院内SVT/VF发生率为5%~10%,且70%~80%的SVT/VF患者会在48 h内发生心源性猝死[4-5],因此尽早识别SVT/VF高危人群并采取积极的预防措施对改善STEMI患者预后具有重要意义。本研究回顾性分析了2011年8月—2013年8月首都医科大学附属北京安贞医院心内科监护病房收治的STEMI患者的临床资料,旨在分析STEMI患者院内发生SVT/VF的临床特点及其影响因素,为STEMI的临床治疗提供参考。
1资料与方法
1.1一般资料连续收集2011年8月—2013年8月首都医科大学附属北京安贞医院心内科监护病房收治的STEMI患者2 343例,入院后连续心电监测72 h以上,按照是否发生院内SVT/VF分为SVT/VF组(n=183)和无SVT/VF组(n=2 160)。纳入标准:(1)发病至入院时间在72 h以内;(2)符合美国心脏病学院(ACC)制定的STEMI诊断标准[6];(3)年龄>18岁。排除标准:院前发生心搏骤停、进行心肺复苏者。
1.2SVT和VF的诊断标准SVT定义为室性心动过速发作时间≥30 s,或室性心动过速发作时间<30 s但进行了电复律。VF定义为心室不能规律地整体收缩,各部心肌快而不协调的颤动,心电图或心电监护不可见独立的QRS波群及T波,导致血流动力学不稳定,需要进行电除颤。
1.3研究方法回顾性分析两组患者的临床资料,记录其一般资料、实验室检查指标、冠状动脉病变及急诊血运重建情况、院内治疗情况、院内临床事件发生情况及TIMI危险评分。
1.3.1一般资料包括患者的年龄、性别、冠心病危险因素〔包括吸烟、高血压病史、糖尿病病史、脑血管疾病病史、冠心病家族史、陈旧性心肌梗死病史、经皮冠状动脉介入治疗(PCI)史、冠状动脉旁路移植术(CABG)史〕、发病至入院时间、入院时血压、心率及心功能情况(包括Killip分级和左心室射血分数),其中左心室射血分数是患者入院后24 h内行超声心动图检查并采用Simpson公式计算所得。
1.3.2实验室检查指标包括血红蛋白、中性粒细胞分数、肌酸激酶同工酶、肌钙蛋白I、血清K+、估算肾小球滤过率(eGFR)及低密度脂蛋白,其中血红蛋白、中性粒细胞分数、肌酸激酶同工酶、肌钙蛋白I及eGFR是在患者进入急诊室或心内科监护病房后即刻检测,血清K+和低密度脂蛋白是在患者入院后24 h内检测。
1.3.3冠状动脉病变及急诊血运重建冠状动脉病变包括冠状动脉病变累及血管及病变部位,急诊血运重建包括急诊PCI和急诊CABG。
1.3.4院内治疗情况包括静脉溶栓、药物治疗〔阿司匹林、二磷酸腺苷(ADP)受体抑制剂、血管紧张素转换酶抑制剂/血管紧张素Ⅱ受体阻滞剂(ACEI/ARB)、β-受体阻滞剂、β-受体阻滞剂开始使用时间、钙离子拮抗剂、利尿剂、硝酸酯类药物、血管活性药物〕、辅助治疗〔主动脉内球囊反搏(IABP)辅助治疗、持续肾脏替代治疗〕及住院时间。
1.3.5院内临床事件包括心源性休克与院内死亡。
1.3.6TIMI危险评分采集患者年龄、入院时收缩压、心率、Killip分级、体质量、前壁心肌梗死情况及发病至再灌注治疗时间,并参照TIMI危险评分标准[7]评估入院即刻TIMI危险评分。

2结果
2.1两组患者一般资料比较两组患者年龄、吸烟率、高血压病史阳性率、糖尿病病史阳性率、脑血管疾病病史阳性率、陈旧性心肌梗死病史阳性率、PCI史阳性率、CABG史阳性率、发病至入院时间比较,差异均无统计学意义(P>0.05);SVT/VF组患者男性所占比例、冠心病家族史阳性率、心率、Killip分级Ⅲ~Ⅳ级者所占比例及左心室射血分数≤35%者所占比例高于无SVT/VF组,收缩压和舒张压低于无SVT/VF组,差异均有统计学意义(P<0.05,见表1)。
2.2两组患者实验室检查指标比较SVT/VF组患者血红蛋白水平、中性粒细胞分数、肌酸激酶同工酶水平及eGFR<60 ml·min-1·(1.73 m2)-1者所占比例高于无SVT/VF组,差异有统计学意义(P<0.05);两组患者肌钙蛋白I水平、血清K+≤3.5mmol/L者所占比例及低密度脂蛋白水平比较,差异无统计学意义(P>0.05,见表2)。
2.3两组患者冠状动脉病变及急诊血运重建情况比较SVT/VF组患者共142例完成急诊冠状动脉造影,无SVT/VF组患者共1 171例完成急诊冠状动脉造影,其中SVT/VF组患者左主干病变发生率高于无SVT/VF组、左回旋支病变发生率低于无SVT/VF组,差异有统计学意义(P<0.05);两组患者左前降支、右冠状动脉病变及血管狭窄70%以上≥2支发生率比较,差异无统计学意义(P>0.05)。SVT/VF组患者前壁梗死和行急诊PCI者所占比例高于非SVT/VF组,差异有统计学意义(P<0.05);两组患者下壁/右室梗死发生率比较,差异无统计学意义(P>0.05,见表3)。两组无一例患者行急诊CABG。
2.4两组患者院内治疗情况比较SVT/VF组患者行静脉溶栓者所占比例、利尿剂使用率、血管活性药物使用率、行IABP辅助治疗及持续肾脏替代治疗者所占比例高于非 SVT/VF组,β-受体阻滞剂使用率低于非 SVT/VF组,β-受体阻滞剂开始使用时间晚于非 SVT/VF组,差异有统计学意义(P<0.05);两组患者阿司匹林、ADP受体抑制剂、ACEI/ARB、硝酸酯类药物使用率及住院时间比较,差异均无统计学意义(P>0.05,见表4)。
2.5两组患者院内临床事件比较SVT/VF组患者心源性休克发生率为35.6%,院内病死率为23.5%;无SVT/VF组患者心源性休克发生率为5.2%,院内病死率为6.8%。SVT/VF组患者心源性休克发生率和院内病死率均高于无SVT/VF组,差异有统计学意义(χ2值分别为64.735、216.182,P<0.05)。
2.6两组患者TIMI危险评分比较SVT/VF组患者TIMI危险评分为9(7,10)分,无SVT/VF组患者TIMI危险评分为7(6,9)分,SVT/VF组患者TIMI危险评分高于非SVT/VF组,差异有统计学意义(Z=-2.432,P=0.015);以TIMI危险评分8分为临界值,TIMI危险评分为8~14分者院内SVT/VF发生率高于TIMI危险评分为0~7分者〔28.8%(44/153)比6.3%(139/2 190)〕,差异有统计学意义(χ2=99.754,P<0.001)。
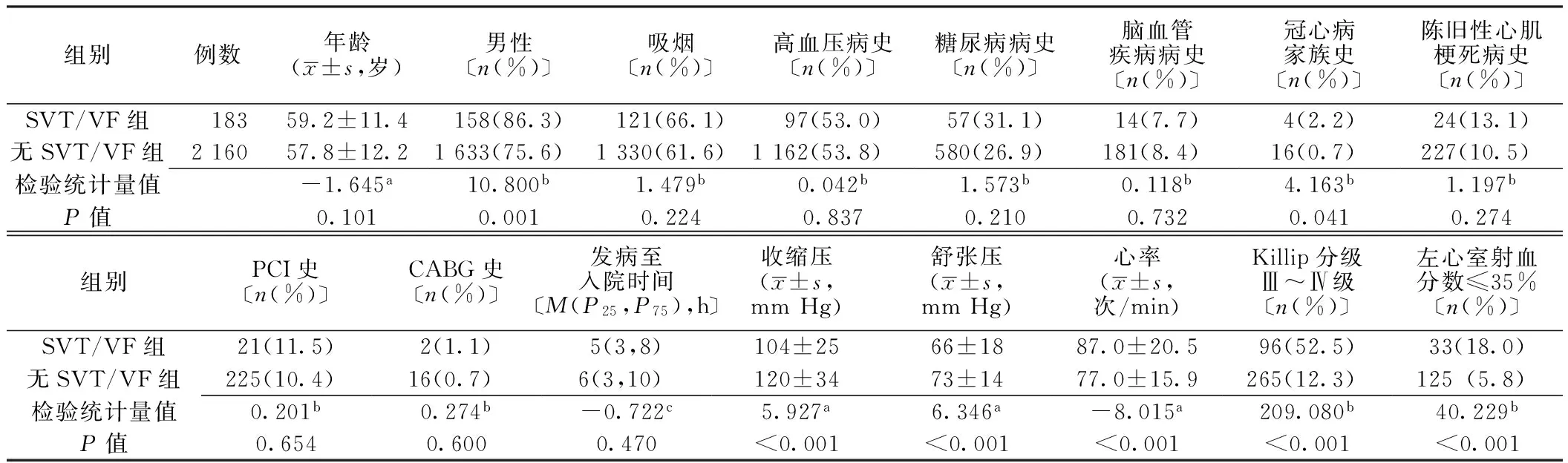
表1 两组患者一般资料比较
注:SVT=持续性室性心动过速,VF=心室颤动,PCI=经皮冠状动脉介入治疗,CABG=冠状动脉旁路移植术;a为t值,b为χ2值,c为Z值
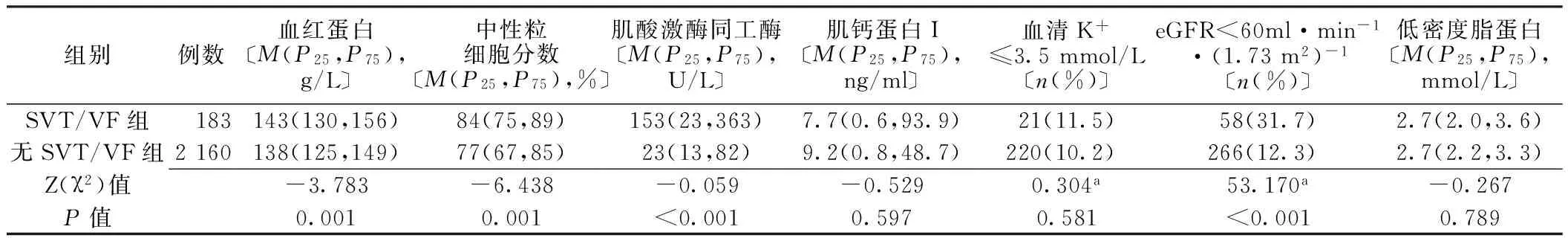
表2 两组患者实验室检查指标比较
注:eGFR=估算肾小球滤过率;a为χ2值

表3 两组患者冠状动脉病变及急诊血运重建情况比较〔n(%)〕
注:a为完成急诊冠状动脉造影患者例数,其中SVT/VF组为142例,无SVT/VF组为1 171例
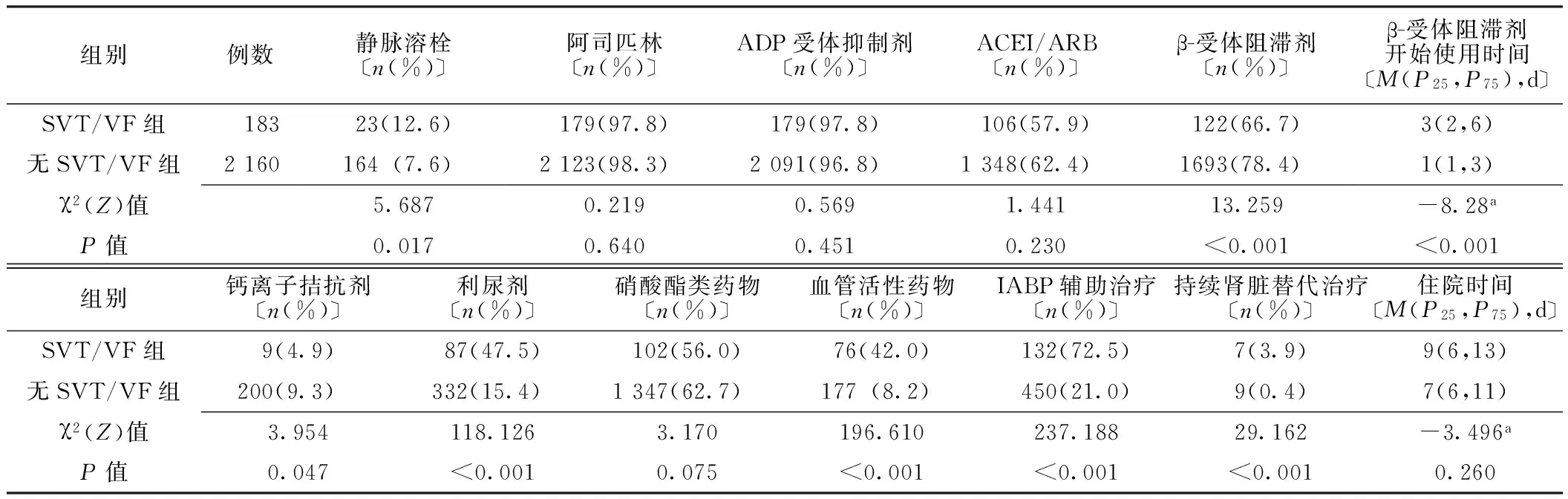
表4 两组患者院内治疗情况比较
注:ADP=二磷酸腺苷,ACEI/ARB=血管紧张素转换酶抑制剂/血管紧张素Ⅱ受体阻滞剂,IABP=主动脉内球囊反搏;a为Z值
2.7STEMI患者发生院内SVT/VF的影响因素分析将院内SVT/VF作为因变量,将一般资料、实验室检查指标、冠状动脉病变及急诊血运重建情况、院内治疗情况中有统计学差异的指标及TIMI危险评分作为自变量(变量赋值见表5)纳入多因素二分类logistic回归分析,结果显示,左心室射血分数≤35%、eGFR<60 ml·min-1·(1.73 m2)-1、行急诊PCI及TIMI危险评分为8~14分是STEMI患者发生院内SVT/VF的危险因素,使用β-受体阻滞剂是STEMI患者发生院内SVT/VF的保护因素(P<0.05,见表6)。
表6STEMI患者发生院内SVT/VF影响因素的多因素二分类logistic回归分析
Table 6Multivariate binary logistic regression analysis on influencing factors of nosocomial SVT/VF in patients with STEMI
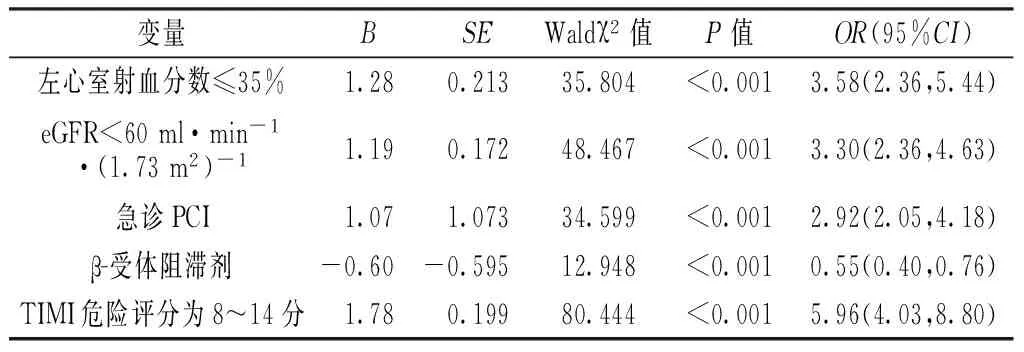
变量BSEWaldχ2值P值OR(95%CI)左心室射血分数≤35%1.280.21335.804<0.0013.58(2.36,5.44)eGFR<60ml·min-1·(1.73m2)-11.190.17248.467<0.0013.30(2.36,4.63)急诊PCI1.071.07334.599<0.0012.92(2.05,4.18)β-受体阻滞剂-0.60-0.59512.948<0.0010.55(0.40,0.76)TIMI危险评分为8~14分1.780.19980.444<0.0015.96(4.03,8.80)
注:因自变量较多,未将无影响变量的多因素二分类logistic回归分析结果列出

表5 变量赋值
3讨论
STEMI是心血管急危重症。尽管心肌梗死治疗技术不断发展,但心肌梗死后发生SVT/VF仍是患者死亡的重要原因。流行病学资料显示,STEMI患者院内SVT/VF发生率为5%~10%[3],本研究结果(7.8%)与之相符。虽然我国经济发达地区已进入急诊PCI时代,但本研究结果显示仅有55.9%的患者行急诊PCI,且SVT/VF组患者行急诊PCI者所占比例和院内病死率均高于无SVT/VF组,推测院内发生SVT/VF可能是导致患者死亡风险升高的原因,应引起临床医师的高度重视。
既往研究指出,STEMI患者发生SVT/VF是由多因素共同作用所致。本研究通过分析STEMI院内发生SVT/VF患者的临床特点发现,院内SVT/VF多发于男性STEMI患者,且患者入院时生命体征不稳定(心率快、血压低)、心功能差、肾功能不全、病情危重。分析原因可能为入院时患者除因心功能不全导致心率代偿性增快外,疼痛与紧张所致的交感神经过度兴奋同样会导致心率增快,易诱发SVT/VF[8]。SVT/VF发生后心脏不能正常射血,严重影响心、肾等器官和周围组织的血流灌注,导致患者病情进一步加重。本研究进一步分析冠状动脉病变情况发现,STEMI院内发生SVT/VF患者病变多累及左主干,且多为前壁梗死。既往有研究证实,SVT/VF的发生与心肌梗死面积及LVEF有关[3,9-10],且院内发生SVT/VF的患者心源性休克及院内死亡风险明显升高,本研究结果与之一致。本研究结果显示,SVT/VF组患者行静脉溶栓者所占比例、利尿剂使用率、血管活性药物使用率、行IABP辅助治疗及持续肾脏替代治疗者所占比例高于非 SVT/VF组,提示发生院内SVT/VF的患者病情更加危重,与其他研究结果相一致[11-12],但即便及时进行有效的血运重建结合IABP辅助治疗及持续肾脏替代治疗,SVT/VF患者预后仍不容乐观。
为了筛选院内发生SVT/VF的高危STEMI患者,本研究采用多因素二分类logistic回归模型进行分析,结果显示左心室射血分数≤35%、eGFR<60 ml·min-1·(1.73 m2)-1、行急诊PCI及TIMI危险评分为8~14分是STEMI患者发生院内SVT/VF的危险因素,使用β-受体阻滞剂是STEMI患者发生院内SVT/VF的保护因素。
左心室射血分数≤35%提示患者存在左心室功能减退现象,而左心室功能减退患者心肌血流灌注受限、电机械同步性降低,可能会诱导SVT/VF的发生。有研究显示,急性心肌梗死后肌酐清除率升高与肾前性灌注不足有关,eGFR是评价急性肾损伤的临床指标,急性肾损伤可能导致包括SVT/VF在内的院内不良事件的发生。
目前以急诊PCI为主的早期再灌注治疗仍是STEMI的主要治疗方法,且大量文献证实,血运重建是有效降低STEMI患者近期病死率及改善患者长期预后的有效措施[13-14]。与未发生SVT/VT的患者相比,完成急诊PCI前发生SVT/VT的患者病死率增加2倍,完成急诊PCI后发生SVT/VT的患者病死率增加5倍[3,9-10],提示急诊PCI术后发生SVT/VF的患者死亡风险更高,分析原因可能与行急诊PCI后患者心功能较差、血流动力学不稳定有关。结合ACC/美国心脏协会(AHA)及欧洲心脏病学会(ESC)制定的指南,对于血流动力学不稳定患者,在条件允许情况下应尽快行以急诊PCI为主的血运重建[6,15-16],且急诊PCI的时间窗可以相应放宽。
2012年ESC及2013年美国心脏病学会基金会/ACCF/AHA发布的STEMI指南指出,危险评分有利于判断患者临床预后、进行危险分层及选择最佳治疗方案,故应对急性心肌梗死患者进行危险评分[6,15]。TIMI危险评分是以临床资料为主要内容的危险评分模型,能有效预测STEMI患者和接受介入治疗患者的短期病死率[7,17]。Morrow等[17]研究发现,STEMI患者TIMI危险评分与其近期病死率呈正相关,TIMI危险评分为8分的患者属于高危患者,且TIMI危险评分为8分的患者短期病死率是TIMI危险评分为0分患者的40倍。本研究结果显示,TIMI危险评分为8~14分者院内SVT/VF发生率高于TIMI危险评分为0~7分者,提示TIMI危险评分高的STEMI患者院内SVT/VF发生率高TIMI危险评分包含Killip分级、前壁心肌梗死及发病至再灌注时间,且既往研究显示Killip分级、前壁心肌梗死及发病至再灌注时间与SVT/VF的发生有关。
2005年进行的COMMIT试验结果提示,心肌梗死患者早期使用β-受体阻滞剂可有效降低VF及再梗死发生率。自2007年起,AHA发布的STEMI和NST-ACS指南指出,在无禁忌证情况下应及早应用β-受体阻滞剂[18-19]。大量研究结果证实,使用β-受体阻滞剂者心血管病死率明显降低,且在用药12~24 h内即开始见效,提示早期使用β-受体阻滞剂可降低患者短期病死率[20-21]。本研究结果显示,SVT/VF组患者β-受体阻滞剂使用率低于非SVT/VF组,β-受体阻滞剂开始使用时间晚于非SVT/VF组,且多因素二分类logistic回归分析结果显示,使用β-受体阻滞剂是STEMI患者院内发生SVT/VF的保护因素。分析原因可能有两个方面:一方面是由于未发生SVT/VF的患者病情相对稳定,心功能较好,可耐受早期使用β-受体阻滞剂;另一方面与β-受体阻滞剂可抑制交感神经及控制心率、心律有关。β-受体阻滞剂的关键作用是阻滞β-受体,保护性降低交感神经张力,降低血浆去甲肾上腺素水平,增加心脏迷走神经兴奋性,从而抑制SVT/VF的发生。
综上所述,院内发生SVT/VF的STEMI患者多为男性,入院时心率快、血压低,心肾功能较差,心源性休克及死亡发生风险高。左心室射血分数≤35%、eGFR<60 ml·min-1·(1.73 m2)-1、行急诊PCI及TIMI评分为8~14分是STEMI患者发生院内SVT/VF的危险因素,使用β-受体阻滞剂是STEMI患者发生院内SVT/VF的保护因素。但本研究为回顾性、单中心、非随机抽样研究,故存在一定的选择偏倚,可能会影响研究结果;此外,本研究未能收集患者住院期间病情变化资料,未对院内SVT/VF的发生进行动态评估。
作者贡献:姚靖进行实验设计与实施、资料收集整理、撰写论文、成文并对文章负责;曹佳宁进行实验实施、评估、资料收集;刘文娴进行质量控制及审校。
本文无利益冲突。
参考文献
[1]Goldberg RJ,Spencer FA,Gore JM,et al.Thirty-year trends(1975 to 2005) in the magnitude of,management of,and hospital death rates associated with cardiogenic shock in patients with acute myocardial infarction: a population-based perspective[J].Circulation,2009,119(9):1211-1219.
[2]张秀英,赵冬,王薇,等.2007年至2009年北京市居民急性心肌梗死住院病死率及其分布特征的研究[J].心肺血管病杂志,2012,31(1):1-4.
[3]Mehta RH,Starr AZ,Lopes RD,et al.Incidence of and outcomes associated with ventricular tachycardia or fibrillation in patients undergoing primary percutaneous coronary intervention[J].JAMA,2009,301(17):1779-1789.
[4]Lee KL,Woodlief LH,Topol EJ,et al.Predictors of 30-day mortality in the era of reperfusion for acute myocardial infarction.Results from an international trial of 41,021 patients.GUSTO-I Investigators[J].Circulation,1995,91(6):1659-1668.
[5]Piccini JP,Hranitzky PM,Kilaru R,et al.Relation of mortality to failure to prescribe beta blockers acutely in patients with sustained ventricular tachycardia and ventricular fibrillation following acute myocardial infarction(from the VALsartan In Acute myocardial iNfarcTion trial[VALIANT] Registry)[J].Am J Cardiol,2008,102(11):1427-1432.
[6]O′Gara PT,Kushner FG,Ascheim DD,et al.2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines[J].J Am Coll Cardiol,2013,61(4):e78-140.
[7]Morrow DA,Antman EM,Parsons L,et al.Application of the TIMI risk score for ST-elevation MI in the National Registry of Myocardial Infarction 3[J].JAMA,2001,286(11):1356-1359.
[8]Honda T,Kanazawa H,Koga H,et al.Heart rate on admission is an independent risk factor for poor cardiac function and in-hospital death after acute myocardial infarction[J].J Cardiol,2010,56(2):197-203.
[9]Jabbari R,Engstrom T,Glinge C,et al.Incidence and risk factors of ventricular fibrillation before primary angioplasty in patients with first ST-elevation myocardial infarction: a nationwide study in Denmark[J].J Am Heart Assoc,2015,4(1):e001399.
[10]Al-Khatib SM,Stebbins AL,Califf RM,et al.Sustained ventricular arrhythmias and mortality among patients with acute myocardial infarction:results from the GUSTO-III trial[J].Am Heart J,2003,145(3):515-521.
[11]曹佳宁,刘文娴.主动脉内球囊反搏术在ST段抬高型心肌梗死患者中不同TIMI评分的疗效分析[J].心肺血管病杂志,2014,33(6):808-812.
[12]Rihal CS,Naidu SS,Givertz MM,et al.2015 SCAI/ACC/HFSA/STS Clinical Expert Consensus Statement on the Use of Percutaneous Mechanical Circulatory Support Devices in Cardiovascular Care: Endorsed by the American Heart Association,the Cardiological Society of India,and Sociedad Latino Americana de Cardiologia Intervencionista;Affirmation of Value by the Canadian Association of Interventional Cardiology-Association Canadienne de Cardiologie d′intervention[J].J Am Coll Cardiol,2015,65(19):2140-2141.
[13]van Domburg RT,Sonnenschein K,Nieuwlaat R,et al.Sustained benefit 20 years after reperfusion therapy in acute myocardial infarction[J].J Am Coll Cardiol,2005,46(1):15-20.
[14]Grzybowski M,Clements EA,Parsons L,et al.Mortality benefit of immediate revascularization of acute ST-segment elevation myocardial infarction in patients with contraindications to thrombolytic therapy: a propensity analysis[J].JAMA,2003,290(14):1891-1898.
[15]Steg PG,James SK,Atar D,et al.ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation[J].Eur Heart J,2012,33(20):2569-2619.
[16]Hochman JS,Sleeper LA,Webb JG,et al.Early revascularization in acute myocardial infarction complicated by cardiogenic shock.SHOCK Investigators.Should We Emergently Revascularize Occluded Coronaries for Cardiogenic Shock[J].N Engl J Med,1999,341(9):625-634.
[17]Morrow DA,Antman EM,Charlesworth A,et al.TIMI risk score for ST-elevation myocardial infarction: A convenient,bedside,clinical score for risk assessment at presentation: An intravenous nPA for treatment of infarcting myocardium early II trial substudy[J].Circulation,2000,102(17):2031-2037.
[18]Antman EM,Hand M,Armstrong PW,et al.2007 Focused Update of the ACC/AHA 2004 Guidelines for the Management of Patients With ST-Elevation Myocardial Infarction:a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines:developed in collaboration With the Canadian Cardiovascular Society endorsed by the American Academy of Family Physicians:2007 Writing Group to Review New Evidence and Update the ACC/AHA 2004 Guidelines for the Management of Patients With ST-Elevation Myocardial Infarction,Writing on Behalf of the 2004 Writing Committee[J].Circulation,2008,117(2):296-329.
[19]Anderson JL,Adams CD,Antman EM,et al.ACC/AHA 2007 guidelines for the management of patients with unstable angina/non-ST-Elevation myocardial infarction:a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines(Writing Committee to Revise the 2002 Guidelines for the Management of Patients With Unstable Angina/Non-ST-Elevation Myocardial Infarction) developed in collaboration with the American College of Emergency Physicians,the Society for Cardiovascular Angiography and Interventions,and the Society of Thoracic Surgeons endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation and the Society for Academic Emergency Medicine[J].J Am Coll Cardiol,2007,50(7):e1-157.
[20]DiNicolantonio JJ,Fares H,Niazi AK,et al.beta-Blockers in hypertension,diabetes,heart failure and acute myocardial infarction:a review of the literature[J].Open Heart,2015,2(1):e000230.
[21]Zhang H,Masoudi FA,Li J,et al.National assessment of early beta-blocker therapy in patients with acute myocardial infarction in China,2001—2011: The China Patient-centered Evaluative Assessment of Cardiac Events(PEACE)-Retrospective AMI Study[J].Am Heart J,2015,170(3):506-515.e1.
(本文编辑:谢武英)
Clinical Features of Nosocomial Sustained Ventricular Tachycardia/Ventricular Fibrillation in Patients With ST-segment Elevation Myocardial Infarction and the Influencing Factors
YAOJing,LIUWen-xian,CAOJia-ning.
InstituteforHeartLungandBloodVesselDiseases,CapitalMedicalUniversityAffiliatedBeijingAnzhenHospital,Beijng100029,China
【Abstract】ObjectiveTo analyze the clinical features of nosocomial sustained ventricular tachycardia(SVT)/ventricular fibrillation(VF)in patients with ST-segment elevation myocardial infarction(STEMI) and the influencing factors.MethodsFrom August 2011 to August 2013,a total of 2 343 patients with STEMI were selected in the CCU of Capital Medical University Affiliated Beijing Anzhen Hospital,all of them received electrocardiogram monitoring for over 72 hours,and they were divided into A group(complicated with SVT/VF,n=183 )and B group(did not complicated with SVT/VF,n=2 160)according to the incidence of nosocomial SVT/VF.General information,laboratory examination results,coronary artery lesions,emergency revascularization,nosocomial treatment,incidence of nosocomial clinical events and TIMI risk score were compared between the two groups,and multivariate binary logistic regression analysis was used to analyze the influencing factors of nosocomial SVT/VF in patients with STEMI.ResultsNo statistically significant differences of age,smoking rate,positive rate of hypertension history,diabetes history,cerebrovascular disease history,old myocardial infarction history,PCI history or CABG history,or duration between attack and admission was found between the two groups(P>0.05);the proportion of male,positive rate of family history of coronary heart disease,heart rate,the proportion of patients with Ⅲ- to Ⅳ-grade Killip grades and patients with LVEF below or equal 35% of A group were statistically significantly higher than those of B group,while SBP and DBP of A group were statistically significantly lower than those of B group(P<0.05).Hb,neutrophils percentage,CK-MB and the proportion of patients with eGFR below 60 ml·min-1·(1.73 m2)-1of A group were statistically significantly higher than those of B group(P<0.05),while no statistically significant differences of cTnI,the proportion of patients with serum K+ below or equal 3.5mmol/L or LDL was found between the two groups(P>0.05).Of A group,142 cases completed the emergency coronary angiography;of B group,1 171 cases completed the emergency coronary angiography.The incidence of left main coronary artery lesion of A group was statistically significantly higher than that of B group,the incidence of left circumflex artery lesion of A group was statistically significantly lower than that of B group(P<0.05);while no statistically significant differences of incidence of left anterior descending branch lesion,right coronary artery lesion or equal or over 2 branches with over 70% stenosis was found between the two groups(P>0.05).The incidence of anterior myocardial infarction and the proportion of patients undergoing emergency PCI of A group were statistically significantly higher than those of B group(P<0.05),while no statistically significant differences of incidence of inferior myocardial infarction or right ventricular infarction was found between the two groups(P>0.05).No one of two groups received emergency CABG.The proportion of patients undergoing intravenous thrombolysis,usage rates of diuretics and vasoactive drugs,the proportion of patients undergoing IABP and continuous renal replacement therapy of A group were statistically significantly higher than those of B group,usage rates of beta adrenergic receptors of A group was statistically significantly lower than that of B group,the time for using beta adrenergic receptor of A group was statistically significantly later than that of B group(P<0.05);no statistically significant differences of usage rate of aspirin,adenosine diphosphate receptor inhibitors,ACEI/ARB or nitrates,or hospital stays was found between the two groups(P>0.05).The incidence of cardiac shock and mortality rate of A group were higher than those of B group(P>0.05).TIMI risk score of A group was statistically significantly higher than that of B group,and the incidence of nosocomial SVT/VF of patients with TIMI risk score at 8 to 14 was statistically significantly higher than that of patients with TIMI risk score at 0 to 7(P<0.05).Multivariate binary logistic regression analysis showed that,LVEF below or equal 35%〔OR=3.58,95%CI(2.36,5.44)〕,eGFR below 60 ml·min-1·(1.73 m2)-1〔OR=3.30,95%CI(2.36,4.63)〕,emergency PCI〔OR=2.92,95%CI(2.05,4.18)〕 and TIMI risk score at 8 to 14〔OR=5.96,95%CI(4.03,8.80)〕 were risk factors of nosocomial SVT/VF in patients with STEMI,while usage of beta adrenergic receptors was the protective factor(P<0.05).ConclusionMale patients with STEMI have high risk of nosocomial SVT/VF,nosocomial SVT/VF patients with faster heart rate and lower blood pressure at admission,poor heart and kidney function,and high risk of cardiac shock and death.Beta adrenergic receptors can reduce the incidence of nosocomial SVT/VF,STEMI patients with poor heart and kidney function,undergoing emergency PCI and with TIMI risk score at 8 to 14 have high risk of of nosocomial SVT/VF,should pay more attentions.
【Key words】Myocardial infarction;Tachycardia,ventricular;Ventricular fibrillation; Root cause analysis
通信作者:刘文娴,100029北京市,首都医科大学附属北京安贞医院-北京市心肺血管疾病研究所;E-mail:liuwenxian@medmail.com.cn
【中图分类号】R 542.22
【文献标识码】A
doi:10.3969/j.issn.1008-5971.2016.05.003
(收稿日期:2016-03-05;修回日期:2016-05-16)
【编者按】心律失常是心肌梗死患者的常见并发症之一,且并发心律失常的心肌梗死患者死亡风险明显增高;仅在2014—2015这一年当中,中国、美国及欧洲多国连续发表了若干ST段抬高型心肌梗死(STEMI)治疗指南,且各指南中均或多或少涉及了STEMI伴心律失常的治疗,STEMI伴心律失常的管理已成为近年来研究热点之一。姚靖等学者通过收集2 343例STEMI患者的临床资料,探讨了其院内持续性室性心动过速/心室颤动发生情况、临床特征及影响因素等,观察指标全面、系统,具有较高的参考价值,可指导临床STEMI伴心律失常预防策略的制定,敬请关注!
