自锁式零切迹椎间融合器治疗多节段颈椎病及其中长期随访
2016-04-12王泽徐沁同孟德华费琴明张键
王泽 徐沁同 孟德华 费琴明 张键
(复旦大学附属中山医院骨科, 上海 200032)
·论著·
自锁式零切迹椎间融合器治疗多节段颈椎病及其中长期随访
王泽徐沁同孟德华费琴明张键
(复旦大学附属中山医院骨科, 上海200032)
摘要目的: 探讨自锁式零切迹椎间融合器治疗多节段颈椎病的可行性及中长期临床疗效。方法: 选择2010年10月—2013年4月接受前路椎间盘切除,新融合器植骨,处理至少3个节段的多节段颈椎病患者34例,采用日本骨科学会(Japanese Orthopedic Association,JOA)评分及颈椎功能障碍指数(neck disability index,NDI)评价患者术前、术后3个月、术后12个月及末次随访时神经及颈椎功能恢复情况;X线评价各时点颈椎前凸角恢复、颈椎间隙高度恢复情况,并与术前相比较;三维CT评价术后6个月、12个月植骨融合情况;Odom评价体系评价术后患者满意度情况。结果: 患者随访18~30个月,平均24.3个月。患者术后3个月,术后12个月及末次随访时JOA评分、NDI评分与术前比较差异均有统计学意义(P<0.05);术后各时点X线提示颈椎整体前凸角、椎间隙高度均较术前改善(P<0.05),且随访期间维持良好。术后6个月CT显示确切融合率为62.4%,总融合率85.1%;术后12个月确切融合率为93.1%,总融合率100%。优良率为88.2%(30/34)。结论: 颈椎自锁式零切迹椎间融合器可应用于多节段颈椎前路减压植骨融合术中,能有效维持颈椎大范围减压后的整体曲度及椎间隙高度,保证植骨融合的成功,临床疗效满意。
关键词自锁定;椎间融合器;颈椎病
Clinical Analysis as Well as Mid-Term and Long-Term Follow-Up Results of Self-Locking and Zero-Profile Interbody Fusion Cage for the Treatment of Multi-Segmental Cervical Spondylosis
WANGZeXUQintongMENGDehuaFEIQinmingZHANGJian
DepartmentofOrthopedics,ZhongshanHospital,FudanUniversity,Shanghai200032,China
AbstractObjective: To explore the feasibility as well as mid-term and long-term clinical efficacy of self-locking and zero-profile cage for the treatment of multi-segmental cervical spondylosis.Methods: A total of 34 patients with cervical spondylosis, who received anterior cervical discectomy and fusion(ACDF) with new fusion cage for at least three segments during Oct. 2010 and Apr. 2013, were enrolled.The neural and cervical function was evaluated with Japanese Orthopedic Association(JOA) scores and neck disability index(NDI) before surgery, 3 months after surgery, 12 months after surgery and at the last follow-up.Meanwhile,the cervical curvature and intervertebral height were evaluated by X-ray at each time point and then compared with that before surgery.And the condition of cervical fusion was assessed by three-dimensional computed tomography scan. Furthermore, dom evaluation system was used to evaluate patients′ satisfaction after operation.Results: The follow-up averaged 24.3 months (range 18-30 months).There were significant differences between the JOA and NDI scores at the 3rd,12th month after operation and the last follow-up and that at preoperative point(P<0.05).The angles of cervical curvature and intervertebral height were improved postoperatively (P<0.05) and maintained throughout the follow-up.CT scan demonstrated that the precise fusion rate and the total fusion rate were 62.4% and 85.1% respectively at the 6th month after operation. And the precise fusion rate, the total fusion rate, the excellent and good rate were 93.1%, 100%, and 88.2%(30/34), respectively, at the 12th month after operation.Conclusions: The self-locking and zero-profile cervical cage could be applied in multi-segmental ACDF. It could maintain the cervical curvature as well as the intervertebral height after wide rage decompression, and assure the success of fusion as well as the satisfactory outcome.
Key WordsSelf-locking;Interbody fusion cage;Cervical spondylosis
颈椎前路减压植骨融合术(anterior cervical discectomy and fusion,ACDF)已成为保守治疗无效的退变性颈椎病的常规术式。ACDF在解除神经压迫的同时,可恢复和维持椎间隙高度及颈椎的生理曲度,近远期效果肯定。然而,随着手术节段的增多,椎间融合失败的风险逐渐增加。颈椎前路钢板技术的确可以为术后的颈椎提供即刻稳定性,也可多少降低近远期融合失败的风险[1-2],但也可增加手术风险和创伤,如术后吞咽困难、血管神经损伤、颈椎曲度不良、内固定失败等并发症[3]。自锁式零切迹椎间融合器则具有使用方便、手术损伤小的特点,临床实践疗效尚佳,但文献报道多限于单节段和2节段颈椎病的ACDF,然而,对于多节段颈椎病手术的研究较少。本研究应用自锁式零切迹椎间融合器行ACDF处理至少3个节段的多节段颈椎病患者,临床疗效满意,现报告如下。
1资料与方法
1.1一般资料选择2010年10月—2013年4月接受自锁式零切迹椎间融合器(RIO-C,法国LDR公司)治疗的多节段颈椎病手术患者34例,其中男性22例,女性12例;年龄43~75岁,平均61.2岁,手术节段共101节段;随访时间为18~30个月,平均24.3个月。患者接受X线、MRI或CT检查,结合病史及体检诊断明确。颈椎病分类包括神经根型4例,脊髓型20例,混合型10例;3节段病变27例,4节段病变7例;连续性节段病例30例,跳跃性节段病例4例。纳入标准:(1)影像学检查提示脊髓受压至少3个节段或以上,且影像学检查所示的病变节段可解释临床症状及体征;(2)脊髓受压主要来自腹侧,可用前路技术完成减压操作。排除标准:(1)颈椎管狭窄、后纵韧带骨化、单纯前路手术无法完成减压操作的病例;(2)既往接受过颈部手术或翻修病例;(3)患者一般条件差,无法耐受麻醉及手术治疗。
1.2手术方法患者全身麻醉后,颈伸仰卧位,取右侧胸锁乳突肌前缘纵行切口约5 cm,逐层分离,经血管-内脏鞘间隙,显露椎前间隙,纵行分开颈长肌及前纵韧带,X线透视确认病变节段。使用撑开器撑开椎间隙,切除病变椎间盘,再用刮匙清理椎体后缘骨赘,切除后纵韧带,彻底减压硬膜囊,探查钩椎关节及神经根出口,必要时一并减压。刮除软骨终板至骨面渗血,完成植骨床准备。选取大小、弧度匹配的融合器型号,试模满意后取自体髂骨松质骨或混合部分同种异体骨填充融合器,打入椎间隙,X线透视提示椎间隙高度及颈椎弧度恢复良好后,将锁定插片打入椎体内,留置引流管,缝合切口。术后佩戴颈托制动至少6周。
1.3术后评价指标
1.3.1术中、术后并发症术后吞咽困难情况:采用Bazaz等[4]提出的标准进行评估;采用日本骨科学会(Japanese Orthopedic Association,JOA)评分系统评价患者术前、术后3个月、术后12个月及末次随访时神经功能恢复情况;采用颈椎功能障碍指数(neck disability index,NDI)评价患者术前、术后3个月、术后12个月及末次随访时颈椎功能恢复情况;采用Odom评价体系评价患者术后满意度。
1.3.2影像学评价所有测定均在院内影像工作站内完成[5-6]。颈椎整体曲度:测定患者术前、术后3个月、术后6个月及末次随访时颈椎侧位X线片上颈椎整体前凸角,即测定颈2椎体下缘与颈7椎体下缘垂线的夹角;颈椎间隙高度:测定患者术前、术后3 d、术后3个月、术后6个月及末次随访时颈椎侧位X线片上颈椎每个手术节段椎间隙高度,即测定手术节段相邻椎体上下终板中点的距离;融合情况:患者术后6个月、12个月接受三维CT检查,按照Singh等[6]的标准判读,结果分为确切融合、可能融合、融合情况不确定以及未融合4类,确切融合率=确切融合例数/总例数×100%,总融合率=(确切融合例数+可能融合例数)/总例数×100%。

2结果
2.1临床评价
2.1.1并发症术中未发生神经、血管、气管及食管等组织损伤;术区及取骨区无切口不良反应发生。1例患者出现髂骨取骨处疼痛,半年后自愈。术后未出现融合器脱出、下沉病例,无翻修病例出现。
2.1.2术后吞咽困难术后发生中度吞咽困难2例,轻度吞咽困难4例,无重度吞咽困难发生,末次随访时仍有1例患者诉偶伴有进食时咽喉部异物感。
2.1.3JOA评分术后3个月、术后12个月、末次随访时JOA评分与术前比较差异均有统计学意义(P<0.05),其中术后各时点JOA评分比较差异无统计学意义,见表1。
2.1.4NDI评分术后3个月、术后12个月、末次随访时NDI评分与术前比较差异均有统计学意义(P<0.05),其中术后各时点NDI评分比较差异无统计学意义,见表1。
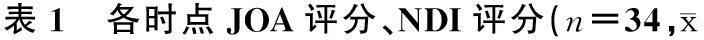
±s)
注:与术前比较,*P<0.05
2.1.5患者满意度优20例,良10例,一般3例,差1例,优良率为88.2%(30/34)。
2.2影像学评价术后3个月、术后12个月、末次随访时,各时点颈椎整体前凸角、颈椎间隙高度较术前均有改善(P<0.05),末次随访改善情况较术后6个月稍差,但差异无统计学意义,见表2。术后6个月确切融合节段63个,可能融合23个,融合情况不确定10个,未融合节段5个,确切融合率为62.4%,总融合率85.1%;术后12个月确切融合节段94个,可能融合7个,确切融合率为93.1%,总融合率100%。

表2 各时点颈椎整体前凸角(n=34)
注:与术前比较,*P<0.05
2.3典型病例患者男性,59岁,脊髓型颈椎病,术前CT示C3~C6节段椎间盘突出,见图1A;出院前X线示融合器在位,颈椎生理曲度改善,见图1B;术后3个月X线示融合器在位,见图1C;术后12个月CT示椎间植骨已融合,见图1D。

A:术前CT;B:出院前X线;C:术后3个月X线;D:术后12个月CT图1 脊髓型颈椎病患者术前、术后影像
3讨论
椎间融合器应用于颈椎前路手术中,具有重建颈椎生理曲度、维持椎间隙及椎间孔高度的特点,可一定程度上提高融合率。但大多数椎间融合器的稳定支撑作用源于术中与椎间隙间的静力压,单独使用仅适用于涉及1~2个手术节段的颈椎病病例[7]。Shimamoto等[8]的研究发现,超过3个节段时,即使对终板进行细致处理,单纯的椎间融合器也无法提供术后即刻稳定,需要额外的内固定或外固定支持。随着手术节段的增加,融合器移位和沉降的风险也逐渐增加,远期对临床疗效的维持不利。相关报道[9-10]也证实了加用前路钢板之后患者的临床获益。然而,安置前路钢板的操作需要扩大术野的范围,增加了组织损伤的风险,近远期亦存在内固定失败的可能,而术后钢板相关性的吞咽功能不良问题也逐渐引起了临床的重视[11]。
随着自锁式零切迹椎间融合器的问世,有关该类融合器应用于颈椎病的报道不断出现,有文献[12]提示其临床疗效可以跟传统钢板内固定融合技术媲美。但文献报道多集中于单节段或2节段的病例,应用于多节段颈椎病中的长期随访研究较少。本组病例单纯采用自锁式零切迹椎间融合器治疗至少3节段的多节段颈椎病,其嵌片技术可将融合器固定在邻位椎体上,无需额外的钢板固定即可达到术后即刻稳定效果,从而降低了融合器移位、下沉的风险,随访期间X线提示颈椎曲度维持良好,椎间隙高度较术后即刻未见明显改变;简易的操作也允许术者无需过度牵开周围组织即可完成,围手术期未出现神经血管损伤等并发症,也避免了钢板内固定置入的那些风险。由于无钢板刺激,术后长期吞咽困难也可避免。本研究中仅1例自愈患者有不适症状,考虑可能与术中气管插管及食管牵拉水肿有关。此外,我们同时发现,该类融合器可以对存在跳跃节段的病例进行分别固定,而无需采用以往长钢板跨越正常节段的固定方式,保留了正常椎间关节的运动。
Yan等[13]的对照研究认为,采用零切迹自锁装置的手术方式具有与传统的钢板内固定手术的相似临床疗效,且并发症更少。而类似的研究[14]也表明,高分子材质的自锁式融合器在维持颈椎曲度及椎间隙高度的作用与钢板相当。尽管所涉及的病例主要以单节段或2节段为主,但已显示出自锁式零切迹椎间融合器的临床优势。本组病例术后神经功能得到改善,随访期间JOA评分依然保持着相似的水平,Odom评价也提示患者对此手术有较高的满意度。X线随访结果提示末次颈椎测量指标较术后6个月前稍差,但差异无统计学意义,考虑可能与颈椎病患者本身生活习惯未完全改变、病程进展以及内固定导致的全部近节段退变加速有关。三维CT检查提示,所有病例在1年时均获得确切融合,愈合时间较文献[15-16]报道的略长,考虑与病例融合节段较多、融合环境更加严苛有关。结合X线结果,依然可以认为该类融合器提供了良好的物理支撑和适宜的力学环境。我们也相信,对神经的彻底减压与否才是决定患者中长期临床疗效的关键,尽管融合时间相对滞后,但仍存在一定的内固定失效的风险,但针对多节段的病例,其临床疗效仍是值得肯定的。
本研究系回顾性研究,尚缺乏对照性研究的支持;同时也无法明确颈椎曲度及椎间隙高度改善情况是否会随时间的延长而进一步恶化,这需要进一步随访来明确。我们强调,确诊病例选择十分重要,这是能否完成减压的大前提,只有多节段的退变性颈椎病的适然患者,才能使自锁式零切迹椎间融合器操作更加简便,才能在恢复颈椎生理曲度及椎间隙高度上显示优点,也可避免传统钢板内固定所带来的近远期并发症。
参考文献
[ 1 ]Papadopoulos EC,Huang RC,Girardi FP,et al.Three-level anterior cervical discectomy and fusion with plate fixation:radiographic and clinical results[J].Spine(Phila Pa 1976),2006,31(8):897-902.
[ 2 ]Wang JC,McDonough PW,Endow KK,et al.Increased fusion rates with cervical plating for two-level anterior cervical discectomy and fusion[J].Spine(Phila Pa 1976), 2000,25(1):41-45.
[ 3 ]Sasso RC,Ruggiero RA Jr,ReillyTM,et al.Early reconstruction failures after multilevel cervical corpectomy[J].Spine (Phila Pa 1976),2003,28(2):140-142.
[ 4 ]Bazaz R,Lee MJ,Yoo JU.Incidence of dysphagia after anterior cervical spine surgery:a prospective study[J].Spine (Phila Pa 1976),2002,27(22):2453-2458.
[ 5 ]Scheer JK,Tang JA,Smith JS,et al.Cervical spine alignment,sagittal deformity,and clinical implications:a review[J].J Neurosurg Spine,2013,19(2):141-159.
[ 6 ]Singh K,Smucker JD,Gill S,et al.Use of recombinant human bone morphogenetic protein-2 as an adjunct in posterolateral lumbar spine fusion:a prospective CT-scan analysis at one and two years[J].J Spinal Disord Tech,2006,19(6):416-423.
[ 7 ]Demircan MN,Kutlay AM,Colak A,et al.Multilevel cervical fusion without plates,screws or autogenous iliac crest bone graft[J].J Clin Neurosci,2007,14(8):723-728.
[ 8 ]Shimamoto N,Cunningham BW,Dmitriev AE,et al.Biomechanical evaluation of stand-alone interbody fusion cages in the cervical spine[J].Spine(Phila Pa 1976),2001,26(19): E432-E436.
[ 9 ]Bolesta MJ,Rechtine GR 2nd,Chrin AM.Three- and four-level anterior cervical discectomy and fusion with plate fixation:a prospective study[J].Spine(Phila Pa 1976),2000,25(16): 2040-2044.
[10]Wang JC,McDonough PW,Kanim LE,et al.Increased fusion rates with cervical plating for three-level anterior cervical discectomy and fusion[J].Spine(Phila Pa 1976),2001,26(6): 643-646.
[11]Zaveri GR,Ford M.Cervical spondylosis:the role of anterior instrumentation after decompression and fusion[J].J Spinal Disord,2001,14(1):10-16.
[12]Scholz M,Reyes PM,Schleicher P,et al.A new stand-alone cervical anterior interbody fusion device:biomechanical comparison with established anterior cervical fixation devices[J].Spine(Phila Pa 1976),2009,34(2):156-160.
[13]Yan B,Nie L.Clinical comparison of Zero-profile interbody fusion device and anterior cervical plate interbody fusion in treating cervical spondylosis[J].Int J Clin Exp Med,2015,8(8):13854-13858.
[14]Mobbs RJ,Rao P,Chandran NK.Anterior cervical discectomy and fusion:analysis of surgical outcome with and without plating[J].J Clin Neurosci,2007,14(7):639-642.
[15]Dai LY,Jia LS.Single-level instrumented posterolateral fusion of lumbar spine with beta-tricalcium phosphate versus autograft:a prospective,randomized study with 3-year follow-up[J].Spine(Phila Pa 1976),2008,33(12):1299-1304.
[16]Vanek P,Bradac O,Delacy P,et al.Anterior interbody fusion of the cervical spine with Zero-P spacer:prospective comparative study-clinical and radiological results at a minimum 2 years after surgery[J].Spine(Phila Pa 1976),2013,38(13):E792-E797.
中图分类号R681.5+5
文献标志码A
通讯作者张键,E-mail: zhang.jian@zs-hospital.sh.cn
