产后妇女盆底肌力与分娩方式、季节的关系
2016-01-12刘浏,张妤,卫兵等
产后妇女盆底肌力与分娩方式、季节的关系
刘浏,张妤,卫兵,王文艳
(安徽医科大学第二附属医院,合肥230601)
摘要:目的了解产后妇女盆底肌力与分娩方式、季节的关系。方法选择2013年12月~2014年11月安徽医科大学第二附属医院收治的足月妊娠分娩、产后6周复查产妇902例作为研究对象,其中剖宫产410例(剖宫产组)、经阴分娩492例(顺产组)。所有产妇在产后接受盆底肌力检查(受检时间为产后35~118 d,于春、夏、秋、冬季接受盆底肌力检查者分别为191、231、233、247例),采用Glazer评估法评估其盆底肌表面肌电压。结果盆底肌肉的5次快速收缩最大肌电压(Dmax)剖宫产组为(37.01±15.65)μV、顺产组为(31.98±12.56)μV,两组相比,t=-5.359,P<0.01。盆底肌持续收缩60 s的平均肌电压(H60 s)剖宫产组为(21.74±10.71)μV、顺产组为(19.06±8.87)μV,两组相比,t=-4.119,P<0.01。春、夏、秋、冬季接受盆底肌力检查者的Dmax分别为(35.99±11.10)、(34.10±13.00)、(33.45±16.86)、(33.86±14.85)μV,组间相比,F=1.256, P>0.05。春、夏、秋、冬季接受盆底肌力检查者的H60 s分别为(24.87±8.82)、(20.74±8.83)、(17.89±10.33)、(18.55±9.77)μV,组间相比,F=22.721,P<0.01;春、夏季接受检查者的H60 s均明显高于秋季检查者(t分别为7.386、3.193,P均<0.01)。分别以Dmax、H60 s为应变量,以孕次、分娩方式、受检季节为自变量,建立多元线性回归模型,分析显示,分娩方式与Dmax、H60 s有关(P均<0.01),受检季节与H60 s有关(P<0.01)。结论 产后妇女盆底肌肌力与分娩方式有关,剖宫产产妇的盆底肌力较顺产者高;产后妇女盆底肌持续收缩力与受检季节有关,春、夏季比较高。
关键词:盆底肌;盆底功能障碍性疾病;盆底肌表面肌电信号;产妇;分娩方式
doi:10.3969/j.issn.1002-266X.2015.43.004
中图分类号:R714.14文献标志码:A
基金项目:国家自然科学基金资助项目(81100412);安徽医科大学2011年校科研基金资助项目(2011xkj060)。
作者简介:第一刘浏(1985-),女,硕士,医师,主要研究方向为妇女保健。E-mail: liuliuflawless@qq.com
作者简介:通信张妤(1963-),女,学士,主任医师,主要研究方向为围产医学。E-mail: zhangyu8648@163.com
收稿日期:(2015-04-24)
Relationship of postnatal pelvic floor muscle strength with delivery mode and delivery season
LIULiu,ZHANGYu,WEIBing,WANGWen-yan
(TheSecondAffiliatedHospitalofAnhuiMedicalUniversity,Hefei230601,China)
Abstract:ObjectiveTo investigate the relationship between delivery mode, delivery season and postnatal pelvic floor muscle strength. Methods A total of 902 postpartum women, including 410 cases of cesarean delivery (cesarean delivery group) and 492 cases of spontaneous delivery (spontaneous delivery group), were screened for pelvic floor muscle strength after childbirth. The pelvic floor muscle strength of all eligible pregnant women was measured, and the measure time was from 35 to 118 days postpartum. There were 191 cases of pregnant women in the spring, 231 in the summer, 233 in the autumn and 247 in the winter. Glazer protocol was used to measure surface muscle voltage of pelvic floor muscle. Results The maximum muscle voltage of pelvic floor muscle in 5 times of fast-contracting (Dmax) was (37.01±15.65) μV in the cesarean delivery group, and (31.98±12.56) μV in the spontaneous delivery group, and there was significant difference between these two groups(P<0.01). The mean value of 60 s continuous contraction of pelvic floor muscles (H60 s) was (21.74±10.71) μV in the cesarean delivery group, and (19.06±8.87) μV in the spontaneous delivery group, and there was significant difference between these two groups(P<0.01). The mean value of Dmax was(35.99±11.10)μV among pregnant women in the spring,(34.10±13.00) μV in the summer, (33.45±16.86)μV in the autumn, and (33.86±14.85)μV in the winter, and there was no significant difference among these groups (F=1.256, P>0.05). The mean value of H60 s was (24.87±8.82) μV among pregnant women in the spring, (20.74±8.83)μV in the summer, (17.89±10.33)μV in the autumn and (18.55±9.77)μV in the winter, and there was significant difference among these groups (F=22.721, P<0.01).The mean value of H60 s of the women in the spring and summer was significant higher than that in the autumn(t=7.386, 3.193; all P<0.01). If we took Dmax, H60 s, gravidity, delivery mode and the delivery seasons as the independent variable to make the multiple liner regression models, it showed that the delivery mode was related with Dmax and H60 s(P<0.01), and the delivery season was related with H60 s(P<0.01). ConclusionsThe postnatal pelvic floor muscle strength is statistically related with delivery mode, and the postnatal pelvic floor muscle strength is higher in women with cesarean delivery than that with spontaneous delivery. The continuous contraction of pelvic floor muscles is related with the delivery season, which is high in the spring and summer.
Key words: pelvic floor muscle; pelvic floor dysfunction; surface electromyography of pelvic floor muscle; postpartum women; delivery mode
妊娠和分娩是导致女性盆底功能障碍性疾病(PFD)发病的重要独立危险因素。目前,国内外多通过促进盆底肌功能的康复而达到预防PFD的目的。动物实验[1~4]发现,蟾蜍、牛蛙腓肠肌的收缩力随温度的升高而增强,在25 ℃时肌肉收缩力最强,25 ℃后随温度的持续升高,肌肉收缩力出现迅速下降趋势。推测人体肌力可能也会受到温度或者气温的影响,但至今国内外尚未见相关研究报道。本研究对产后妇女盆底肌肌力与分娩方式、季节的相关性进行了分析探讨。现将结果报告如下。
1资料与方法
1.1临床资料选择2013年12月~2014年11月在安徽医科大学第二附属医院分娩、产后6周复查产妇902例作为研究对象,入选标准:恶露干净;无泌尿系统急性炎症;无糖尿病史;无盆腔器官脱垂和尿失禁史;认知能力正常。902例产妇的年龄为(28.35±3.28)岁,产时孕周为(38.83±12.99)周,孕1~9次,产1~3次,新生儿体质量(3.33±0.51)kg。其中剖宫产410例(剖宫产组),经阴分娩492例(顺产组)。所有产妇在产后接受盆底肌力检查,受检时间为产后35~118 d,于春、夏、秋、冬季接受盆底肌力检查者分别为191、231、233、247例。
1.2盆底肌力检测采用MyTrac Pro生物刺激反馈仪进行盆底肌电图检查,用Glazer评估法,在7 min 46 s的时间内让盆底肌群进行指定的收缩和放松动作,检测盆底肌肉Ⅰ类和Ⅱ类肌纤维肌力。通过测量盆底肌群在进行一系列收缩和放松动作时盆底肌的肌电信号,对盆底肌肉的5次快速收缩最大肌电压(Dmax)和盆底肌持续收缩60 s的平均肌电压(H60 s)等指标进行记录。
1.3统计学方法采用SPSS17.0统计软件。两组均数的比较用独立样本t检验,多组均数的比较用方差分析,两样本相关性分析用Spearman等级相关分析法;分别以Dmax、H60 s为应变量,以孕次、分娩方式、受检季节为自变量,建立多元线性回归模型(对季节进行亚变量设置,以秋季为参照)。P<0.05为差异有统计学意义。
2结果
902例产妇的盆底肌肉Dmax为(34.27±14.26)μV,H60 s为(20.28±9.83)μV。
盆底肌Dmax剖宫产组为(37.01±15.65)μV、顺产组为(31.98±12.56)μV,两组相比,t=-5.359,P<0.01。盆底肌H60 s剖宫产组为(21.74±10.71)μV、顺产组为(19.06±8.87)μV,两组相比,t=-4.119,P<0.01。
春、夏、秋、冬季受检产妇盆底肌Dmax和H60 s的变化趋势见图1。图1显示,无论是顺产还是剖宫产分娩的产妇,其盆底肌Dmax都随着季节呈现一条与横轴平行的曲线,即Dmax不会随着季节的变化而发生改变;然而,顺产和剖宫产分娩的产妇,其盆底肌H60 s随着季节呈现波动,从1月开始上升,到3、4月达“峰值”,之后开始下降,8、 9月达“谷值”,之后又出现上升趋势。春、夏、秋、冬季接受盆底肌力检查者的Dmax分别为(35.99±11.10)、(34.10±13.00)、(33.45±16.86)、(33.86±14.85)μV,组间相比,F=1.256,P>0.05。春、夏、秋、冬季接受盆底肌力检查者的H60 s分别为(24.87±8.82)、(20.74±8.83)、(17.89±10.33)、(18.55±9.77)μV,组间相比,F=22.721,P<0.01;春、夏季接受检查者的H60 s均明显高于秋季检查者(t分别为7.386、3.193,P均<0.01)。
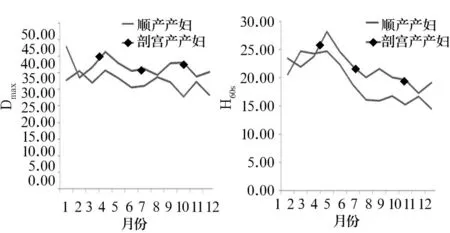
图1 春、夏、秋、冬季受检产妇盆底肌D max和H 60 s的变化
分别以Dmax、H60 s为应变量,以孕次、分娩方式、受检季节为自变量,建立多元线性回归模型,分析结果见表1。表1显示,分娩方式与Dmax、H60 s有关,受检季节与H60 s有关。
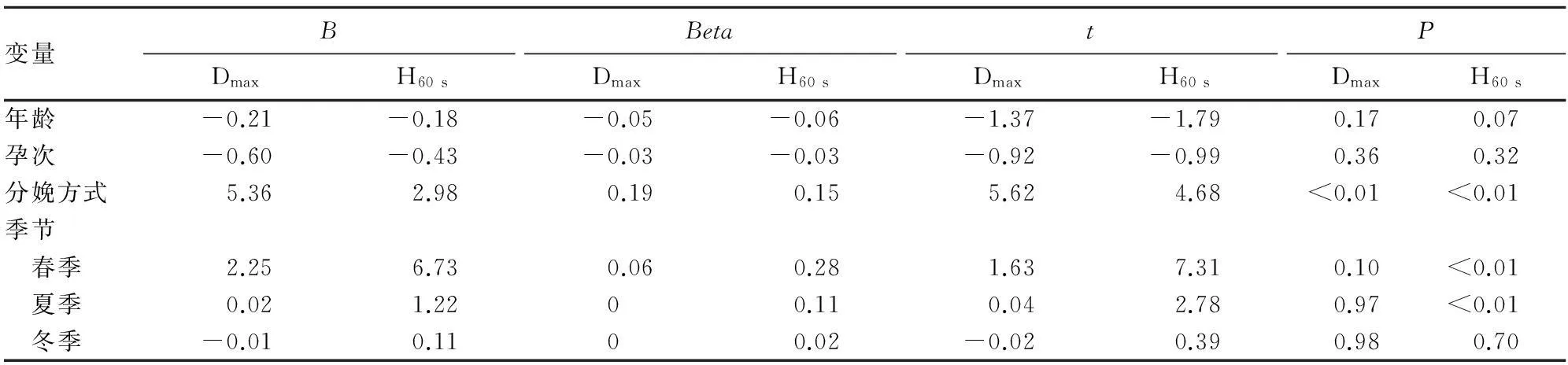
表1 分底肌D max、H 60 s的相关因素分析结果
注:B为回归系数,Beta为标注化回归系数;在季节的亚变量设置中,以秋季为参照。
3 讨论
盆底肌肉训练对预防产妇PFD的作用是明确的[5,6]。因此,了解会阴、阴道和肛门括约肌的张力,及时发现并帮助早期盆底肌力减退的产后妇女开展康复训练,有助于对PFD的预防[7]。
PFD发生的可能机制是盆底支撑系统与腹腔压力的失衡。盆底肌是PFD发生的第一道防线,盆底结缔组织是PFD发生的第二道防线。妊娠和分娩会造成盆底肌的损伤,承托盆腔器官的任务落到第二道防线上,使得盆底结缔组织发生变形、伸长,PFD随之出现[8,9]。本研究结果显示,顺产组的Dmax和H60 s明显低于剖宫产组,与文献[10]结果一致。可能原因是产妇在经阴分娩过程中,软产道和周围的盆底组织极度扩张,特别是胎儿头围偏大、第二产程延长、急产、阴道助娩产者,盆底肌纤维、神经、韧带、筋膜都受到不同程度的损伤[11,12]。阴道分娩是女性PFD发生的一个重要独立危险因素[13,14],韩采青等[15]发现,经阴道分娩容易导致产后盆底功能受损。
动物实验[1~4]发现,蟾蜍、牛蛙腓肠肌的收缩力随温度的升高而增强,在25 ℃时肌肉收缩力最强,25 ℃后随温度的持续升高,肌肉收缩力迅速下降。本研究发现,产后妇女盆底肌H60 s与受检季节存在相关性,春、夏季受检者的盆底肌H60 s明显高于秋季受检者,3、4月受检者的盆底肌H60 s最高,之后开始下降,8、9月受检者的盆底肌H60 s最低,之后又出现增高趋势,并且这种关系不受分娩方式的影响。据此可以推测,H60 s随着季节变化而出现周期性波动,即盆底肌的持续收缩肌力可能会因气温或其他气候因素的影响而发生变化。本研究结果提示,产褥期妇女机体的内、外环境保持在15~25 ℃可能更有利于盆底肌收缩力的恢复,从而可有效预防产后盆底功能障碍性疾病。
参考文献:
[1] 张声蓉,张东东,郑彩顺,等.不同理化因素对肌肉疲劳影响的探讨[J].医学理论与实践,2014,27(5):561-562.
[2] 赵敬国,李建文. 温度对蟾蜍腓肠肌收缩能力的影响[J].山东科技,2002,24(3):36-37.
[3] 王艳.温度对蛙腓肠肌收缩的影响[J].四川职业技术学院学报,2006,16(4):116-117.
[4] 陈彤,黄仁美.温度对牛蛙腓肠肌收缩性的影响[J].福建畜牧兽医,2008,30(6):7-9.
[5] Boyle RL, Hay-Smith EJ, Cody JD, et al. Pelvic floor muscle training for prevention and treatment of urinary and fecal incontinence in antenatal and postnatal women: a short version cochrane review[J]. Neurourol Urodyn, 2014,33(3):269-276.
[6] Hay-Smith J, Herderschee R, Dumoulin C, et al. Comparisons of approaches to pelvic floor muscle training for urinary incontinence in women: an abridged cochrane systematic review[J]. Eur J Phys Rehabil Med , 2012,48(4):689-705.
[7] Leijonhufvud Å, Lundholm C, Cnattingius S, et al. Risk of surgically managed pelvic floor dysfunction in relation to age at first delivery[J] . Am J Obstet Gynecol, 2012,207(4):303-309.
[8] Dua A, Radley S, Jones G, et al. The personal impact of pelvic floor symptoms and their relationship to age[J] . Int Urogynecol J, 2014,25(1) :117-121.
[9] Andrada-Hamer M, Persson J. Familial predisposition to pelvic floor dysfunction: prolapse and incontinence surgery among family members and its relationship with age or parity in a swedish population[J] . Eur J Obstet Gynecol Reprod Biol, 2013,170(2):559-562.
[10] Leijonhufvud A, Lundholm C, Cnattingius S, et al. Risk of surgically managed pelvic floor dysfunction in relation to age at first delivery[J] . Am J Obstet Gynecol, 2012,207(4):303-309.
[11] 单淑芝,石彬.盆底功能障碍性疾病及相关生物力学研究进展[J].中国实用妇科与产科杂志,2010,26(4):304-306.
[12] 张珂,王澜静,焦玲洁,等.产后盆底功能障碍性疾病与盆底肌收缩力及其相关因素分析[J].实用妇产科杂志,2014,30(10):757-759.
[13] Hyland G, Hay-Smith J, Treharne G. Women′s experiences of doing long-term pelvic floor muscle exercises for the treatment of pelvic organ prolapse symptoms [J]. Int Urogynecol J, 2014,25(2):265-271.
[14] Boyle R, Hay-Smith EJ, Cody JD, et al. Pelvic floor muscle training for prevention and treatment of urinary and fecal incontinence in antenatal and postnatal women: a short version Cochrane review[J] .Neurourol Urodyn, 2014,33(3):269-276.
[15] 韩采青,领雪峰.盆底功能训练联合生物反馈电刺激在经阴分娩产妇盆底功能改善中的作用[J].山东医药,2014,54(23):63- 65.
