Risk factors of polycystic ovarian syndrome among Li People
2015-12-23BaoShanJunhongCaiShuYingYangZhuoRiLi
Bao Shan, Jun-hong Cai, Shu-Ying Yang, Zhuo-Ri Li
1Department of Gynecology and Obstetrics, Hainan Provincial People’ s Hospital, Haikou 570311, China
2Central Laboratory, Hainan Provincial People’ s Hospital, Haikou 570311, China
3Department of Surgery, Hainan Provincial People’ s Hospital, Haikou 570311, China
Risk factors of polycystic ovarian syndrome among Li People
Bao Shan1, Jun-hong Cai2, Shu-Ying Yang1, Zhuo-Ri Li3*
1Department of Gynecology and Obstetrics, Hainan Provincial People’ s Hospital, Haikou 570311, China
2Central Laboratory, Hainan Provincial People’ s Hospital, Haikou 570311, China
3Department of Surgery, Hainan Provincial People’ s Hospital, Haikou 570311, China
ARTICLE INFO
Article history:
Received 15 April 2015
Received in revised form 20 May 2015
Accepted 15 June 2015
Available online 20 July 2015
Li people
Objective: To study the relevant risk factors of polycystic ovarian syndrome (PCOS) of Li People so as to provide basis for early diagnosis and treatment of PCOS. Methods: With casecontrol study method, 285 cases of PCOS of Li People were as recruited case group, and 580 cases of non-PCOS of female Li People as control group. Questionnaire was adopted to collect data regarding risk factors of PCOS, then the risk factors of PCOS was searched by univariate and multivariate analysis. Results: Multivariate analysis showed that the risk factors of PCOS included in menstrual cycle disorder (OR=5.824), bad mood (OR=2.852), family history of diabetes (OR=7.008), family history of infertility (OR=11.953), menstrual irregularity of mother (OR=2.557) and lack of physical exercise (OR=1.866). Conclusions: To target the high risk factors of menstrual cycle disorder, family history of diabetes, family history of infertility, family history of diabetes, bad mood and lack of physical exercise of female population, we should implement early screen, diagnose and treatment of POCS in order to reduce the incidence rate of PCOS and improve prognosis of PCOS.
1. Introduction
Polycystic ovarian syndrome (PCOS), featuring problematic follicular development, is an endocrine system disorder that has lifelong impact upon its patients. Prevalence of PCOS among women at reproductive age was reported to be 5%-10%[1]. The disease is characterized by oligomenorrhea or amenorrhea, unovulation, insulin resistance (IR), hyperandrogenemia and cysts on the ovaries[2] and deemed as one of the main cause of anovulatory infertility. It does a lot of harm to women’s physical and mental health. Etiology of PCOS is still unknown and prevalence of this disease varies due to the differences in genetic traits and living environment of its victims. The Hainan province is a tropical island on which multiple ethnic groups including Han people and Li people live. Territorial clustering of habitation provides favorable condition for research of the prevalence and risk factor of PCOS among the Li ethnic minority population in Hainan, China. With case-control study design, this study investigate the risk factors of PCOS among female Li people at reproductive age living in the Hainan province to inform decision making regarding early screen and preventive measures against PCOS.
2. Materials and methods
2.1. Sample of the study
Of 285 cases were recruited from hospitalized patients from January 2014 to December 2014 in four of the cities or counties of the Hainan province, namely Lingshui, Qiongzhong, Changjiang, and Sanya, where Li population is concentrated. All cases met the diagnosis criteria of PCOS published by the Chinese Ministryof Health, which defines a PCOS patient as one who must have symptoms of oligomenorrhea and amenorrhea or abnormal uterine bleeding as well as one of the two following symptoms: hyperandrogenism and polycystic ovaries. Other cause of hyperandrogenism and polycystic ovaries must be excluded to make the diagnosis. Patients with malignant tumor, cardiovascular disease, server organic disease, and psychiatric issues were excluded from the sample. Of 580 cases of non-PCOS of female Li People were sampled from those hospitals during the same time period. Hospital ethic committees approved the study and all subjects had signed the informed consent form.
2.2. Data collection
Self-designed questionnaire was handed out among case and control groups. Data collected include patients’ age, address, BMI, age of menarche, length of period cycle, gravida, parity, marital status, education, vocation, menstrual disorder, alcohol intake, tea drinking, mood, family relationship, family history of PCOS, family history of diabetes, family history of infertility, mother’s irregular menstruation and lack of physical exercise. Data of other PCOS-related conditions including hirsutism, acne, skin conditions and ultrasound findings of ovarian were also obtained. Biochemistry tests for testosterone (Testo), luteotropic hormone (LH), Folliclestimulating hormone (FSH), Insulin (INS), glucose (GLU) and so on were carried out using automatic biochemistry analyzers and chemiluminescence analyzers.
2.3. Statistical analysis
Epidata 3.02 was employed for double data entry in order to ensure the quality of data record. All the data were analyzed by statistical software of SPSS 18.0. Chi-square test and t test were used to respectively analyze measurement data and enumeration data. Multivariate Logistic Regression was performed to adjust for impacts of multiple factors, and using of stepwise method to screen model. P<0.05 is defined as statistically significant in this study.
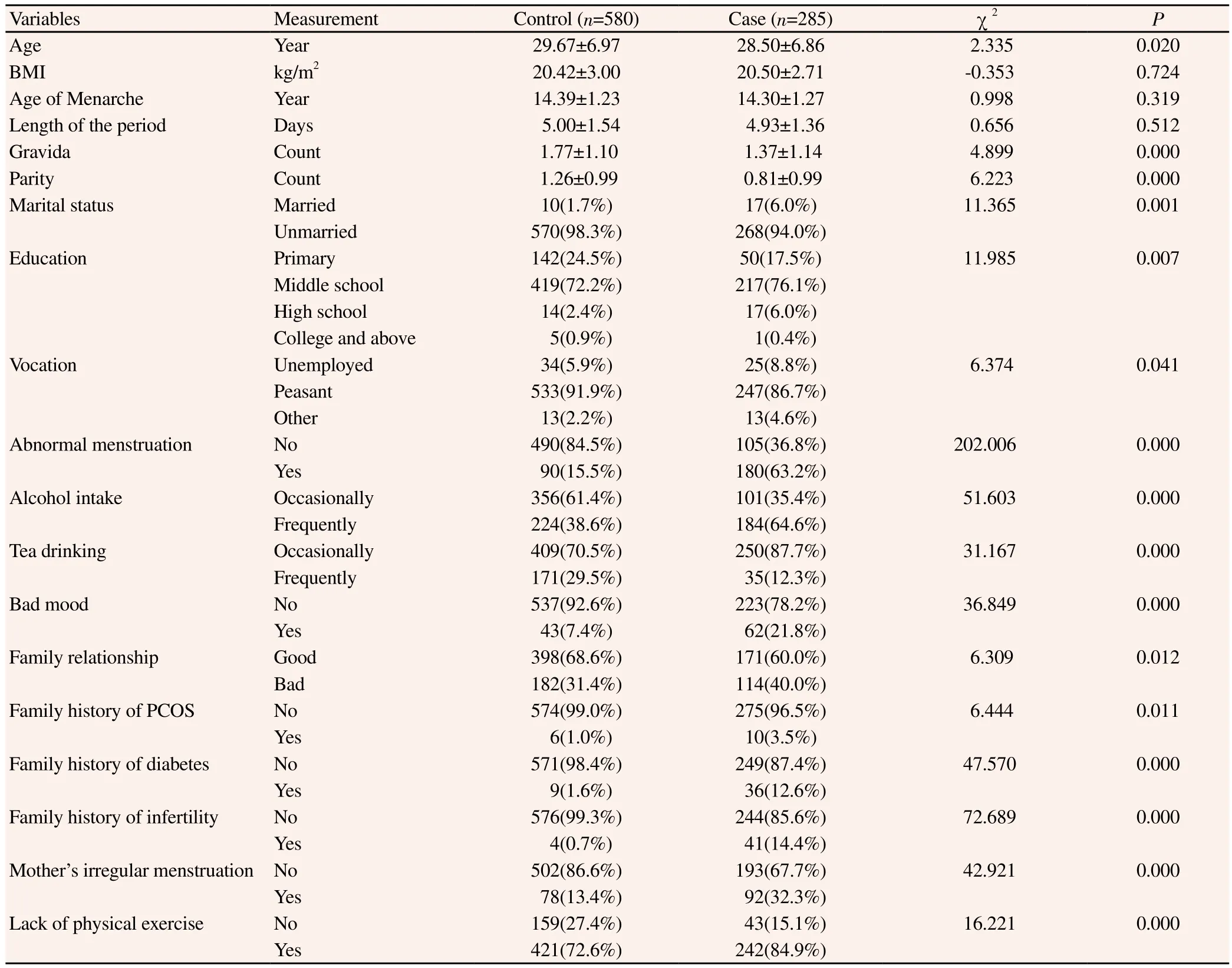
Table 1 Chi-square analysis of risk factors for PCOS.

Table 2 Multivariate analysis of risk factors for PCOS.
3. Results
3.1. Univariate analysis of risk factors for PCOS
Results of chi-square analysis was shown in table 1 and it can be interpreted that age, gravida, parity, marital status, education, vocation, irregular menstruation, alcohol, tea drinking, bad mood, family relationship, family history of PCOS, family history of diabetes, family history of infertility and mother’s irregular menstruation were all significantly related to the incidence of PCOS.
3.2. Multivariate analysis on risk factors for PCOS
With incidence of PCOS as the dependent variable (ycontrol=0, ycase=1) and the 16 variables selected by the univariate analysis as independent variables, multivariate logistic regression were performed using step-wise method to confirm the risk factors for PCOS. Study results reported in table revealed that irregular menstruation, bad mood, family history of infertility and diabetes, mother’s irregular menstruation, unpleasant mood, and lack of physical exercise were statistically associated with PCOS.
4. Discussion
Etiology of PCOS is still inconclusive due to its complexity. One study attributes its cause to the interaction between genetic and environment factors[3]. Due to the fact that PCOS patients share one significant clinical manifestation of hyperandrogenemia, male hormone has been widely acknowledged as a biomarker for PCOS in recent years. Except for hyperandrogenemia, PCOS also involve obesity, insulin resistance and type 2 diabete and all of these complications lead to the ovarian production of androgen. Some studies also suggested that adolescent obesity increases the probability of PCOS at a later stage of life and insulin resistance as well as ensuing hyperinsulinemia may directly or indirectly result in LH secretion that leads to hyperandrogenemia[4,5]. As it has been confirmed obesity is the main risk factor for type 2 diabetes, there is a hypothesis that obesity, insulin resistance as well as hyperandrogenism were all potential risk factors for PCOS. For generations the Li people have been living in the Hainan province and exogamy remains much less prevalent among them. Their genetic polymorphism has great implications for research of causes of PCOS. This study of the 1 099 female of Li Chinese found that PCOS prevalence among Li people is as high as 8.2%, much higher than the incidence rate (5.6%) of Chinese women of childbearing age in 2013 reported by Li et al[6], higher than Greek women (6.8%) [7] and Spanish white women (6.5%)[8]. Ethnic differences play an important part in metabolism of PCOS, including in insulin resistance, glucose intolerance, dyslipidemia and so on. With regard to the high incidence rate of PCOS of Li People in Hainan Province, it might be concerned with lifestyle affecting metabolic factors.
Results of the study indicates that the risk factors for PCOS including irregular menstruation, family history of infertility and diabetes, mother’s irregular menstruation, unpleasant mood, and lack of physical exercise. Most PCOS patients experience the onset of irregular menstruation since adolescence and Endocrine dyscrasia along any part of the hypothalamic-pituitary-gonadal axis may lead to irregular menstruation and anovulation[9]. It is also confirmed by our study that PCOS is closely related to irregular menstruation. IR as an important contributor to PCOS was found in some of our participants and some studies reported that percentage of IR among PCOS patients was as high as 50% to 70%[10]. Family history of diabetes, notably a inherited metabolic disorders, also poses significantly high risk for PCOS. This is consistent with the finding of Roe et al[11]. Tian et al[12] reported the odds ration of mother’s infertility OR was 8.599 while our study found that it was 11.953, which suggested the heredity of the PCOS disease. The correlation between mother’s irregular menstruation and the daughter’s also contribute to higher risk of PCOS of the daughter. Our study suggested that mother’s irregular menstruation can be translated into a 2.557 odds ratio of daughter’s PCOS, which is similar to the findings of Bates et al[13]. Both national and abroad psychology evaluation studies discovered severe mental or psychological disorder among PCOS patients, and it is inferred that unpleasant mood also increase the risk for PCOS. Research of Xiao et al described similar findings in this aspect[14]. Lack of physical exercise, leading to uneven distribution of body fat,is an important risk factor of centripetal obesity. One study advises proper diet and regular physical exercise to obese PCOS patients to achieve significant alleviation of symptoms like excessive hair and irregular menstruation and if combining medicine with kinesitherapy and Individualized nutrition therapy within three months patients can also expect significant improvement in metabolism and internal secretion[15].
Contrast with Han People, Li People women likes to eat pickled food, coarse food, drink and salty food, with irregular diet. Most of Li People use of rice straw and leaf as fuel, and it lead to air pollution. Moreover, Li People are a little idleness, lack of physical activity. These lifestyles play different extent to affect insulin resistance and lipid metabolism disorder of Li People women, and human metabolic disorders also would induce to the incidence of PCOS. This study result showed that the factors of metabolic diseases included in diabetes history and lack of physical exercise, and the other metabolic disease factors were not contained in this study, because of the limitation of epidemiologic survey. In the future study, we should further improve project design.
Conflict of interest statement
We declare that we have no conflict of interest.
[1] Wang YY, Hao SL, Hou LH, Wu XK. Research progress on cardiovascular risk factors for polycystic ovarian syndrome. J Medl Res 2013; 42(7): 11-13.
[2] Liu Y, Li C, Wang LL. Logistic regression of risk factors for polycystic ovarian syndrome with Clomiphene citrate resistance. J Reprod Med 2014; 39(11): 1542-1545.
[3] Society of Gynecology and Obstetrics of the Chinese Medical Association. Expert consensus for diagnosis and treatment of polycystic ovarian syndrome. Chin J Obst Gynecol 2008; 43(7): 553-555.
[4] Zhang JY, He H. Risk factors and treatment for infertility caused by polycystic ovarian syndrome. Hainan Med 2014; 25(12): 1750-1753.
[5] Li FX, Fan GL, Yi JP. Research review on risk factors for cardiovascular disease among polycystic ovarian syndrome patients. Maternal Child Health Care China 2012; 27(32): 5218-5220.
[6] Li R, Zhang Q, Yang D, Li S, Lu S, Wu X, et al. Prevalence of polycystic ovary syndrome in women in China: a large community-based study. Hum Reprod 2013; 28(9): 2562-2569.
[7] Diamanti-Kandarakis E, Kouli CR, Bergiele AT, Filandra FA, Tsianateli TC, Spina GG, et al. A survey of the polycystic ovary syndrome in the Greek island of Lesbos: hormonal and metabolic profile. J Clin Endocrinol Metab 1999; 84(11): 4006-4011.
[8] Asuncion M, Calvo RM, San Millán JL, Sancho J, Avila S, Escobar-Morreale HF. A prospective study of the prevalence of the polycystic ovary syndrome in unselected Caucasian women from Spain. J Clin Endocrinol Metab 2000; 85(7): 2434-2438.
[9] Du JY, Xu ZY, Feng JY. Impact of environment on the incidence of polycystic ovarian syndrome in the Weihai district. Chin J Healthy Birth & Child Care 2012; 18(5): 269-272.
[10] Karakas SE, Kim K, Duleba AJ. Determinants of impaired fasting glucose versus glucose intolerance of polycystic ovary syndrome. Diabetes Care 2010; 33(4): 887-893.
[11] Roe AH, Prochaska E, Smith M, Sammel M, Dokras A. Using the androgen excess-PCOS society criteria to diagnose polycystic ovary syndrome and the risk of metabolic syndrome in adolescents. J Pediatrics 2013; 162(5): 937-941.
[12] Tian XX, Ruan XY, Wang J, Liu SY, Yin DM, Lu YJ, et al. Analysis of risk factors for 437 cases of polycystic ovary syndrome. J Capital Univ Med Sci 2014; 35(4): 414-418.
[13] Bates GW, Legro RS. Longterm management of polycystic ovarian syndrome (PCOS). Mol Cellular Endocrinol 2013; 373(1-2): 91-97.
[14] Xiao WH, Qiu XY, Zhang T, Zhuang AW. Study on the mood of polycystic ovarian syndrome patients. Zhejiang J Trad Chin Med 2011; 46(11): 795-796.
[15] Le Donne M, Alibrandi A, Giarrusso R, Lo Monaco I, Muraca U. Diet, metformin and inositol in overweight and obese women with polycystic ovary syndrome: effects on body composition. Minerva Ginecol 2012; 64(1): 23-29.
*Corresponding author:Zhuo-Ri Li, Department of Surgery,Hainan Provincial People’s Hospital, Haikou 570311, China.
Tel: 86-898-68622476
Fax: 86-898-68622476
E-mail: Baoshan3@hotmail.com
Foundation project: It is supported by Social Development of Hainan Province Special Fund of Science and Technology (SF201302).
Polycystic ovarian syndrome
Risk factors
杂志排行
Asian Pacific Journal of Tropical Medicine的其它文章
- Influence of overexpression of SOCS2 on cells of DN rat
- Effect of salinomycin on metastasis and invasion of bladder cancer cell line T24
- Expression of transferrin in hematoma brain tissue at different stages after intra cerebral hemorrhage in rats
- Effect of subarachnoid nerve block anesthesia on glutamate transporter GLAST and GLT-1 expressions in rabbits
- Relationship between gene polymorphisms and prostate cancer risk
- Anti-tumor effect of LTA combined with 5-FU on H22 tumor bearing mice
