Effect of low-intensity pulsed ultrasound on posterolateral lumbar fusion of rabbit
2015-12-08JianWangJianWeiLiLeiChen3rdDepartmentofOrthopedicsRizhaoPeopleHospitalAffiliatedtoShandongUniversityRizhao276826China
Jian Wang, Jian-Wei Li, Lei Chen3rd Department of Orthopedics, Rizhao People’s Hospital Affiliated to Shandong University, Rizhao 276826, China
Effect of low-intensity pulsed ultrasound on posterolateral lumbar fusion of rabbit
Jian Wang, Jian-Wei Li, Lei Chen*
3rd Department of Orthopedics, Rizhao People’s Hospital Affiliated to Shandong University, Rizhao 276826, China
ARTICLE INFO
Article history:
Received 26 October 2014
Received in revised form 10 November 2014
Accepted 22 December 2014
Available online 20 January 2015
Low-intensity pulsed ultrasound
Lumbar posterolateral
Fusion
Ilium
Objective: To observe the effect of low-intensity pulsed ultrasound in the posterolateral lumbar fusion of rabbit. Methods: A total of 48 New Zealand white rabbits were randomly divided into the observation group and control group, including the autogenous iliac observation group, artificial bone observation group, artificial bone control group and autogenous iliac control group according to the different bone grafting. The posterolateral lumbar fusion of rabbits in each group was analyzed and compared. Results: After 4 weeks of treatment using the low-intensity pulsed ultrasound, the fusion in the bone grafting area of observation group was good. There was the relatively dense fusion area between the right transverse process and artificial bone. The left transverse process had been completely fused, with the clear bone trabecula through the fusion area. There was no significant fusion sign in the control group. According to the fusion comparison between two groups, the fusion rate of the observation group was 83.3% and it was significantly higher than the one of the control group (37.5%). Results of the comparison were statistically significant (P<0.05). The number of chondrocytes and the increase in the relative gray-scale in the fusion area of the iliac observation group were significantly higher than ones of the iliac control group (P<0.05). The number of chondrocytes and the increase in the relative gray-scale in the fusion area of the artificial bone observation group were significantly higher than ones of the artificial bone control group (P<0.05). The expression of IL-1, IL-6 and IL-17 4 weeks after the treatment of the observation group was significantly lower than the one of the control group, with the statistical significance (P<0.05). It indicated that the treatment of low-intensity pulsed ultrasound could reduce the expression level of inflammatory factors. Conclusions: The low-intensity pulsed ultrasound can significantly increase the bone grafting fusion rate of the rabbit’s posterolateral lumbar fusion. The possible mechanism is that it promotes the lumbar posterolateral endochondral ossification and reduces the inflammatory reaction.
1. Introduction
The bone grafting fusion is one of common surgical procedures in the treatment of spinal diseases[1]. Generally speaking, the spinal fusion can be divided into the posterolateral fusion, posterior interbody fusion and anterior interbody fusion[2]. The former one is always adopted in the lumbar spinal surgery. As the spinal surgery mainly destroys the stability of joints, the reconstruction of spinal stability is of critical importance for the post-operative recovery of spinal function[3]. The rigid internal fixation and spinal fusion complement each other, showing the close relationship with the success of lumbar spinal surgery[4]. It is a thorny problem how to promote the favorable fusion of bone grafting area in the field of spinal treatment. This study adopted the model of the rabbit’s lumbar posterolateral fusion to observe the effect of low-intensity pulsed ultrasound (LIPUS) on the autogenous bone grafting fusion. It thus discussed the effect of LIPUS on the rabbit’s posterolateral lumbar fusion. Results are shown as follows.
2. Materials and methods
2.1. Subjects
48 New Zealand white rabbits were chosen in this study, with the weight of 2.0-2.8 kg individually and without any limitation on the gender.
2.2. Artificial bone and ultrasonic instrument
The hydroxyapatite artificial bone was in the shape of long strip with 1 g per piece, where, compressive strength ≥125 Mpa, the porosity of (50±20)%, the pore size of 200-500 μm and the gap connection rate >95%. The low-intensity pulsed ultrasonic instrument was purchased from Smith Nephew. The ultrasound in the treatment parameters was sinusoidal pulse wave, with the frequency of 1.5 MHz, intensity of 30 Mw/cm2, pulse width of 200 μs and repetition frequency of 1 KHz.
2.3. Establishment of animal model
Skin was prepared for experimental rabbits 3-5 days before the operation. Rats were pre-operative weighted and had intravenous anesthesia of 3% sodium pentobarbital at the edge of ear. After the success of anesthesia, the prone position operation was adopted. All rats were sterilized and draped. 3cm straight incision was done at the side of erector spine in the right. Skin was cut and was wrapped by fascia layer by layer. In the intermuscular space outside the erector spine the transverse tips of L5 and L6 was exposed. Blunt dissection was carried out to expose the transverse process of L5 and L6 and the intertransverse gap. The transverse periosteum was removed. The wound was washed with the hydrogen peroxide solution and the stripped artificial bone was implanted. It was stitched layer by layer after the operation and the incision was closed. The same procedure was used to expose the transverse process of L5 and L6 in the left. It was continued along the lower and posterior direction to expose the ilium. Blunt dissection was carried out to remove the muscle attached to the ilium. The ilium pieces were chose with the size of 2 cm×1 cm to be implant in the intertransverse gap of L5 and L6. The incision was closed layer by layer. The povidone iodine was adopted to disinfect the incision after the operation, with the intragluteal injection of benzylpenicillin sodium 1.6 million U. Wound was dressed after the operation, and rats had intramuscular injection of benzylpenicillin sodium 80 UI time/day, for 1 week.
2.4. Experimental groups
Experimental animals were randomly divided into the observation group and control group, including autogenous iliac observation group, artificial bone observation group, artificial bone control group and autogenous iliac control group according to the different bone grafting.
2.5. Low-intensity pulsed ultrasound treatment
The ultrasound treatment was carried out in the observation group 1 week after the operation. Wounds of experimental animals had been healed perfectly. The intravenous anesthesia of 1.5 mL and 3% sodium pentobarbital was done at the edge of ear. The ultrasonic probe of therapeutic instrument was put close to the skin of bone grafting fusion area. The ultrasonic couplant was applied between the probe and skin. The special device was used to fix the probe and the treatment was carried out, 20 min/day at each side for 4 weeks. The placebo treatment was carried out using the same therapeutic instrument in the control group.
2.6. Post-operative X-ray detection
The lumbar was taken posterior to anterior X-ray films after the operation and the completion of ultrasonic detection to compare the change in the gray value of X-ray in the fusion area before and after the ultrasonic treatment. Image J was applied to analyze the gray value of X-ray in the fusion area before and after the treatment. Gray value in the fusion area/ scale gray value was equal to the relative gray-scale value. The scale on each X-ray film was the same. The equation was as follows: The gray value in the fusion area after the treatment/scale gray value - gray value in the fusion area before the treatment - scale gray value = increase in the relative gray-scale.
2.7. Specimens collection and histological detection
The euthanasia was adopted to execute animals after the ultrasonic treatment. After the fusion specimens of L5/6 segments was obtained, the procedures of decalcification embedment and section and then HE straining were carried out. The ossification was observed and the chondrocytes was counted under the optical microscope. Six high power fields were counted in each fusion area. The mean equaled to the number of chondrocytes in such fusion area.
2.8. Double antibody sandwich ELISA detection
Blood collection was done on all experimental animals before the operation, 2 weeks and 4 weeks after the operation. The serum was separated and stored in the place with the temperature of -70 ℃. The double antibody sandwich ELISA was used to detect factors of IL-1, IL-6 and IL-17.
2.9. Statistical treatment
Fisher exact probability test was adopted using the four-
fold table data to observe the fusion area on X-ray film. Two-factor two-level factorial analysis was done to analyze the increase in the gray scale of X-ray fusion area and the number of chondrocytes. Where P<0.05 it indicated the statistical difference.
3. Results
3.1. Comparison of X-ray results
48 rabbits were included in this experiment. One case in the observation group died of the incision infection and one case in the control group died of the diarrhea and incision infection during the study. Alternative rabbits were included to replace those dead ones; in this way, there were 24 cases in each group. After 4 weeks of treatment using the lowintensity pulsed ultrasound, the fusion in the bone grafting area of observation group was good. There was the relatively dense fusion area between the right transverse process and artificial bone. The left transverse process had been completely fused, with the clear bone trabecula through the fusion area. There was no significant fusion sign in the control group (Figure 1).
3.2. Histological observation
5 weeks after the operation, it showed a great number of cartilage tissues in the fusion area of treatment group, as well as the relatively mature fixation around the cartilage tissues. There were many primary bone marrow cavities and the structure of bone trabecula under the low power lens. The number of chondrocytes was relatively less in the control group, without any primary bone marrow cavity. Under the high power lens, it showed a great number of chondrocytes in the observation group with the clear structure of bone trabecula. There was only separated chondrocyte island in the fusion area of control group ( Figure 2).
3.3. Fusion comparison
According to results of the fusion comparison between two groups, the fusion rate of the observation group was 83.3% and it was significantly higher than the one of the control group 37.5% (P<0.05) (Table 1).

Table 1 Fusion comparison.
3.4. Increase in relative gray-scale and the mean number of chondrocytes under high power lens between groups before and after the treatment
In this study, the number of chondrocytes and the increase
in the relative gray-scale in the fusion area of the iliac observation group were significantly higher than ones of the iliac control group (P<0.05). The number of chondrocytes and the increase in the relative gray-scale in the fusion area of the artificial bone observation group were significantly higher than ones of the artificial bone control group (P<0.05). There was no statistical difference in the number of chondrocytes and the increase in the relative gray-scale between the artificial bone observation group and the iliac observation group (P>0.05) (Table 2).

Table 2 Increase in relative gray-scale and the mean number of chondrocytes under high power lens between groups before and after the treatment.
3.5. Expression of inflammatory factors IL-1, IL-6 and IL-17 during different stages
2 weeks after the operation of two groups, the expression of IL-1, IL-6 and IL-17 showed the upward tendency. 2 weeks after the operation, the increase in the expression of IL-1, IL-6 and IL-17 in the control group was relatively higher than the one of observation group, but results had no statistical significant difference (P>0.05). 4 weeks after the operation, the expression of IL-1, IL-6 and IL-17 in the observation group was significantly lower than the one of the control group, with the statistical significant difference (P<0.05) (Table 3).
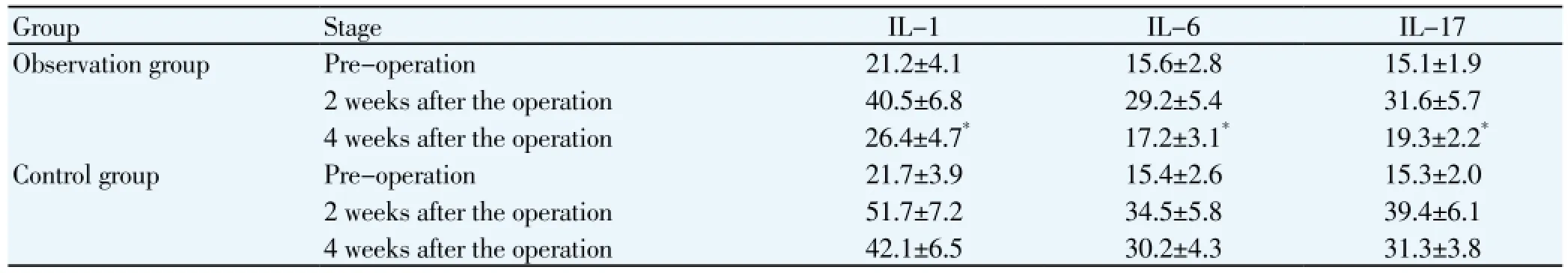
Table 3 Expression of inflammatory factors IL-1, IL-6 and IL-17 during different stages (mean±sd, pg/mL).
4. Discussion
The posterior spinal fusion is the most common procedure for the reconstruction of spinal stability. The improved mechanical stability after the fusion can significantly reduce the instability, degeneration and disorder of spine. The objective of spinal fusion is to maintain the mechanics and physiological curvature, correct the segmental instability, prevent and relieve the nerve pain[5,6]. The failure of spinal fusion is one of the most common complications in the spinal surgery[7]. In the treatment of spinal diseases, no matter the progressive anterior spinal fusion, the lumbar posterolateral fusion is always of importance. Many procedures of the fusion treatment of spinal diseases can be used in the reconstruction of spinal stability[8], such as the anterior and posterior intertransverse, interspinal and posterior interspinal ones. The biomechanical study shows that the mechanical stability provided by the intertransverse fusion and anterior lumbar fusion is significantly better than the one by the posterior interspinal fusion. Meanwhile, the posterolateral fusion is the best procedure to obtain the good segmental stability, with the slight impact on the adjacent segments[9]. As the complications such as the pseudarthrosis caused by the spinal fusion can lead to high rate of fever, as well as serious consequences of progressive scoliosis, pain and joint instability, it is one of basic objectives for the spinal operation to increase the bone grafting fusion rate, in order to obtain the solid and fast fusion[10].
The ultrasound is some kind of mechanical energy that can be transmitted into the human body in the form of high-frequency sound wave. The low-intensity pulsed ultrasound is some kind of sonic pressure wave, which can make use of the effect of mechanical stimulation and also prevent from the damage of heat effect against the tissues and cells. It can assist the tissues in producing the microstructural tension and compression stress, leading to a series of biological effects to promote the generation and maturity of bones finally. Previous studies showed that the application of low-intensity pulsed ultrasound in the treatment of fracture healing, cartilage repairing and knee osteoarthritis all had the good results[11-13]. Korstjens et al[14] found that LIPUS could significant increase the content of 35S-sulfate in the extracellular matrix of cartilage grafts of normal and diseased joints, which could promote the synthesis of articular cartilage matrix. Wang et al[15] applied the LIPUS treatment in the rabbit’s bilateral radial fracture-separation model to promote the fracture healing. Results showed that the observation group receiving LIPUS treatment was significantly better in the anti-bending and anti-torque than the control group. It indicated that LIPUS could effectively promote the fracture healing, shorten the time of fracture healing and enhance the degree of fracture healing along with the increase in the time of ultrasonic treatment. Meanwhile, Hantes et al[16] reported that LIPUS could increase the mineral density of cortical bone and improve the transverse bending strength of osteotomy model. In this study, it found that, after LIPUS treatment, the fusion rate of the observation group was 83.3% and it was significantly higher than the one of the control group (37.5%). Results of the comparison were statistically significant (P<0.05). According to X-ray film observation, after 4 weeks of treatment using the low-intensity pulsed ultrasound, the fusion in the bone grafting area of observation group was good. There was the relatively dense fusion area between
the right transverse process and artificial bone. The left transverse process had been completely fused, with the clear bone trabecula through the fusion area. There was no significant fusion sign in the control group. Afterwards, we compared the increase in the relative gray-scale and mean number of chondrocytes in the fusion area under the high-power lens between two groups before and after the treatment. Results showed that the number of chondrocytes and the increase in the relative gray-scale in the fusion area of the iliac observation group were significantly higher than ones of the iliac control group (P<0.05). The number of chondrocytes and the increase in the relative gray-scale in the fusion area of the artificial bone observation group were significantly higher than ones of the artificial bone control group (P<0.05). It indicated that the bone grafting fusion rate of the observation group receiving LIPUS treatment was significantly higher than the one of the control group without LIPUS treatment. LIPUS treatment could significantly increase the number of chondrocytes in the fusion area and the lumbar spinal fusion area after the treatment. The reason that LIPUS treatment could improve the fusion in the lumbar fusion area was that it increased the number of chondrocytes and promoted the endochondral ossification. The expression of inflammatory factors IL-1, IL-6 and IL-17 4 weeks after the treatment of the observation group was significantly lower than the one of the control group, with the statistical significance (P<0.05). It indicated that the treatment of lowintensity pulsed ultrasound could reduce the expression level of inflammatory factors.
In conclusion, the low-intensity pulsed ultrasound can significantly increase the bone grafting fusion rate of the rabbit’s posterolateral lumbar fusion. The possible mechanism to increase the bone grafting fusion rate is that it promotes the lumbar posterolateral endochondral ossification and reduces the inflammatory reaction.
Conflict of interest statement
We declare that we have no conflict of interest.
[1] Oh YM, Choi HY, Eun JP. Delayed retroperitoneal hemorrhage due to lumbar artery pseudoaneurysm after posterolateral lumbar fusion. J Korean Neurosurg Soc 2013; 54(4): 344-346.
[2] Koo KH, Lee JH, Chang BS, Lee CK. Effects of alendronate on posterolateral lumbar fusion using hydroxyapatite in rabbits. Artif Organs. 2012; 36(12): 1047-1055.
[3] Ohtori S, Inoue G, Orita S, Yamauchi K, Eguchi Y, Ochiai N, et al. Teriparatide accelerates posterolateral lumbar fusion in women with postmenopausal osteoporosis: prospective study. Spine (Phila Pa 1976) 2012; 37(23): E1464-E1468.
[4] Koo KH, Yeo do H, Ahn JM, Kim BS, Kim CS, Im GI. Posterolateral lumbar fusion using heparin-conjugated fibrin for sustained delivery of bone morphogenic protein-2 in a rabbit model. Artif Organs 2012; 36(7): 629-634.
[5] McGuire RA, Pilcher LE, Dettori JR. Posterolateral lumbar fusion with local bone graft plus bone extender compared with iliac crest bone graft: a systematic review. Evid Based Spine Care J 2011; 2(2): 35-40.
[6] Wang Z, Sakakibara T, Sudo A, Kasai Y. Porosity of β-tricalcium phosphate affects the results of posterolateral lumbar fusion. J Spinal Disord Tech 2013; 26(2): E40-E45.
[7] Hwang CJ, Vaccaro AR, Hong J, Lawrence JP, Fischgrund JS, Alaoui-Ismaili MH, et al. Immunogenicity of osteogenic protein 1: results from a prospective, randomized, controlled, multicenter pivotal study of uninstrumented posterolateral lumbar fusion. J Neurosurg Spine 2010; 13(4): 484-493.
[8] Cui C, Zhu Y, Han XX. Meta-analysis of posterolateral lumbar fusion versus circumferential fusion in the treatment of the lumbar disease. Zhonghua Wai Ke Za Zhi 2009; 47(18): 1374-1378.
[9] Koshi T, Ohtori S, Inoue G, Yamashita M, Yamauch Ki, Suzuki M, et al. Posterolateral lumbar fusion inhibits sensory nerve ingrowth into punctured lumbar intervertebral discs and upregulation of CGRP immunoreactive DRG neuron innervating punctured discs in rats. Eur Spine J 2010; 19(4): 593-600.
[10] Suliman A, Wollstein R, Bernfeld B, Bruskin A. Robotic-assisted device in posterior spinal fusion for a high risk thoraculombar fracture in ankylosing spondylitis. Asian Spine J 2014; 8(1): 64-68.
[11] Wu G, Chen L, Zhu G. Low-intensity ultrasound accelerates mandibular implant bone integration in dogs with mandibular osteoradionecrosis. J Surg Res 2013; 182(1): 55-61.
[12] Choi WH, Choi BH, Min BH, Park SR.. Low-intensity ultrasound increased colony forming unit-fibroblasts of mesenchymal stem cells during primary culture. Tissue Eng Part C Methods 2011; 17(5): 517-526.
[13] Vaughan NM, Grainger J, Bader DL, Knight MM. The potential of pulsed low-intensity pulsed ultrasound to stimulate chondrocytes matrix synthesis in agarose and monolayer cultures. Med Biol Eng Comput 2010; 48(12): 1215-1222.
[14] Korstjens CM, Van der Rijt RH, Albers GH, et al. Low-intensity pulsed ultrasound affects human articular chondrocytes in vitro. Med Biol Eng Comput 2008; 46(12): 1263-1270.
[15] Wang Q, Gou SH, Liu Y, Ouyang YP, Liang W, Han QL, et al. Biomechanical study on low-intensity pulsed ultrasound in promoting fracture healing, Academic J Second Milit Med Univ 2004; 25(6): 658-660.
[16] Hantes ME, Mavrodontidis AN, Zalavras CG, Karantanas AH, Karachalios T, Malizos KN.. Low-intensity transosseous ultrasound accelerates osteotomy healing in a sheep fracture model. Bone Joint Surg Am 2004; 86-A(10): 2275-2282.
ment heading
10.1016/S1995-7645(14)60190-5
*Corresponding author: Lei Chen, Rizhao, Associate Chief Physician, M.D., 3rd Department of Orthopedics, Rizhao People’s Hospital Affiliated to Shandong University, Rizhao 276826, China.
E-mail: chenleisd1969@126.com
杂志排行
Asian Pacific Journal of Tropical Medicine的其它文章
- Inhibition of advanced glycation endproducts formation by Korean thistle, Cirsium maackii
- Anti-hypercholesterolemic effect of kenaf (Hibiscus cannabinus L.) seed on high-fat diet Sprague dawley rats
- Susceptibility to temephos, permethrin and deltamethrin of Aedes aegypti (Diptera: Culicidae) from Muang district, Phitsanulok Province, Thailand
- Cloning, expression, purification and bioinformatic analysis of 2-methylcitrate synthase from Mycobacterium tuberculosis
- Prevalence of shiga toxins (stx1, stx2), eaeA and hly genes of Escherichia coli O157:H7 strains among children with acute gastroenteritis in southern of Iran
- Larvicidal, ovicidal and repellent activities of marine sponge Cliona celata (Grant) extracts against Anopheles stephensi Liston (Diptera: Culicidae)