Effectiveness of an employment-based smoking cessation assistance program in China
2015-12-06PeizhongLiChristopherLarrisonRichardLennoxMattMollenhauerDavidSharar
Peizhong Li, Christopher Larrison, Richard Lennox, Matt Mollenhauer, David A. Sharar
1. Chestnut Global Partners,China, Shanghai, China
2. Healthcare Performance Consulting representing Cease Smoking Today, Indianapolis,Indiana, USA
3. Chestnut Global Partners,Bloomington, Illinois, USA
Effectiveness of an employment-based smoking cessation assistance program in China
Peizhong Li1, Christopher Larrison2, Richard Lennox3, Matt Mollenhauer3, David A. Sharar3
1. Chestnut Global Partners,China, Shanghai, China
2. Healthcare Performance Consulting representing Cease Smoking Today, Indianapolis,Indiana, USA
3. Chestnut Global Partners,Bloomington, Illinois, USA
Objective:The objective of this study was to adapt an evidence-based smoking cessation intervention initially developed in the United States to the Chinese context and evaluate the effectiveness of this intervention in China.Method:A smoking cessation program from United States was adapted and implemented through an Employee Assistance Program (EAP) in China. The intervention consisted of recommending medication and psychological counseling. Local EAP counselors
training on the program and delivered the intervention to clients. Program evaluation examined the intervention's effectiveness in helping clients quit or reduce the amount of smoking and nicotine dependence.Results:Ninety-day follow-up showed that those who had completed the program were more likely to remain abstinent, or stop smoking daily and have lower levels of nicotine dependence(p< 0.05) than those who had dropped out.Conclusions:The evidence-based cessation program is effective in helping Chinese smokers quit or reduce the amount of smoking. Moreover, implementing such programs in an EAP setting is a practical approach to providing a wider spectrum of smokers with access to cessation assistance in China.
Smoking cessation; employee assistance program; program evaluation
Introduction
The World Health Organization has identified cigarette smoking as one of the most lifethreatening health problems worldwide [1].In developing countries, smoking-related diseases place a greater strain on the health care systems, which are often inadequate and fragile [2–4]. The need for smoking reduction and cessation has a special urgency in developing countries [1]. China is unequivocally the main battleground for combating the smoking epidemic [2–4]. Indeed, China is host to the world's largest cigarette manufacturers and population of smokers. According to the WHO's Global Adult Tobacco Survey, China has 301 million smokers. Among Chinese≥15 years of age, 52.9% of males and 2.4% of females smoke and 85.6% of smokers smoke cigarettes daily [2]. The trend in the country's effort to control and reduce smoking is far from optimistic; there was almost no reduction in the male smoking rate from 2002 to 2010,while the smoking rate among young women increased [2].
Inadequate information and education is in part to blame for China's smoking epidemic.Many people in the country are unaware or unclear of the impact of smoking on their health. More than three-fourths of Chinese respondents to the WHO 2010 survey lacked adequate knowledge about the harm of first-hand smoke,while two-thirds of the respondents were misinformed about the effects of second-hand smoke [2]. Eighty-six percent of respondents, including 54.7% of the physicians surveyed,did not realize that the claim "low tar equals low harm" is false. Awareness of the harm of smoking is inadequate, even among health care providers, hindering their ability to play an active and effective role in smoking cessation [2]. Among current smokers who visited physicians within the last 12 months, only 40.8% were asked about tobacco use and only 33.9% were advised to quit [2]. In other words, nearly 60%of smokers were not even asked about tobacco use when they visited their physicians.
Smokers who are motivated to quit face serious obstacles. Effective assistance from health care providers is seriously lacking in China. According to the WHO 2010 survey,among the 36.4% of Chinese smokers who had attempted to quit within the last 12 months, 91.8% had received no cessation assistance [2]. Left to combat the smoking addiction on their own, a large percentage (33.1%) of those who try to quit resume smoking [2]. Smoking is a stubborn addiction that takes more than willpower to cease [5]. Introducing effective assistance programs to help smokers quit is important in China [6]. Fortunately, evidence-based cessation assistance programs have been established in developed countries, such as the United States [7]. The smoking rates in developed countries have been declining due to effective intervention, as well as increased public awareness [8]. Introducing these programs with appropriate cultural adaptation will improve smoking reduction efforts in China and reduce the gap in cessation across the globe.
Efforts to provide cessation assistance exist in China, but face considerable difficulties. The Chinese health authorities have mandated large public hospitals in major cities to set up cessation clinics that provide medication and counseling for smokers trying to quit [9]; however, these facilities are underutilized. Few smokers use cessation clinics for cessation assistance, with the exception of patients with heart diseases awaiting surgery. One reason for the underutilization of cessation clinics is the cost for medication and counseling[10], which are not covered by medical insurance and must be paid out-of-pocket by smokers [7]. Another possible reason for smokers' reluctance to use cessation clinics is the perception of the onerous process of getting help at large public hospitals,which tend to be overcrowded and inadequately staffed and equipped. Making the assistance more affordable and accessible will help more smokers use those services. This goal may be achieved by leveraging the infrastructures and resources of Employee Assistance Programs (EAPs) for providing cessation assistance. As a result of economic growth and integration with the global economy, more and more employers in China are starting to provide EAPs, which offer a useful vehicle for launching health improvement services, including smoking cessation. EAPs are an employment benefit to help employees and their families with a variety of personal concerns that may have negative effects on job performance. A large proportion of employees' personal and family issues that EAPs offer assistance with are related to mental and behavioral health.
EAPs have multiple advantages in providing smoking cessation assistance in China. First, as a health benefit paid for by employers, services through EAPs are low cost to employees, thus reducing the financial barrier for those covered in EAPs to use mental health services, including smoking cessation assistance. Second, the EAP infrastructures offer employees easy access to smoking cessation assistance. Most EAPs operate call centers that offer 24-h, 7 day-a-week hotlines to provide evaluation, counseling, and scheduling of further assistance for clients' employees. Employees seeking smoking cessation assistance may use the same hotlines to contact counselors. Measurement and evaluation of the program's effectiveness can also be implemented through the call centers. Third, EAPs employ on-staff and affiliate mental health counselors, with effective systems and resources for organizing counselor education activities. These professionals may be educated on best practices to work with clients on smoking cessation. The counselors' affiliation with an established EAP ensures their competence in providing mental and behavioral health guidance have been properly evaluated, and that they receive continuous professional supervision.
Introducing effective cessation assistance through employment-based health systems, such as EAPs, is an attractive approach to smoking reduction in China. The current research evaluates the feasibility and success of such an effort. A team of US and Chinese clinicians and researchers have adapted a cessation program that has been developed and validated in the US, transferred the knowledge and skills for implementing the program to Chinese behavioral health professionals,and tested the interventions in China. Chinese counselors first received training on cessation assistance, then used those methods to help clients quit smoking. The researchers systematically evaluated the effectiveness of the adapted messages,tools and resources, the outcomes of clinician education with respect to changes in knowledge and skills in delivering cessation assistance, as well as the efficacy of the intervention as measured by quit rates and reduction in nicotine dependence.The project consisted of four components (localization of the program materials and resources, counselor education, service delivery, and program evaluation). Each component has established key activities, expected outcomes, and methods of evaluation.
Localization of the assistance program
The intervention adopted in this study follows the best practices established in the US Public Health Service Guideline(Clinical Practice Guideline: Treating Tobacco Use and Dependence 2008 Update) [7]. The assistance targets the key factors contributing to smoking and preventing smokers from quitting, i.e., the smoking habit, psychological dependence,nicotine addiction, and relapse. The counselor reinforces the clients' motivation to quit and help them establish realistic and effective quit plans, including the designation of a quit day and identifying the situations that trigger smoking and maintain the habit, such as daily routines, socialization, and stressful moments. Stress management receives special attention in the counseling because many clients use smoking as a coping strategy. Two methods were introduced to clients for combating nicotine dependence, i.e., medication and tapering.Two types of medications have been approved by the Chinese Food and Drug Administration and its counterpart in the US.One type consists of nicotine replacement products, including patches and gums. These are classified as over-the-counter or non-prescription medications in China and the US. The other type of medication includes varenicline and bupropion SR,which are classified as prescription medications and dispensed through cessation clinics at public hospitals. Both the overthe-counter and prescription medicines effectively reduce withdrawal symptoms during cessation attempts and pose acceptable risks to users [7, 11]. The second method for combating withdrawal symptoms involves tapering [7, 11]. The client is instructed to reduce the amount of smoking from the beginning of the counseling, e.g., by one-half every week in order to get ready for complete cessation by the time of the quit day. The counselors help clients cope with slips and relapses by treating the sense of setback, finding out the reason for the failed cessation attempts, developing effective coping strategies, and motivating the clients to set a new quit day. This protocol is implemented during a series of telephonic counseling sessions, each lasting for 1 h. Each client typically receives six sessions of counseling.
The original US cessation program developed extensive educational materials and resources for clinicians to help smokers quit. These materials were translated and adapted for Chinese health care providers by a team of professionals from US and China. The US team consisted of experts with in-depth knowledge and expertise in the content of the program. The Chinese team consisted of mental health professionals who are bilingual (Chinese and English). Considerations were given to cultural norms, needs, and lifestyles of Chinese clients, as well as the competence and knowledge of local counselors.Medication and counseling recommendations were customized based on local availability.
Counselor education
Eight full-time counselors at a local EAP received training on the cessation program with experts from the US serving as the faculty. The training started with 3 days of face-to-face instruction conducted by US experts, including lectures, casebased small group discussions, and interactive skill-building workshops. This was followed by web-based meetings and conference calls for consolidation of the knowledge and skills.Subsequently, the counselors implemented the program, helping clients quit smoking. Throughout the implementation period, the counselors held weekly peer-supervising sessions to share experiences and discuss issues encountered. The counselors also received monthly group supervision from the US experts. Individual supervision with the US experts was arranged as needed. Success of counselor education was evaluated with two methods, i.e., practice assessment interviews and knowledge assessments.
Practice assessment interviews
The counselors went through the Practice Assessment Interview twice (before and after training). The counselors'mastery of the cessation assistance techniques was scored using a rubric with best practices. The rubric consisted of three sections that measured different sets of outcomes, as follows:(1) the counselors' perception of the importance of treating tobacco use and their confidence in completing this activity;(2) their current practice in addressing tobacco use among their clients in general; and (3) their current practice in cessation counseling in particular. In the first section, the counselors rated their (1) perception of the importance of addressing clients' tobacco use, (2) confidence in advising clients of the danger of smoking and the advantage of quitting, and (3) confidence in assisting someone developing a quit plan. The counselors rated themselves on these dimensions on scales of 0–10.In the second section, the counselors reported their current practice with respect to tobacco use among their clients. More specifically, the counselors reported whether or not they (1)asked every client on every call about tobacco use, (2) advised all tobacco users to quit with clear, strong, and personalized language, (3) assessed every tobacco user's willingness to quit, and (4) would motivate a client to quit even if he/she was unwilling to give up smoking at the moment. For each of these questions, the counselors indicated "yes or no." If the answer was "no," the counselors were asked to explain the answer. In the third section, the counselors reported their current practice in helping clients quit smoking. More specifically, the counselors reported whether or not they implemented the following key activities in their cessation assistance counseling: (1) helping the client develop quit plans; (2) encouraging the client to remove tobacco products from their environment; (3) assisting the client to get support from family, friends, and co-workers; (4) reviewing past quit attempts (what helped and what led to relapse); (5) assisting the client to anticipate challenges,particularly during the first few weeks; (6) teaching the client how to cope with triggers to smoke; (7) assisting the client to identify reasons for quitting and benefits of quitting; (8) giving advice on successful quitting; (9) encouraging the use of medication; (10) selecting the appropriate medication for the client; (11) providing resources, such as quitlines; (12) arranging for follow-up visits to review progress toward quitting; and(13) encouraging repeat quit attempts if relapse occurs.
Seven of the eight trained counselors completed both interviews. The training produced uneven effects on the three sets of outcomes. The counselors' perceptions of the importance of treating tobacco use and confidence in doing so showed little change from before and after the training. In both interviews,the counselors scored close to the mid-point on the scale regarding the importance of addressing tobacco use. Treating tobacco use were not their top priorities in counseling and the training had little impact in changing this attitude. The counselors' confidence in advising the danger of smoking did not change from before to after the training, nor did their confi-dence in helping clients develop quit plans.
The counselors reported little change in their current practice in addressing tobacco use in their clients in general.Before training, none of the counselors asked every client on every call about tobacco use or advised all smokers to quit.After training, none of the counselors asked every client on every call about tobacco use, while only one of the counselors advised all smokers to quit. Before training, none of the counselors assessed every smoker's willingness to quit, while one of the counselors did so after training. One person would motivate smoking clients to quit even when the client was unwilling to quit both before and after training. The counselors attributed the reason for their lack of initiative in addressing the smoking problem to the standard practice of EAP counseling,which tends to focus on the issue(s) that the client brings up.The EAP counselors are reluctant to bring up smoking unless the issue was raised by the clients themselves, for fear of being considered as side-tracking or imposing the issue of smoking on the client, a situation that might affect the client's satisfaction with the quality of counseling.
In contrast, the counselors showed dramatic changes in their current practice in cessation counseling. Before the training, none of the counselors had ever assisted clients to develop quit plans, while all of the counselors did so after the training. Before the training, none of the counselors implemented any of the 13 key cessation assistance activities sampled in the interviews, while all of the counselors implemented those activities, with the exception of the activities related to recommending medication and providing external resources, such as quitlines. Before the training, none of the counselors recommended medication, while two of the counselors reported doing so after the training. None of the counselors referred clients to external resources for cessation before or after training. The reason cited for not doing so was lack of availability(see next section for details).
Knowledge assessment
We conducted written assessments on the counselors before and after training to evaluate changes in the counselor' knowledge and skills in smoking cessation assistance. Six of the eight trained counselors completed both assessments. An additional counselor completed the second assessment only.The first assessment took place 1 week before the training to establish a baseline, while the second assessment took place 3 months after the training to evaluate changes. The questions in both assessments were divided into two parts. The first part of both assessments was identical, consisting of four questions designed to sample the counselors' knowledge related to smoking cessation. More specifically, these questions tested if the counselors knew the following: (1) smoking is the leading cause of death and disability worldwide; (2) the most prevalent illness caused by smoking; (3) the number of smokers in China; and (4) the significant consequences of smoking. The results from this part of the first assessment indicated that the counselors had inadequate cessation-related knowledge before training. One-half of the counselors did not know that smoking is the leading cause of death and disability worldwide.None of the counselors knew that the most prevalent illness caused by smoking is heart disease. On average, the 6 counselors answered 53.57% of the questions correctly. After the training was completed, the counselors answered 64.29% of the questions correctly.
The two assessments differed in the second part. The second part of the first assessment consisted of case scenarios that tested the counselors' knowledge in developing quit plans and providing guidance to help smokers quit. The questions covered knowledge in selecting the most effective strategies for quitting, coping with slips and relapses, managing stress, and using medication. The counselors correctly answered 67.35%(SD=35.68%) of these questions, suggesting that the counselors were somewhat knowledgeable about the basic strategies for helping clients quit smoking before training. These questions were not repeated in the second assessment.
The second part of the second assessment consisted of open-ended questions. Specifically, the counselors were asked the following: (1) what they liked about the training; (2) what improvements they thought should be made to the training;and (3) what other topics they would like to discuss. Five of the seven counselors said they liked the role-play practices based on case scenarios provided by the trainers. The counselors also mentioned the interactive format of the training and the detailed information and useful materials they received.With respect to possible improvements in the training, six of the seven counselors who completed the assessment indicated they would like to have more role-plays, scenarios, and case descriptions to learn how to do cessation counseling. Two counselors answered the question about other topics they would like to discuss. Both of the counselors would like to receive supervision in their cessation assistance practice from the trainers.
In summary, the results from the two parts of the exams indicate significant changes in the counselors' practice in working with smokers who are trying to quit smoking. The counselors successfully implemented the techniques for the intervention, suggesting that the training was successful; however, the counselors' perceptions of the importance of addressing tobacco use in their daily work did not change after the training, nor did their confidence in doing so.
Cessation assistance and program evaluation
The EAP offered the smoking cessation program to the employees of 8 current clients free of charge between 1 June and 31 December 2014. These corporate clients included both multinational and local companies. EAP account managers collaborated with client contacts to publicize the free smoking cessation program among employees. The promotion included putting up posters in public areas in the workplace(e.g., employee cafeterias and dedicated smoking areas), circulating e-mails from Corporate Health or Human Resources Departments, and posting notices on the EAP website. Current smokers who were willing to quit within the next 30 days were invited to participate in the program. During this period,228 current smokers contacted the EAP call center to express an interest in the program and willingness to quit smoking within the next 30 days. The call center staff provided information about the program and later contacted each of those callers to set up an appointment with a cessation counselor.A total of 147 (64.47%) of the candidates scheduled the first appointment with a counselor. The remaining candidates(n=71) either changed their mind about cessation and declined the invitation to participate or simply could not be reached.
For each individual client, the cessation program consisted of three components, i.e., baseline assessment, intervention,and follow-up. The baseline assessment was completed by the cessation counselor verbally during the first session after obtaining informed consent, whereas the follow-up was completed at least 90 days after the quit day or the day of withdrawal in cases when the client dropped out before setting a quit day, with a mean of 130.27 days (SD=33.59). The baseline and follow-up assessments gathered information on the client's smoking status for calculating quit rates and a measurement of nicotine reliance. The smoking status information included the following: (1) whether or not he/she smoked cigarettes daily; and (2) the number of cigarettes he/she smoked per day. Nicotine reliance was measured with the Fagerstrom Nicotine Reliance Rating [12]. The six-item instrument gives raw scores ranging from 0 to 10. The Chinese Clinical Manual of Smoking Cessation [13] assigns scores from 0 to 3 as low,4–6 as moderate, and >7 as a high level of dependence. The intervention closely followed the protocol the counselors had acquired during the training, with two caveats (recommending medication and other resources, such as quitline). Nonprescription nicotine replacement medications are unavailable on mainland China, because the manufacturers had stopped supplying non-prescription nicotine replacement medications in the Chinese market, presumably because of a lack of demand. These medications were rarely used during the program (and only by a few employees who work for a multinational company that manufactures the products and employees who were able to obtain the products during overseas travel).The prescription medications are available sporadically at some of the cessation clinics in major cities but were not used in this program because of a lack of interest from the clients.The counselors used tapering as the primary method for helping clients overcome the withdrawal effects. Similarly, the counselors could not locate reliable resources outside of the EAP for cessation, such as quitlines.
Client characteristics
The 147 smokers who scheduled the first appointment consisted of 144 men and 3 women, with an average age of 32.61 years (SD=8.06). Because of the small number of women in the sample, gender was not included in subsequent analyses. In this sample, 111 individuals (75.51%) of the participants identified themselves as smoking daily, 16 individuals (10.88%) reported not smoking daily, while another 20 individuals (13.61%) did not give valid responses to this question. The daily smokers smoked 13.89 (SD=6.07) cigarettes each day when they entered the program.
Dropout rates
Among the 147 smokers who participated in the program,59 individuals (40.14%) of the group completed the program,while 88 individuals (59.86%) dropped out before the completion of the counseling. Dropout was defined as unilateral withdrawal from counseling by the client before he or she had successfully stopped smoking. Those who completed the program received an average of 5.69 counseling sessions(SD=0.93), with 66.10% and 15.25% of participants completing 6 and 5 sessions, respectively. Those who dropped out received an average of 1.70 counseling sessions (SD=1.23).The majority of the participants withdrew from the program during the first (27.27%) or second session (31.82%), when they reached the juncture of discussing a quit day with the counselor, while 18.18% could not be reached for the first appointment. In the group that completed the program, 94.92% set a quit day, whereas only 18.18% of those who dropped out were able to do so.
We compared those who completed the program with those who dropped out when they first entered the program. On average, the group that dropped out smoked slightly more cigarettes each day (mean=13.54, SD=6.55) than those who completed the program (mean=12.47, SD=6.61). The dropouts also had slightly higher nicotine dependence than those who completed the program (see later); however, independent sample t-tests showed that neither of these differences reached conventional levels of statistical significance (p>0.05). Both groups started with low-to-moderate levels of dependence when they entered the program. The main differentiator between the two groups appeared to be the clients' motivation to quit.
Quit rates and nicotine reliance
We examined the proportion of participants who had remained completely abstinent between their quit days and the follow-up date. Moreover, since client compliance is likely a key factor in successful cessation, we compared those who completed the program with those who dropped out. To date, 97 participants have completed the followup. Among the participants who completed the followup, 22.68% remained completely abstinent since their quit days, while 67.01% smoked during this time and another 10.31% did not give valid responses to this question. We compared the quit rates between those who completed the program and those who dropped out. In the 52 individuals who had completed the program and the follow-up,18 (34.62%) remained completely abstinent. In contrast,amongst the 45 individuals who had dropped out of the program, but completed the follow-up, only 4 (8.89%) remained completely abstinent. This difference between the two groups was statistically significant [χ2(2,n=97)=9.24,p=0.01].
Among the self-identified daily smokers before the intervention (n=111), 83 completed the follow-up. Within this group, 45 individuals (54.22%) stopped smoking daily,34 (40.96%) still smoked daily, and 4 individuals (4.82%) did not give valid responses to this question. Among the daily smokers who had completed the program and the follow-up(n=44), 32 (72.73%) stopped smoking daily at the follow-up date, while the others either continued to smoke daily or did not give valid responses to this question. In contrast, among the daily smokers who had dropped out of the program, but completed the follow-up (n=39), 13 (33.33%) had stopped smoking daily, while the others either continued to smoke daily or did not give valid responses to this question. This difference between those who completed the program and dropouts was statistically significant [χ2(2,n=83)=13.54,p<0.01]. A larger proportion ofthe daily smokers who had completed the program were able to stop smoking daily than those who had dropped out.
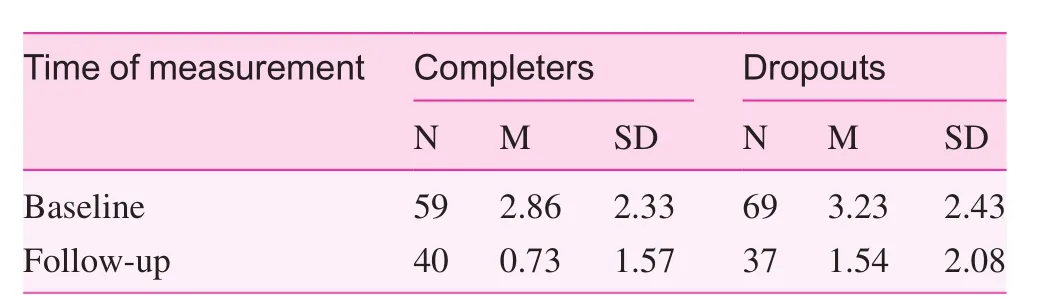
Table 1. Nicotine reliance between clients who completed vs.dropped out the program
We examined the changes in nicotine reliance measured on the Fagerstrom Nicotine Reliance Rating scale before and after the intervention. We also compared the groups that had completed or dropped out from the program. A two-by-two analysis of variance (ANOVA) with the reliance scores as repeated measures (before and after intervention) and completion of the program as a between-subject factor (completed vs.dropped out) revealed a main effect for the repeated measures[F (1, 75)=65.48,p<0.001]. In both groups, nicotine reliance dropped from before to after the intervention (see Table 1 for the means). The main effect for the completion of the program was not significant, nor was the interaction between pre- and post-test measures and the completion of the program(p>0.05); however, consideration of the means indicate that those who had completed the program experienced a greater reduction in nicotine reliance than those who had dropped out(Table 1). While the two groups did not differ significantly on reliance before the intervention [t(126)=0.87,p>0.05], those who completed the program showed lower reliance than the dropouts during follow-up, a difference that is marginally significant [t(75)=1.95,p=0.05].
General discussions
Employment-based cessation programs are innovative in China. This approach bypasses some hurdles preventing smokers from seeking cessation intervention, e.g., the cost and inconvenience in access to assistance. EAP infrastructures,such as a toll-free hotline, provide easy access to professional cessation assistance, while the cost of the counseling is covered by the employer. The implementation of this program showed that EAPs offer useful settings and resources for providing cessation assistance in China; however, several issues need to be taken into consideration in future developments of this approach. These issues relate to both implementing cessation assistance in an EAP setting and the effectiveness of the intervention used in this study.
EAP counselors' perceptions and practices with respect to cessation
The training and subsequent clinical intervention in this program have changed the EAP counselors' practices in assisting smokers who are seeking help to quit smoking. The counselors have mastered the techniques in the protocol and implemented the techniques in counseling clients. The clinician education part of the program has been successful in transferring the know-how and expertise developed in the US to Chinese counselors; however, even after the training and practice, the EAP counselors do not see smoking cessation as a prominent issue that they must address when they work with clients. The counselors take few initiatives to ask and advise clients about tobacco use during their everyday EAP counseling practice.
The reasons behind the sparse attention to smoking may be pragmatic, and related to the the role functions and responsibilities of EAP counselors in China. EAP counselors work in a setting where tobacco use is one of numerous personal issues they are trying to help clients solve. EAP counseling follows a short-term, solution-focused approach, with an emphasis on being helpful in six or fewer sessions, identifying specific problem areas and using direct intervention techniques. The counselors' performance is evaluated based on the satisfaction of the clients, who tend to focus on the counselor's ability for solving the problems they regard as urgent and important. The counselors focus on the issues that the client raise and try to solve, e.g., emotion control, family and marriage, parenting,and inter-personal relations. Most of the time tobacco use is not an issue that the clients are trying to solve. Under these circumstances, the counselor is reluctant to lead the client to review their tobacco use proactively for fear of being viewed as non-focused, non-responsive, or side-tracking by the client.This client-centered approach did not change after the training because it is dictated by the protocol of EAP counseling.
The above situation indicates that EAPs must collaborate with physicians and employer groups in China to provide multiple channels for patient education and intervention.International non-governmental organizations have already begun to work with employers in China to promote employee health, e.g., by offering accreditations to employers for best practices in cancer prevention. Smoking cessation is an integral component of such programs. Meanwhile, the Chinese Ministry of Health has also been promoting tobacco control and cessation in the workplace through consortiums of employers and in collaboration with universities in the US. These governmental and non-governmental efforts help bring multiple resources (e.g., physicians, EA professionals, and employers)to tackle the smoking epidemic in a systematic way; however,these efforts are very limited in scale and will have a long way to go before making a significant impact on the large number of smokers in China.
Client motivation and compliance as key factors in smoking cessation
Greater than one-third of the smokers who had initially signed up for the program withdrew, even before scheduling the first counseling appointment. Greater than one-half of those who scheduled appointments withdrew before completing the program. Most of the participants in this group withdrew during the first or second session before committing to a quit day.The reasons the participants gave for their withdrawal relate to a lack of motivation or self-efficacy for quitting. The participants claimed that their goals and expectations for the program were not to quit smoking completely, or that this was not the right time for doing so (e.g., tight schedules and job transitions). Some of the participants only wanted to reduce or control the amount they smoke. The participants were unwilling to commit to a firm date when they would stop smoking. This unwillingness to stop completely is buttressed with misperceptions of smoking. Some of the participants believed that they benefited from smoking, e.g., smoking helped them relax, socialize, or be individualistic. Some of the participants believed that they could control the amount of smoking, and that low-level smoking was not harmful. Research has shown that these misperceptions are widespread among Chinese smokers [14]. Some of the participants did not believe that they could ever stop smoking, so it was not worth trying.Research has shown that those misperceptions are widespread and tenacious among Chinese smokers. The counselors seem to be inadequately prepared to overcome these hurdles in the EAP setting, which emphasizes short-term interventions.Counseling itself may not be enough to combat those misperceptions because they are common and widespread in the society. Public education must be strengthened to correct the misperceptions and motivate more smokers to set the goal of quitting. Future programs should integrate the EAP cessation program with the client organization workplace wellness policies and health and productivity programs to provide public education on the harm of smoking and benefits of smoking cessation. For example, the cessation program should be integrated with the efforts of the client organization to create smoke-free workplaces or other health drives.
Availability of cessation assistance medication
The non-prescription patches and gums are not available in the marketplace, while the prescription medications are sporadically available, but are of limited interest among smokers and counselors alike. Under these circumstances, few clients used medications in this program. Tapering was the primary method for helping smokers cope with the withdrawal effects in quitting. The lack of availability of medication could make quitting more difficult for heavy smokers with greater nicotine dependence [7]. The good news is that the smokers in this study smoked 14 cigarettes per day on average. The average nicotine dependence level is between low and moderate on the Fagerstrom Reliance Rating scale. Withdrawal from nicotine may not be a serious problem and tapering may be sufficient,given sufficient motivation on the part of the smokers.
Quit rates and research methodology
Researchers have used various methods for calculating quit rates for cessation interventions [15]. In this study we calculated the quit rate by dividing the number of clients who had remained abstinent by the number of clients who had registered for intervention and received at least minimal treatment (one counseling session), as recommended by the North American Quitline Consortium [15]; however, our follow-up period was shorter than most studies from the US and other Western countries, which typically are 5 [7], 6 [16, 17], or 12 months in length [18]. The small number of studies with a focus on the impact of cessation programs with Chinese smokers in Hong Kong also reported 12-month quit rates [19].The aforementioned studies have reported quit rates ranging from 14% to 27% over the various follow-up periods, which is similar to what we have found in this study. Of course, it is difficult to compare the quit rate of this program with similar cessation programs due to the different follow-up periods.Moreover, the various efficacy studies differ with respect to frequency and intensity of counseling, as well as use of medications. Therefore, caution is warranted in comparing the quit rate we have observed in this program with other studies. In contrast, our results indicate that those who had completed the program benefited from the program to a greater extent that those who had dropped out. The participants who completed the program were more likely to stop smoking daily,remain completely abstinent during the follow-up period, and experience less nicotine reliance than the dropouts. This "dosage effect" suggests that the intervention is useful in helping the clients quit smoking. Ideally, we should have included the smokers who had called the hotline to sign up for the program, but did not schedule an appointment with a counselor in the study as a control group. In practice, however, it would be difficult to conduct baseline and follow-up assessments on these individuals who are disinterested in the program in an EAP setting.
Future research should use follow-up periods more similar to existing studies in the literature for comparative evaluations. A related methodologic issue is that this study used a quasi-experimental design to test the effectiveness of an education-based smoking cessation program. Ideally, the study would include a "no treatment" control group to demonstrate the causal effect of the intervention (independent of other factors, such as client motivation) in helping clients quit smoking;however, in most practical tests of behavioral health intervention, it is unethical to withhold treatment from employees who want to quit smoking. Despite these limitations, the study has taken a significant first step in understanding the impact of evidence-based smoking cessation programs in China in general, and in an EAP setting in particular.
Conflict of interest
The authors declare no conflict of interest.
Funding
This study was supported by an educational grant from Pfizer,Inc.
1. WHO. WHO Report on the global tobacco epidemic, 2013. World Health Organization; 2011. Available from: http://apps.who.int/iris/bitstream/10665/85381/1/WHO_NMH_PND_13.2_eng.pdf?ua=1.
2. WHO. Global adult tobacco survey, 2010 China country report.Geneva: World Health Organization; 2011. Available from:www.wpro.who.int/internet/files/chn/gats_china_report_en.pdf.
3. Sung H, Wang L, Jin S, Hu T, Jiang Y. Economic burden of smoking in China, 2000. Tobacco Control 2006;15 Suppl 1:i5–i11.
4. Wang L, Kong L, Wu F, Bai Y, Burton R. Preventing chronic diseases in China. Lancet 2005;366:1821–4.
5. American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed. Washington, DC: American Psychiatric Association; 2013.
6. Yang J, Hammond D, Driezen P, O'Connor RJ, Li Q, Yong H,et al. The use of cessation assistance among smokers from China: findings from the ITC China Survey. BMC Public Health 2011;11:75.
7. Fiore MC, Jaén CR, Baker TB, Bailey WC, Benowitz NL, Curry SJ, et al. Treating tobacco use and dependence: 2008 update.Clinical practice guideline. Rockville, MD: U.S. Department of Health and Human Services. Public Health Service; 2008.
8. Jha P, Peto R. Global effects of smoking, of quitting and of taxing tobacco. N Engl J Med 2014;370:60–8.
9. China's Plan for Tobacco Control (2012–2015). General Administration of Quality Supervision, and Quarantine of PRC;2012. Available from: www.aqsiq.gov.cn/xxgk_13386/jhgh/gh/201212/t20121221_335194.htm#_Toc24472.
10. Lam TH, Abdullah AS, Chan SS, Hedley AJ, Hong Kong Council on Smoking and Health Smoking Cessation Health Centre (SCHC) Steering Group. Adherence to nicotine replacement therapy versus quitting smoking among Chinese smokers: a preliminary investigation. Psychopharmacology(Berl) 2005;177:400–8.
11. Raw M, McNeill A, West R. Smoking cessation guidelines for health professionals. A guide to effective smoking cessation interventions for the health care system. Thorax 1998;53:S1–S18.
12. Heatherton TF, Kozlowski LT, Frecker RC, Fagerström KO.The Fagerström test for nicotine dependence: a revision of the Fagerström tolerance questionnaire. Br J Addict 1991;86:1119–27.
13. Wang C. Chinese clinical manual for smoking cessation. trial ed.Beijing: People's Medical Publishing House; 2007.
14. Ma S, Hoang MA, Samet JM, Wang J, Mei C, Xu X, et al. Myths and attitudes that sustain smoking in China. J Health Commun 2008;13:654–66.
15. North American Quitline Consortium, Measuring Quit Rates,NAQC Issue Paper, 2009. Available from: www.pdastats.com/PublicFiles/Naqc_Issuepaper_Measuringquitrates.pdf.
16. Town GI, Fraser P, Graham S, McSweeney W, Brockway K, Kirk R.Establishment of a smoking cessation programme in primary and secondary care in Canterbury. NZ Med J 2000;113:117–9.
17. Croghan IT, Offord KP, Evans RW, Schmidt S, Gomez-Dahl LC, Schroeder DR, et al. Cost-effectiveness of treating nicotine dependence: the Mayo Clinic experience. Mayo Clin Proc 1997;72:917–24.
18. Hurt RD, Dale LC, Fredrickson PA, Caldwell CC, Lee GA,Offord KP, et al. Nicotine patch therapy for smoking cessation combined with physician advice and nurse follow-up. One-year outcome and percentage of nicotine replacement. J AM Med Assoc 1994;271:595–600.
19. Abdullah AS, Lam TH, Chan SS, Hedley AJ. Smoking cessation among Chinese young smokers: does gender and age difference matters and what are the predictors? Addict Behav 2006;31:913–21.
Peizhong Li 555 West Guangzhong Road,Shanghai, China 200072
E-mail: Lipeizhong@eapchina.net
11 March 2015;
Accepted 29 March 2015
杂志排行
Family Medicine and Community Health的其它文章
- Team-based stepped care in integrated delivery settings
- The Accountable Care Organization results: Population health management and quality improvement programs associated with increased quality of care and decreased utilization and cost of care
- "Three essential elements" of the primary health care system:A comparison between California in the US and Guangdong in China
- Menopause and the risk of metabolic syndrome among middle-aged Chinese women
- Availability and social determinants of community health management service for patients with chronic diseases:An empirical analysis on elderly hypertensive and diabetic patients in an eastern metropolis of China
- Evaluating the process of mental health and primary care integration:The Vermont Integration Profile