Team-based stepped care in integrated delivery settings
2015-12-06CassandraSnipesAlexandrosMaragakisWilliamDonohue
Cassandra Snipes, Alexandros Maragakis, William O'Donohue
1. Department of Psychology,University of Nevada, Reno,1664 N. Virginia Street, Mail Stop 298, Reno, NV, USA 89557
2. Department of Psychiatry,University of Maryland School of Medicine, 701 W. Pratt Street,3rd Floor, Baltimore, MD 21201
Team-based stepped care in integrated delivery settings
Cassandra Snipes1, Alexandros Maragakis2, William O'Donohue1
1. Department of Psychology,University of Nevada, Reno,1664 N. Virginia Street, Mail Stop 298, Reno, NV, USA 89557
2. Department of Psychiatry,University of Maryland School of Medicine, 701 W. Pratt Street,3rd Floor, Baltimore, MD 21201
Fragmented health care delivery is recognized as increasingly problematic. Integrated care has been advanced as a reform that will improve quality of care and lower costs. Despite the application of integrated care systems in the United States, there has been a limited amount of empirical work explicating the most effective health care pathways. Stepped care has been proposed as a framework by which to implement coordinated team-based care and has gained preliminary empirical support. In this manuscript a rationale for team-based stepped care is presented, tools for implementation are provided, and future research directions are suggested.
Integrated care; team-based care; behavioral health in primary care
Introduction
Fragmented care has been identified as one of the major contributors to high health care costs,as well as increasing the likelihood of medical errors [1]. Fragmented care is thought to occur when different specialties operate in "silos"and do not communicate or coordinate care of a particular patient. Non-fractionated care attempts to coordinate care so there are no gaps or duplications in patient care. Indeed, there are a number of costly problems associated with fragmented care. First, there is often poor communication between providers, who have a variety of core competencies, all of which can be critical for establishing the correct diagnosis,treatment planning, and treatment implementation. Poor communication can result in inadequate diagnoses and treatment (e.g., failure to identify potential drug interactions). Second,behavioral health correlates of physical disease are often not addressed due to the fact that primary care providers (PCPs) do not have comprehensive training in detection or treatment of these problems. Furthermore, when behavioral health concerns are addressed, patients often do not follow through with external referrals to specialty care due to factors, such as perceived stigma, and geographical and financial constraints [2–4]. Behavioral health problems that are left untreated are associated with a host of adverse events, including suicide, school failure, teenage pregnancy,chronic medical problem exacerbation, unstable employment, marriage at an early age,marital instability, and domestic violence [5].Fragmented care is not only costly, but can be unsafe and of low quality; however, coordinating care across a wide variety of professionals,and even across a large number of settings, can be a challenging task.
Integrated care
Integrated care (IC), which for our purposes herein involves behavioral health care providers and PCPs working in interdisciplinary teams, has been proposed as a solution to increase multidisciplinary collaboration, reduce medical errors, and improve patient access to quality care [6, 7]. IC is theorized to improve quality of care in multiple ways. First, patients in the primary care setting have immediate access to behavioral health experts that specialize in somatic or behavioral health concerns. This is important because individuals who arrive in the primary care setting often present with co-morbid behavioral and somatic issues that complicate their medical care or may be a major reason for their presentation [8]. The behavioral health issues include depression, anxiety, obesity,chronic pain, treatment adherence, stress, parenting difficulties, chronic disease management, and severe mental illness.Second, multidisciplinary teams can promote collaborative treatment plans, decrease redundancies, provide more comprehensive diagnosis and treatment, and provide a clinical pathway for addressing behavioral health problems, which are often missed by PCPs [9]. Finally, the integration of behavioral health providers in the primary care setting allows for PCPs to "hand off" behavioral health concerns that are typically time-consuming, and beyond the scope of their medical practice or interests. Thus, there is more efficient use of PCP time, which leads to higher levels of productivity and work satisfaction [8]. This process is sometimes referred to as "the physician leveraging effect," and has been shown to increase physician satisfaction and productivity [10].
Because of these factors, IC promises to be a major factor in health care reform; however, systematic investigation of how these multidisciplinary teams can operate most effectively is needed. For example, population health management, which involves preventive education and treatment for high incidence disorders, such as diabetes, obesity, hypertension, and smoking, is a model that allows providers to disseminate care to a large number of patients in an efficient and low-cost manner.IC is sometimes thought of as "low touch, high volume," much like primary care medicine.
The utility of population health management may be lost because PCPs may not always view some of these somatic concerns (e.g., diabetes and obesity) as having important behavioral components. The creation and investigation of standardized clinical models and pathways for patients to access these low-cost interventions would provide an avenue for health care systems to address drivers of health care costs(i.e., preventable disease) in a cost-efficient manner. Another problem in integrated health care delivery that requires further examination involves IC relying on brief individual treatment models, and not consistently using stepped care approaches[11]. The consistent use of multiple individual appointments to address behavioral health issues may not necessarily be required for all behavioral issues (e.g., sub-clinical levels of depression or anxiety), and certainly limits the productivity of the clinician (for a further discussion of clinician productivity, see O'Donohue et al. [12]). Therefore, further examination of other modalities of delivering behavioral health care in IC settings (e.g., eHealth, telehealth, and bibliotherapy)and how these interventions fit within a larger stepped care model of IC may prove useful. A final difficulty in IC is that we currently do not have a metric that can evaluate the extent to which team-based care actually occurs. While providers are often co-located and work from the same electronic health records, there are no systems that ensure multiple providers are appropriately involved in the same treatment plan, which may lead to inefficiencies and reduce the overall benefit of the IC model. Indeed, an important related problem is identifying when team-based care is not necessary. Team-based care is expensive and inefficient for very simple medical problems,such as evaluating a child for streptococcal pharyngitis, and if positive, prescribing antibiotics. Therefore, while IC is a step forward in the provision of care, IC has room to improve as a model of care.
Team-based stepped care
For IC to be most effective and efficient, care should be implemented in a stepped fashion [13, 14], and this framework is consistent with the way medical treatment is usually delivered in primary care settings. Specifically, more complex and expensive interventions should only be used when simpler,reasonable interventions have been shown to be inadequate[11, 13]. Stepped care posits that providers offer care that achieves the following: 1) minimal disruption in the patient's life; 2) least extensive required for a reasonable probability of producing positive results; 3) least intensive for positive results, especially with respect to the side effect profile; 4) least expensive for positive results; 5) least expensive with respect to staff training and involvement required to provide effective service [11]; and 6) most efficient with respect to team-based IC (i.e., uses all the professionals necessary and none that are unnecessary). These attributes of stepped care contribute to increased patient choice, an opportunity for increased coordination between interdisciplinary team members, and better accomplish medical cost offset.
A brief outline of stepped care for depression follows:
1.Watchful waiting(for very low level, perhaps subclinical reactive depression, such as a break-up of a relationship);
2.Psychoeducational interventions(a brochure on behavioral activation, seeking social support and exercise is given for mild depression);
3.Ehealth(the patient is referred to excellent evidencebased ehealth sites, such as the Australian Beacon sites);
4.Bibliotherapy(the patient is referred to excellent evidence-based self-help books, such as Burn'sFeeling Good);
5.Group psychotherapy(the patient is referred to an ongoing cognitive behavioral mood management group where >10 patients can be treated simultaneously);
6.Individual psychotherapy(for more severe depression);
7.Medication intervention(for more severe depression and patient preference); and
8.Inpatient treatment(for the most severe depression,which may be associated with substantial suicidality).
Improved patient choice
Stepped care offers the patient the greatest choice of interventions. For example, a patient may not feel comfortable navigating online treatment and may prefer to engage in bibliotherapy.In the case of a severely ill patient, the patient has access to consultation on the potential benefit of anti-depressants versus individual psychotherapy or a combination of anti-depressants and psychotherapy via interaction with the multidisciplinary care team. Enhanced patient choice renders integrated stepped care "consumer-centric."
Enhanced coordination
Integrated stepped care is a common language by which all team members can be involved in triage, coordination, and treatment. Most PCPs are trained to provide intervention in a stepped manner.
Population management
Population health management is the application of interventions to defined groups of patients in an effort to improve the health of the individuals within the group at the lowest cost [15]. Through identification of patient severity, stepped care delivers the least invasive and least costly intervention to patients overall. In addition, those patients identified as severely ill or high utilizers of health care services can be targeted to receive the highest level of professional care and optimally use the team resources, and resources are not overutilized with patients who do not require intensive care.
Medical cost offset
Through implementation of integrated stepped care, and therefore population management, medical cost offset is more likely to be achieved than in traditional IC. In fact, IC has been shown to reduce costs by approximately 20% overall across a range of implementation approaches [16]; however, in some cases IC fails to deliver medical cost offset [17] due to a number of systemic challenges. Team-based stepped care can address these problems by allocating collaborative resources in the most effective manner. Specifically, team-based stepped care aims to neither over- or under-treat.
Evidence in support of team-based stepped care
It has been demonstrated that collaborative stepped care is a feasible and effective system of care. Stepped care has been shown to be more cost effective relative to treatment as usual (TAU) in the treatment of anxiety disorders [18]. This treatment modality has also been shown to improve outcomes and patient satisfaction in the treatment of depression[19–21]. Stepped care has also been shown to increase the population impact of post-traumatic stress disorder treatment [22]. Team-based stepped care has proved to be successful; however, further research explicating care pathways is critical.
The problem of team-based assessment and triage
Stepped care can accomplish better coordination, at least in part because stepped care provides a consistent model of intervention for all team members; however, potential pitfalls related to stepped care assessment and triage remain. Team members may disagree regarding patient severity. For example, in the case of a patient with obesity, a behavioral health consultant (BHC) may suspect depression to be a precipitating factor in weight gain and propose treatment for depression in order to promote weight management. Alternatively, the PCP may conclude that the depression does not reach the threshold necessary for intervention and may propose services from a dietician as the frontline intervention. Second, members of the team may disagree regarding what is the least invasive intervention. In the preceding example, the PCP may propose a low-dose anti-depressant as the least intensive intervention,while the BCP may advocate for a treatment group or eHealth intervention. Finally, communication regarding assessment and triage must be resolved. With the PCP acting as the team"quarterback," do all stepped care treatment decisions need to be cleared with this provider before implementation? Can a BCP implement an intervention and discuss the intervention with the PCP after the visit? Is it important that this communication be in person?
Although some of the aforementioned problems are open empirical questions, such as the best way to accomplish team communication, there are strategies that can resolve team stepped care assessment and triage problems, as follows:1) elicit patient preference when deciding between two reasonable interventions; 2) follow existing clinical guidelines; 3)implement a first course of treatment and use watchful waiting to determine the success of this treatment plan (i.e., have responsive treatment plans); and 4) PCP has the ultimate say as the team "quarterback."
Implementation
The clinical care team
A significant amount of success in an integrated care system depends on the type of providers that comprise the multidisciplinary team. At a minimum, a care team must include a PCP and a psychologist to treat both primary and behavioral health issues. In the optimal scenario, these professionals would be joined by a care manager, psychiatrist, health behavior coach,a social worker, nurses, dietician, and dentists (see Table 1 for examples of roles). Without varying levels of providers, the levels of stepped care can be successfully implemented due to the fact that providers would be "underemployed." For example, without a health behavior coach, the psychologist may be required to complete telehealth calls or to provide psychoeducation, responsibilities that can be successfully accomplished by a lower level provider.
Coordination of the clinical care team is of the utmost importance. The PCP should always act as the "quarterback"of the team; the PCP is the hub that the other members of the team revolve around. Thus, the patient remains a patientof the PCP and the other team members serve as consultants.The PCP has the ultimate responsibility for approval of the patient care plan. This burden of coordination drains professional time and the PCP must be supported by a care manager.
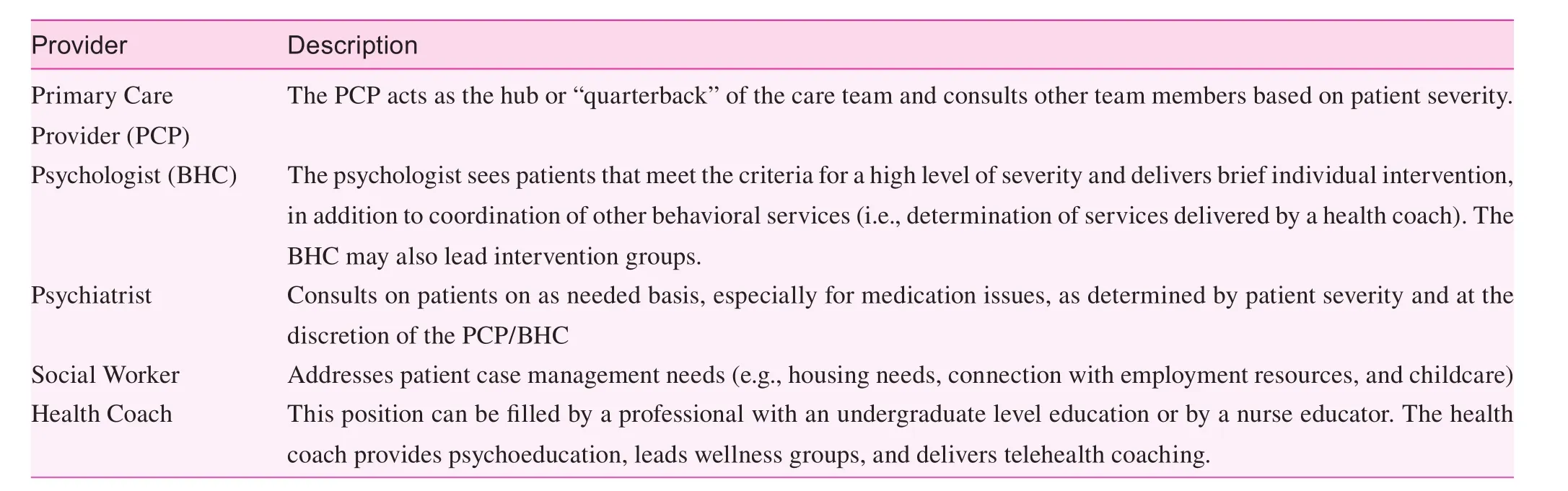
Table 1. Example of multidisciplinary team member roles and responsibilities
One or more care managers should coordinate team care and assign patient severity (a discussion of severity assignment is detailed below). Patient severity also dictates the mode of delivery of stepped care (sequential or staffed care).Sequential care is characterized by receipt of intervention from team members one after another (i.e., a visit with the PCP results in a hallway handoff to the BHC) and is used for less complex patient presentations. Complex patient presentations, as rated by the care manager and or PCP, should by staffed by the team. Specifically, care of these patients is discussed and coordinated in weekly or biweekly care team meetings.
Importance of screening
To attain proper recognition of patient severity, effective screening is imperative. Screening should capture a wide variety of behavioral health issues (e.g., depression, anxiety,and alcohol and substance abuse), physical health issues (e.g.,concerns regarding sleep and weight), and problems of living (e.g., financial or legal issues). Effective screening aids in problem identification and subsequently supports assessment of patient severity. It is imperative that stepped care screening be comprehensive to thoroughly characterize patient dysfunction. This process serves to inform which members of the team should have contact with the patient and is team-based because the PCP and/or the care manager review the screening measure to direct the patient to services. This may result in a "warm handoff" to the BCP or other appropriate team member. After patient contact, the ancillary provider then follows up with the PCP to obtain care plan approval. The care manager should also be involved in each step to facilitate team coordination of care.
Determination of patient severity
Determination of problem severity is the cornerstone of effective team-based stepped care. Severity should be assigned based on both screening results, the type of patient visit, care at other sites, and data from potential previous encounter(s).Patients are labeled as low, moderate, or high severity by the care manager (see Table 2 for examples of severity classifi-cations and Figure 1 for care pathways associated with each level of severity). The level of severity determines the type and number of providers involved on the patient care team and in the clinic visit.
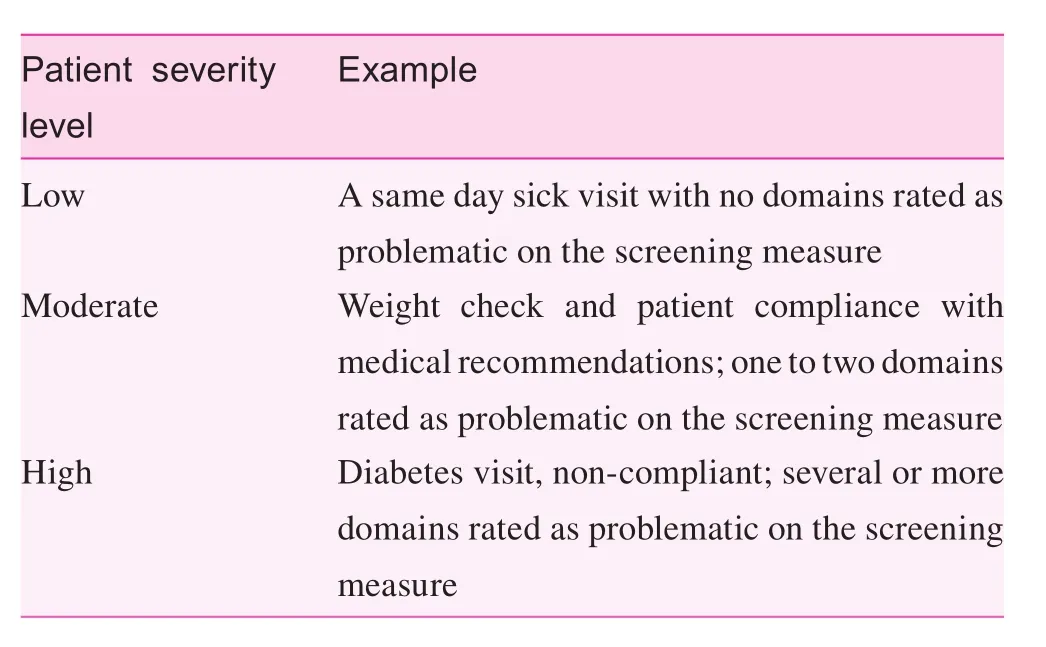
Table 2. Patient severity categories
Importance of the electronic health record
Proper use of an electronic health record (EHR) is crucial for effective implementation of team-based stepped care. All members of the care team, and particularly the care manager,must be able to review all patient data in order to coordinate care. Furthermore, team members must be trained in effective EHR communication. Modes of communication differ with each program and consensus must be reached on best practices. EHR use is not a perfect proxy for verbal consultation;however, these programs uphold team-based practice.
An example of team-based stepped care
Consider the case of an adult patient presenting to a primary care clinic with type 2 diabetes mellitus. The patient was known to have poor control of blood glucose based on information from a prior encounter and records from a recent emergency department visit. The patient did not exhibit psychological impairment on screening measures during the encounter in question, but reported low mood not accompanied by additional symptoms of clinical depression. First, the care manager would assign this patient to the "high" severity category due to the patient's poor blood glucose control, recent ED visit,and mood symptoms. Ideally, this severity rating would be assigned a week in advance of the present encounter to allow time for the patient to be staffed during the team meeting.
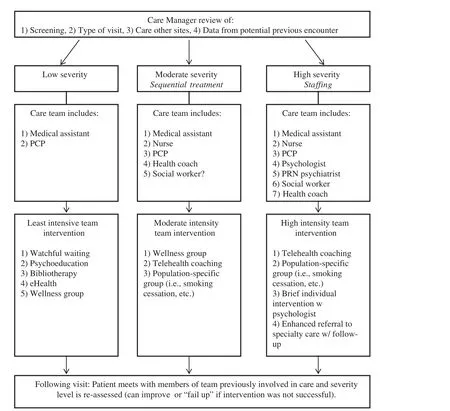
Figure 1. Team-based integrated care pathways based on patient severity.
An example of stepped care intervention, as determined at the staffing meeting, might include the following: 1) increasing health literacy (educating the patient regarding proper diabetes management, what symptoms are indicative of increased intervention, and how low mood is maintained/alleviated; Health Coach); 2) motivational interviewing techniques to enhance motivation for change (BHC); 3) idiographic prevention (i.e.,support of healthy coping strategies and discouragement of use of avoidance coping; BHC); 4) primary care encounter consistent with TAU; PCP; 5) nutritional counseling (dietician); 6)strengthening of the provider/patient relationship (specifically,informing the patient that should her symptoms worsen that the provider will be available to provide consultation and care;all team members); 7) telehealth coaching to increase adherence to the diabetes management regimen (health coach); and 8) provision of a printed integrated care plan (front desk staff).The team must also determine the order of services received by the patient. In the event that the patient's symptoms of low mood do not remit, a brief evidence-based cognitive behavioral intervention would be implemented in the primary care setting. If the patient's symptoms do not remit following a brief intervention, referral to a BHC or other health care provider would be appropriate.
Progress towards treatment targets should be continually assessed during encounters with team members and patient severity may be reassigned by the care manager. For example, in the case of a patient in whom the low mood remitted,services targeting this problem would be eliminated and the patient may move to a moderate severity category.
Importance of quality improvement
Quality improvement (QI) in health care is an important method of assessing and improving health outcomes, as emphasized in the seminal report, Crossing the Quality Chasm[1]. Team-based stepped care functions as a system, with many processes involved in the delivery of care, and QI provides the ideal method of assessing quality.
To utilize QI, measurable processes and outcomes must first be identified. For example, if a practice is interested in assessing patient satisfaction as an outcome, processes in the system that may influence that outcome must be identified.This may include assessing variables such as wait times in the clinic, time between scheduling an appointment and seeing a provider, and time between calling a provider and getting to speak with the provider. By collecting data on these variables,administrators may find that there may be one or multiple variables that may be addressed to improve overall patient satisfaction with services.
Another aspect of QI is the assumption that problems with performance or sub-optimal care are a product of the system and not the individuals working within the system, which may be particularly important with a team-based approach in that it does not make assertions or try to weed out the "bad apple."Therefore, changes at a system level would allow a plethora of individuals to operate effectively within that system rather than trying to find an individual that can perform well despite problems in the system. This approach to gaps in care may also improve staff morale, and reduce the cost of turnover and the need to train individuals in a team-based approach. Use of QI in all team-based stepped care is imperative due to the fact that evaluation of this approach remains in its infancy.
Conclusions
Team-based stepped care is a framework from which all IC should be implemented. This approach facilitates collaboration between care teams by providing a common perspective for providers to work from that is consistent with the medical model. The ability of stepped care to appropriately scale treatment to patient severity also aids in population management and medical cost offset. Through the use of QI initiatives and continued empirical evaluation, team-based stepped care can support IC in fulfilling the creation of meaningful health care reform.
Conflict of interest
The authors declare no conflict of interest.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
1. Institute of Medicine (US). Committee on Quality of Health Care in America. Crossing the quality chasm: A new health system for the 21st century. National Academy Press; 2001.
2. McGuire TG, Miranda J. New evidence regarding racial and ethnic disparities in mental health: policy implications. Health Affair 2008;27:393–403.
3. World Health Organization. Integrating Mental Health into Primary Care: A Global Perspective. Geneva, Switzerland: WHO Press; 2008.
4. Kazdin AE, Blase SL. Rebooting psychotherapy research and practice to reduce the burden of mental illness. Perspect Psychol Sci 2011;6:21–37.
5. National Institute of Mental Health. Mental illness exacts a heavy toll, beginning in youth. Available from: www.nimh.nih.gov/news/science-news/2005/mental-illness-exacts-heavy- tollbeginning-in-youth.shtml; 2005.
6. Cummings NA, O'Donohue WT, Ferguson KE. The impact of medical cost offset on practice and research: Making it work for you: A report of the first reno conference on medical cost offset.Reno, Nevada: Context Press; 2002.
7. O'Donohue WT, Cummings NA, Cucciare MA, Runyan CN,Cummings JL. Integrated behavioral health care: A guide to effective intervention. Amherst, NY: Humanity Books; 2006.
8. Cummings NA, O'Donohue WT. Where we are, how we got there, and where we need to go: The promise of integrated care.Understanding the behavioral healthcare crisis: The promise of integrated care and diagnostic reform, 1–18, 2011.
9. Sheldrick RC, Merchant S, Perrin EC. Identification of developmental-behavioral problems in primary care: a systematic review. Pediatrics 2011;128:356–63.
10. Laygo R, Chaffe B, O'Donohue W. Integrating Behavioral Health Into Primary Care in Military Treatment Facilities: Report on A Successful Quality Improvement Project. In O'Donohue, W.T. & Maragakis, A. (Eds.) Quality Improvement and Behavioral Health. New York: Springer Publishing Company (in press).
11. O'Donohue WT, Draper C. The case for evidence-based stepped care as part of a reformed delivery system. In Stepped Care and e-Health. New York: Springer; 2011. pp. 1–16.
12. O'Donohue W, Snipes C, Maragakis A. Increasing the productivity of the clinical psychologist: A neglected Archimedean pivot?Prof Psychol: Res Pract 2014;45:357.
13. Von Korff M, Glasgow RE, Sharpe M. ABC of psychological medicine: Organising care for chronic illness. BMJ: Brit Med J 2002;325:92.
14. Zeiss AM, Karlin BE. Integrating mental health and primary care services in the Department of Veterans Affairs health care system. J Clin Psychol Med Sett 2008;15:73–8.
15. Health Catalyst. Population health management solutions. Available from: www.healthcatalyst.com/population-health/; 2015.Accessed 5 February 2015.
16. Chiles JA, Lambert MJ, Hatch AL. The impact of psychological interventions on medical cost offset: A meta-analytic review. Clin Psychol: Sci Pr 1999;6:204–20.
17. California Mental Health Service Authority. Why pursue integrated behavioral health care? Available from: http://ibhp.org/index.php?section=pages&cid=104; 2015.
18. Muntingh AD, Feltz-Cornelis CM, van Marwijk HW, Spinhoven P, Assendelft WJ, de Waal MW, et al. Collaborative stepped care for anxiety disorders in primary care: Aims and design of a randomized controlled trial. BMC Health Serv Res 2009;9:159.
19. Lin EH, VonKorff M, Russo J, Katon W, Simon GE, Unutzer J,et al. Can depression treatment in primary care reduce disability?:A stepped care approach. Arch Family Med 2000;9:1052.
20. Katon W, Von Korff M, Lin E, Simon G, Walker E, Unützer J,et al. Stepped collaborative care for primary care patients with persistent symptoms of depression: a randomized trial. Arch Gen Psychiat 1999;56:1109–15.
21. Hedrick SC, Chaney EF, Felker B, Liu CF, Hasenberg N,Heagerty P, et al. Effectiveness of collaborative care depression treatment in Veterans' Affairs primary care. J Gen Intern Med 2003;18:9–16.
22. Zatzick D, Rivara F, Jurkovich G, Russo J, Trusz SG, Wang J,et al. Enhancing the population impact of collaborative care interventions: Mixed method development and implementation of stepped care targeting posttraumatic stress disorder and related comorbidities after acute trauma. Gen Hosp Psychiat 2011;33:123–34.
Cassandra Snipes Department of Psychology, University of Nevada, Reno, 1664 N.Virginia Street, Mail Stop 298,Reno, NV, USA 89557
E-mail: snipes.cassandra@gmail.com
3 March 2015;
Accepted 10 March 2015
杂志排行
Family Medicine and Community Health的其它文章
- Effectiveness of an employment-based smoking cessation assistance program in China
- The Accountable Care Organization results: Population health management and quality improvement programs associated with increased quality of care and decreased utilization and cost of care
- "Three essential elements" of the primary health care system:A comparison between California in the US and Guangdong in China
- Menopause and the risk of metabolic syndrome among middle-aged Chinese women
- Availability and social determinants of community health management service for patients with chronic diseases:An empirical analysis on elderly hypertensive and diabetic patients in an eastern metropolis of China
- Evaluating the process of mental health and primary care integration:The Vermont Integration Profile