典型与非典型症状非糜烂性反流病患者食管动力学特征研究
2015-06-28林玲冉亚梅郎秀琼何雨芩陈强纪雷杨敏
林玲,冉亚梅,郎秀琼,何雨芩,陈强,纪雷,杨敏
典型与非典型症状非糜烂性反流病患者食管动力学特征研究
林玲,冉亚梅,郎秀琼,何雨芩,陈强,纪雷,杨敏
目的探讨典型与非典型症状非糜烂性反流病(NERD)患者的食管动力学特征。方法选取2012年8月-2014年12月于第三军医大学大坪医院消化科就诊的NERD患者86例,分别行上消化道内镜及高分辨率食管测压检查。纳入内镜检查未见食管黏膜破损和Barret食管等的患者。按照有无典型反酸烧心症状分为典型症状组(n=47)和非典型症状组(n=39),采用高分辨率食管测压仪检查评估不同症状NERD患者食管动力的差异及临床意义。结果典型症状组食管下段括约肌(LES)静息压及残余压分别为15.79±1.21和5.80±1.16mmHg,明显低于非典型症状组(分别为20.68±1.64和10.42±1.20mmHg,P<0.01)。典型症状组和非典型症状组在食管体部蠕动功能、LES总长度、LES腹内段长度及食管上段括约肌(UES)静息压及残余压方面差异均无统计学意义(P>0.05)。结论典型与非典型症状的NERD患者食管动力特征存在差异,区别主要在于前者LES静息压和残余压降低。
胃食管反流;食管括约肌,下段;动力学
非糜烂性反流病(non-erosive reflux disease,NERD)是指存在反流相关的不适症状,但内镜下未见食管黏膜损害的疾病,是临床上最常见的胃食管反流病[1],约占胃食管反流病(GERD)的50%~70%。典型反流综合征可以在不用诊断性试验的情况下通过特征性临床症状来诊断。有文献报道,与糜烂性食管炎相比,NERD患者很少存在食管动力障碍,常表现为食管下段括约肌(LES)静息压正常或略有降低,极少会低于10mmHg,且NERD患者仅存在轻微的食管动力异常[2-3]。然而既往研究多将NERD作为一个整体来进行研究分析,而未进一步区分不同亚型NERD患者食管动力的差异。本研究比较典型与非典型症状NERD患者食管压力的检查结果,以全面了解典型与非典型症状NERD患者的食管动力学特征,以及食管动力改变在不同症状NERD患者发病机制中的可能作用。
1 资料与方法
1.1 研究对象 2012年8月-2014年12月在第三军医大学大坪医院消化内科就诊的86例具有典型反流烧心、胸骨后不适等食管及食管外相关症状的NERD患者,所有患者均接受上消化道内镜检查及高分辨率食管测压检查。入选标准:(1)典型症状NERD组:最近3个月内有典型的反酸烧心症状,RDQ量表反酸烧心等症状评分>12分;(2)非典型症状NERD组:存在有非典型的胃食管反流症状,主要表现为反流性喉炎、反流性咳嗽、反流性哮喘、咽部不适、胸闷、声嘶、嗳气、咽部异物感、胸骨后疼痛等,亦可伴有上消化道不适(包括呕吐、嗳气、上腹不适、恶心等)[4-5];(3)内镜阴性,即食管下无黏膜破损无Barrett食管等;(4)近4周内未服用H2受体拮抗剂类药物和/或PPI;(5)既往无消化系统病史,无消化道手术史,无可引起胃食管反流症状的严重心肺疾病或其他全身性疾病。排除标准:不能耐受食管测压及胃镜检查者,年龄<18岁,孕妇及哺乳期妇女;内镜检查发现Barrett食管,食管良恶性肿瘤患者,食管静脉曲张者,严重食管动力障碍性疾病如贲门失迟缓征,食管裂孔疝及食管息肉等;曾行胃及食管手术者,糖尿病患者,酗酒者,结缔组织病及凝血机制障碍者等可能影响胃肠道运动功能的疾病。本研究经第三军医大学大坪医院伦理委员会批准,所有参加者对研究方案均知情同意。
1.2 方法
1.2.1 上消化道内镜检查 所有患者检查前均禁食禁饮8h以上以防止呕吐和误吸,使用奥林巴斯(Olympus)电子胃镜检查。患者采取侧卧位,经手背静脉全麻后再经口腔将电子内镜缓慢插入食管及胃十二指肠中,在电镜直视下观察有无食管粘膜损害、Barret食管及其他需纳入排除标准的胃食管改变。
1.2.2 高分辨率食管测压 测压采用美国Sierra Scientific Instruments(SSI)公司的36通道固态高分辨率传感器测压系统(型号ENA1068)通道间距1cm,导管外径4.2mm。所有患者检查前均禁食禁饮8h防止呕吐和误吸,检查前1d禁烟酒、咖啡及胃肠动力药。检查在安静、适温的检查室中进行。调试好测压设备,受试者取坐位,经鼻插入测压导管。当部分咽部、全段食管和部分胃内压力均能同时显示且保证至少2个测压通道位于胃内后,将导管用医用胶带固定于鼻翼处。嘱患者适应5min,若患者出现明显恶心、呕吐、误吸等症状不能耐受检查时则停止检查,若无明显不适后再取侧卧位。连接导管和传感器,待压力数值稳定后开始测压记录。记录过程中,除需吞咽外,受试者不可做吞咽动作,且每次只允许吞咽一次,一旦在一次吞咽记录期间出现连续2次或2次以上吞咽、咳嗽或者打嗝等,该次吞咽将被剔除并且重新开始新的吞咽。嘱受试者停止吞咽30s以记录食管各段基础压力水平,然后再给予10次湿咽,每次咽生理盐水5ml,2次吞咽间隔30s,对于配合能力差的受试者,每次吞咽间距至少达20s,待所有程序完成后拔出测压导管,检查结果基于已发表的芝加哥分类[6]。
1.3 统计学处理 采用SPSS18.0 软件,计量资料采用表示,计量资料的比较采用t检验,计数资料的比较采用χ2检验。以P<0.05为差异有统计学意义。
2 结 果
2.1 一般情况 根据以上纳入排除标准共入选86例患者,其中典型症状组47例,非典型症状组39例。两组性别及身高差异无统计学意义(P>0.05);典型症状组年龄(48.4±1.9岁)大于非典型症状组(41.7±1.6岁,P<0.05)。
2.2 食管括约肌情况比较 典型症状组食管下段括约肌(LES)静息压及残余压均较非典型症状组明显降低,差异有统计学意义(P<0.05或P<0.01);而两组之间LES总长度、腹内段长度,以及食管上段括约肌(UES)静息压及残余压差异无统计学意义(P>0.05,表1)。
2.3 食管体部蠕动功能比较 典型症状组与非典症状组在食管蠕动速度≤6.25cm/s的百分比、同步收缩速度≥6.25cm/s的百分比、蠕动波起始速度(cm/s)、食管无效吞咽百分比(LES以上3~11cm),波幅平均值(mmHg)、平均波持续时间平均值(s)(LES以上3~7cm)等方面差异均无统计学意义(P>0.05,表2)。
3 讨 论
随着医疗诊断水平的提高以及人们生活水平的进步,更多的技术被用于医疗诊断。高分辨率食管测压技术可以清楚地显示从咽部到食管的运动情况。该技术虽然不能直接反映胃食管反流病,但可以评估NERD患者是否存在抗反流机制障碍,如LES大小、LES长度及食管体部运动功能等。GERD是一种常见病,在世界各地的发病率不同。烧心和反流是其特征性症状,在GERD患者中,烧心和反流的发生率分别为75%~98%和48%~91%。GERD是一种多因素导致的慢性疾病[7-8],其主要发病机制为食管侵袭性因素的增强及防御功能的减弱。侵袭性因素包括胃酸、胆汁胆盐等反流入食管及茶、非甾体抗炎药、咖啡等某些刺激性伤害性药物异物等对食管黏膜的急慢性损伤[9]。而LESP降低及其功能障碍[8]及食管体部运动功能异常是食管防御功能减弱的主要表现,与NERD发病密切相关[10]。LES是食管-胃连接处一段约3~5cm长度的高压带,其压力在10~35mmHg,有效地阻止了胃内容物的反流。LES和膈角被认为是食管下端的内括约肌和外括约肌,为食管主要的抗反流屏障,LESP的高低为食管屏障功能高低的表现之一。正常人腹腔内压升高时通过神经反射调节,LESP也显著增加来加强抗反流屏障。另外,当LES压力降低也增加了一过性反流的概率。大量临床实践表明:高分辨率食管测压是诊断食管良性疾病,特别是食管功能障碍性相关疾病的重要手段。不同症状的NERD患者临床抗酸治疗效果不同,可能是其发病机制不同所致。
表1 两组LES及UES情况比较(mmHg,±s)Tab.1 Features of LES and UES in both TSP and ASP group (mmHg,±s)
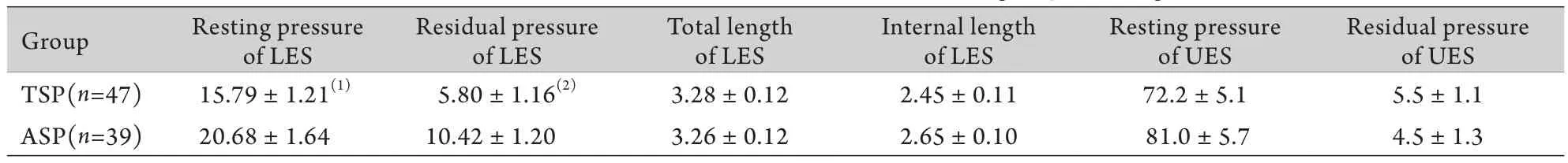
表1 两组LES及UES情况比较(mmHg,±s)Tab.1 Features of LES and UES in both TSP and ASP group (mmHg,±s)
TSP. Typical symptom group; ASP. Atypical symptom group; LES. Lower esophageal sphincter; UES. Upper esophageal sphincter; (1)P<0.05,(2)P<0.01 compared with ASP
Residual pressure of UES TSP(n=47) 15.79±1.21(1) 5.80±1.16(2) 3.28±0.12 2.45±0.11 72.2±5.1 5.5±1.1 ASP(n=39) 20.68±1.64 10.42±1.20 3.26±0.12 2.65±0.10 81.0±5.7 4.5±1.3 Group Resting pressure of LES Residual pressure of LES Total length of LES Internal length of LES Resting pressure of UES
表2 食管体部蠕动功能(±s)Tab.2 The peristalsis function of esophageal body (±s)
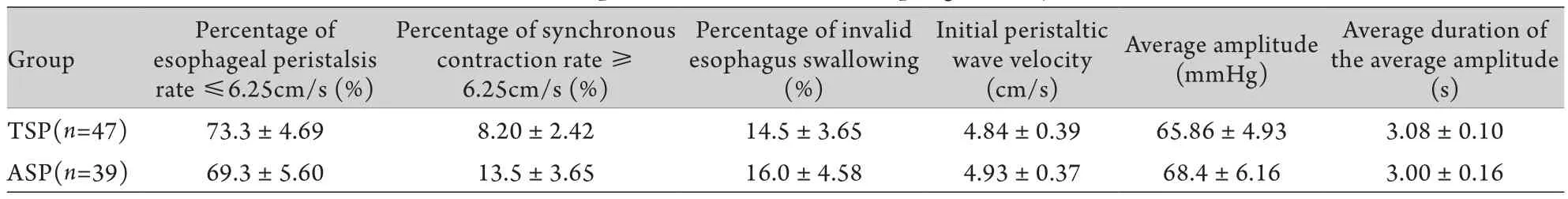
表2 食管体部蠕动功能(±s)Tab.2 The peristalsis function of esophageal body (±s)
TSP. Typical symptom group; ASP. Atypical symptom group
Average duration of the average amplitude (s) TSP(n=47) 73.3±4.69 8.20±2.42 14.5±3.65 4.84±0.39 65.86±4.93 3.08±0.10 ASP(n=39) 69.3±5.60 13.5±3.65 16.0±4.58 4.93±0.37 68.4±6.16 3.00±0.16 Group Percentage of esophageal peristalsis rate ≤6.25cm/s (%) Percentage of synchronous contraction rate ≥6.25cm/s (%) Percentage of invalid esophagus swallowing (%) Initial peristaltic wave velocity (cm/s) Average amplitude (mmHg)
据文献报道,与正常对照组相比较,NERD患者LES松弛率较高且LESP明显降低[11];糜烂性食管炎患者与NERD患者在LESP、LES的长度、食管收缩振幅及远端收缩积分等方面均无明显差异[12];有反流烧心典型症状的患者LESP降低比无反酸烧心的患者更加明显[13]。本研究表明,不同症状的NERD患者,即典型症状和非典症状的NERD 患者的LES静息压及残余压具有明显统计学差异,且典型症状组的LES静息压及残余压较非典型组明显降低,而在食管体部蠕动力方面两者无明显统计学差异。由此我们推测:不同症状的NERD患者食管动力特征差异的主要区别可能在于LESP的改变。对于不同症状的NERD患者,典型症状组的反流烧心症状非常明显的原因可能在于典型症状组LESP降低明显及LES长度缩短及功能障碍等[14]。当LES压力降低,破坏了抗反流屏障的重要组成部分,胃内容物更容易反流入食管[15],且当LES静息压降低或一过性松弛时[8],胃内压升高,胃动力降低使胃排空延缓,腹内压增高等造成抗反流屏障功能相对降低,食管体部有效收缩功能及蠕动波的传导速度减慢造成食管算清除能力下降等因素相互作用[16-17],引起胃酸、胆汁胆盐等胃十二指肠内物反流入食管或长期停留在食管内,刺激食管黏膜而出现反酸、烧心、胸骨后不适等症状[18]。LESP降低时将增加食管中酸暴露的概率,而食管中酸暴露增加又会反馈性引起LES一过性的松弛[19]。同时有研究表明[18],食管酸敏感性增高可能导致食管黏膜损害并出现烧心的主要原因。以上因素相互影响相互作用可能是不同症状NERD患者出现不同表现的主要原因。
本研究还发现,典型症状组与非典型症状组的NERD患者在年龄上存在统计学差异,且典型症状组的NERD患者发病年龄较大。有研究表明,年龄大于65岁的人群中上消化道疾病的发生率明显升高[20],老年人群中NERD的发病率及疾病严重程度均高于年轻人群。同时有研究认为,55岁以后GERD的发病率有明显升高[21]。也有研究证实,随年龄增长,食管的蠕动波传导速度逐渐下降,无效的食管蠕动增加,可能进一步导致食管清除障碍,推进NERD的发生及加重其严重程度[14,22]。年龄对NERD的影响是复杂的,其机制可能与老年人LES长度缩短及其压力降低、食管运动功能减弱、胃排空能力减弱、唾液分泌减少、胆盐及药物等侵袭因素增加有关,其具体机制尚不清楚还需进一步研究。
综上所述,不同症状NERD患者的食管动力学特征存在差异,其差别在于LESP的改变以及年龄对NERD临床症状的影响。本研究未对年龄对NERD的影响进行更深入的研究,尚存在不足。但本研究对NERD患者从症状学上进行了亚分组,初步了解了不同症状NERD患者食管动力学特征。由此我们建议,对具有典型症状的NERD患者,可在常规抗酸保护黏膜等治疗的同时加用增加LESP的药物[23],采用电刺激疗法[24]或手术等方法,以共同作用来减轻或消除NERD症状。
[1]Ran YM,Lin L,He YQ,et al. Therapeutic efficacy of digital music gastric electrical pacing for refractory functional dyspepsia concomitant with non-erosive reflux disease[J]. Med J Chin PLA,2015,40(3): 212-216. [冉亚梅,林玲,何雨芩,等. 数字化音乐胃电起搏治疗顽固性功能性消化不良重叠非糜烂性反流病的疗效观察[J]. 解放军医学杂志,2015,40(3): 212-216.]
[2]Fass R. Erosive esophagitis and nonerosive reflux disease (NERD): comparison of epidemiologic,physiologic,and therapeutic characteristics[J]. J Clin Gastroenterol,2007,41(2): 131-137.
[3]Hershcovici T,Fass R. Nonerosive reflux disease (NERD)-an update[J]. J Neurogastroenterol Motil,2010,16(1): 8-21.
[4]Hom C,Vaezi MF. Extra-esophageal manifestations of gastroesophageal reflux disease: diagnosis and treatment[J]. Drugs,2013,73(12): 1281-1295.
[5]Powitzky ES,Khaitan L,Garrett CG,et al. Symptoms,quality of life,video laryngoscopy,and twenty-four-hour triple-probe pH monitoring in patients with typical and extra-esophageal reflux[J]. Ann Otol Rhinol Laryngol,2003,112(10): 859-865.
[6]Bredenoord AJ,Fox M,Kahrilas PJ,et al. Chicago classification criteria of esophageal motility disorders defined in high resolution esophageal pressure topography[J]. Neurogastroenterol Motil,2012,24(suppl 1): 57-65.
[7]Moayyedi P,Talley NJ. Gastrooesophageal reflux disease[J]. Lancet,2006,367(9528): 2086-2100.
[8]Boeckxstaens G,El-Serag HB,Smout AJ,et al. Symptomatic reflux disease: the present,the past and the future[J]. Gut,2014,63: 1185-1193.
[9]Vossoughinia H,Salari M,Mokhtari Amirmajdi E,et al. An epidemiological study of gastroesophageal reflux disease and related risk factors in urban population of mashhad,iran[J]. Iran Red Crescent Med J,2014,16(12): e15832.
[10] Ho SC,Chang CS,Wu CY,et al. Ineffective esophageal motility is a primary motility disorder in gastroesophageal reflux disease[J]. Dig Dis Sci,2002,47(3): 652-656.
[11] Ribolsi M,Holloway RH,Emerenziani S,et al. Impedance-high resolution manometry analysis of patients with nonerosive reflux disease[J]. Clin Gastroenterol Hepatol,2014,12(1): 52-57.
[12] Yi ZH,Feng L,Wen MY,et al. Association between acid reflux and esophageal dysmotility in patients with gastroesophageal reflux disease[J]. Sichuan Da Xue Xue Bao Yi Xue Ban,2014,45(3): 480-483.
[13] Wang K,Duan L,Xia Z,et al. Esophageal motility characteristics of refractory heartburn: a study based on high resolution manometry and 24 hour pH-impedance monitoring[J] Zhonghua Yi Xue Za Zhi,2014,94(34): 2650-2655.
[14] Corsi PR,Gagliardi D,Horn M,et al. Factors related to the presence of reflux in patients with typical symptoms of gastroesophageal reflux disease (GERD ) [J]. Rev Assoc Med Bras,2007,53(2): 152-157.
[15] Curcic J,Roy S,Schwizer A,et al. Abnormal structure and function of the esophagogastric junction and proximal stomach in gastroesophageal reflux disease[J]. Am J Gastroenterol,2014,109(5): 658-667.
[16] Wang K,Duan L,Xia Z,et al. Esophageal motility characteristics of refractory heartburn: a study based on high resolution manometry and 24 hour pH-impedance monitoring[J]. Zhonghua Yi Xue Za Zhi,2014,94(34): 2650-2655.
[17] Ergün M,Doğan İ,Ünal S. Ineffective esophageal motility and gastroesophageal reflux disease: a close relationship[J]? Turk J Gastroenterol,2012,23(6): 627-633.
[18] Ru F,Banovcin P Jr,Kollarik M. Acid sensitivity of the spinal dorsal root ganglia C-fiber nociceptors innervating the guinea pig esophagus[J]. Neurogastroenterol Motil,2015,27(6): 865-874.
[19] Banovcin P Jr,Halicka J,Halickova M,et al. Studies on the regulation of transient lower esophageal sphincter relaxations (TLESRs) by acid in the esophagus and stomach[J]. Dis Esophagus,2015 doi: 10.1111/dote.12357. [Epub ahead of print]
[20] Pilotto A. Aging and upper gastrointestinal disorders[J]. Best Pract Res Clin Gastroenierol,2004,18(suppl): 73-81.
[21] Dent J,El-Serag HB,Wallander MA,et al. Epidemiology of gastro-oesophageal reflux disease: a systematic review[J]. Gut,2005,54(4): 710-717.
[22] Besanko LK,Burgstad CM,Cock C,et al. Changes in esophageal and lower esophageal sphincter motility with healthy aging[J]. J Gastrointestin Liver Dis,2014,23(3): 243-248.
[23] Kempf J,Lewis F,Reusch CE,et al. High-resolution manometric evaluation of the effects of cisapride and metoclopramide hydrochloride administered orally on lower esophageal sphincter pressure in awake dogs[J]. Am J Vet Res,2014,75(4): 361-366.
[24] Ciotola F,Ditaranto A,Bilder C,et al. Electrical stimulation to increase lower esophageal sphincter pressure after POEM[J]. Surg Endosc,2015,29(1): 230-235.
The differences in esophageal motility and its clinical significance between the patients with typical and atypical symptoms of non-erosive reflux disease
LIN ling,RAN Ya-mei,LANG Xiu-qiong,HE Yu-qin,CHEN Qiang,JI Lei,YANG Min*
Department of Gastroenterology,Daping Hospital,Third Military Medical University,Chongqing 400042,China
*< class="emphasis_italic">Corresponding author,Email: yangmindoctor@126.com
,Email: yangmindoctor@126.com
This work was supported by the key project of Natural Science Foundation of Changqing (cstc2013jjB0143)
ObjectiveTo study the characteristics of esophageal motility in the patients with different symptoms of nonerosive reflux disease (non-erosive reflux disease,NERD).MethodsEighty-six patients with NERD who visited the Department of Gastroenterology in our hospital from August 2012 to December 2014 were selected. They were all evaluated with upper gastrointestinal endoscopy and high resolution esophageal manometry. Those who had neither definite esophageal mucosal erosion nor Barrett's esophagus at endoscopy were diagnosed as NERD. According to the presence or absence of typical acid reflux and/or heartburn symptoms,patients with NERD were divided into two groups: the typical symptom group (47 cases),and the atypical symptom group (39 cases). High resolution measurement of esophageal pressure was used to evaluate the differences in esophageal dynamic characteristics between patients with different symptoms of NERD. The final results were analyzed withttest and chi-square test.ResultsCompared with atypical symptom group,both the resting pressure (20.68±1.64mmHgvs15.79±1.21mmHg respectively,P<0.05) and residual pressure (10.42±1.20mmHgvs5.80±1.16mmHg respectively,P<0.01) of lower esophageal sphincter (LES) in typical symptoms group were obviously lower and the differences were statistically significant. However,the esophageal peristalsis function,the total length of LES,the intra-abdominal length of LES,the resting pressure and residual pressure of upper esophageal sphincter (UES) showed no obvious difference between two groups (P>0.05).ConclusionThere is a difference in esophageal motility characteristics between the patients with typical and atypical symptoms of NERD,and the main differences are changes in the resting pressure and residual pressure of LES.
gastroesophageal reflux; esophageal sphincter,lower; kinetics
R573.9
A
0577-7402(2015)12-0999-04
10.11855/j.issn.0577-7402.2015.12.12
2015-06-25;
2015-08-12)
(责任编辑:熊晓然)
重庆市自然科学基金(重点)项目(cstc2013jjB0143)
林玲,硕士研究生。主要从事胃肠动力学的临床与基础研究
400042 重庆 第三军医大学大坪医院消化内科(林玲、冉亚梅、郎秀琼、何雨芩、陈强、纪雷、杨敏)
杨敏,E-mail:yangmindoctor@126.com