颈椎后纵韧带钙化前路手术并发脑脊液漏的处理策略
2015-06-23菅凤增
吴 浩,齐 猛,菅凤增
(首都医科大学宣武医院,北京 100053)
颈椎后纵韧带钙化前路手术并发脑脊液漏的处理策略
吴 浩,齐 猛,菅凤增
(首都医科大学宣武医院,北京 100053)
目的 探讨前路手术治疗颈椎后纵韧带钙化(ossification of the posterior longitudinal ligament,OPLL)时脑脊液(cerebrospinal fluid,CSF)漏的处理方法。方法 2010年8月至2014年12月期间治疗的颈椎OPLL患者124例,其中75例行前路椎体次全切,49例行椎体次全切+单间隙间盘摘除术。分析发生CSF漏的处理方式及预后,总结前路手术并发CSF漏的处理策略。结果 124例患者术中硬脊膜破损发生率为 5.6%(7/124),CSF漏的发生率为3.2%(4/124)。硬脊膜破损但蛛网膜保持完整的患者未作任何特殊处理,患者预后良好,未出现明确CSF漏;CSF漏的患者术中使用脂肪或人工硬膜配合纤维蛋白胶修补,术后均腰池引流4~5天,最终预后良好,无一例CSF漏患者并发脑膜炎、皮肤窦道等二次并发症。结论 前路手术治疗颈椎OPLL出现CSF漏的处理方式包括预防措施、术中硬脊膜修补(使用不同材料)、术后腰池引流,甚至脑室引流或脑室腹腔分流。术中硬脊膜直接缝合修补是最佳的处理方式,但是由于在技术操作困难,大部分情况是不能实施的。术中进行一定的修补措施,同时术后进行辅助手段,可以达到良好效果。
颈椎后纵韧带骨化;前路手术;脑脊液漏
颈椎后纵韧带钙化(ossification of the posterior longitudinal ligament,OPLL)是颈椎管狭窄的主要原因之一,可导致脊髓型颈椎病及神经根型颈椎病。颈椎OPLL的治疗有多种手术方式,包括颈前路椎体次全切、后路单开门椎管扩大成形术、后路椎板切除+固定融合术、前后联合入路等[1]。对于连续型、多个节段(>3个)的颈椎OPLL的治疗往往采用后路单开门手术或后路椎板切除+内固定融合手术,进行间接减压。对于局限性的OPLL,相对于后路手术,前路椎体次全切去除钙化后纵韧带并固定融合,对脊髓能够达到直接的更为充分的减压效果,同时由于齿状韧带的作用,使神经根袖套更为贴近椎管腹侧,因此对于神经根型颈椎病,前路手术对于神经根的减压疗效远好于后路手术[2,3]。但是许多颈椎OPLL的病例中,腹侧硬脊膜往往与钙化的后纵韧带粘连紧密,有时甚至硬脊膜本身出现钙化[2]。因此术中去除钙化的后纵韧带时,极易造成硬脊膜撕裂、破损,导致CSF漏,有时甚至会导致脊髓或神经根的损伤,所以前路手术导致CSF漏风险远高于后路手术[4~6]。因此在选择前路手术方式时,术者必须考虑到CSF漏的风险,并在术前评估、术中操作、术后处理等多方面应对CSF漏[7~9]。
1 资料与方法
1.1 一般资料 2010年8月至2014年12月首都医科大学宣武医院神经外科收治的颈椎OPLL患者124例。其中男68例,女56例;年龄18~73岁;75例行前路椎体次全切,49例行椎体次全切+单间隙间盘摘除术。
1.2 方法 分析颈椎OPLL患者术中及术后发生CSF漏的处理方式及预后,总结前路手术并发CSF漏的处理策略。
2 结果
术中硬脊膜破损发生率为 5.6%(7/124),CSF漏发生率为3.2%(4/124)。7例硬脊膜破损患者中,宽基OPLL 2例,大于2节段OPLL的2例;硬脊膜破损、蛛网膜保持完整、无CSF流出3例,均采用自体脂肪结合纤维蛋白胶封堵;硬脊膜破损较小、合并CSF流出者采用自体脂肪结合纤维蛋白胶封堵;硬脊膜破损较大、合并CSF流出者采用术中显微镜下直接缝合修补。术中发生硬膜囊撕破、有CSF流出的患者,均留置术区硬膜外引流;硬脊膜破损、蛛网膜保持完整的患者未用术区硬膜外引流。CSF漏的患者均行腰池引流4~5天,其中1例在拔出腰池引流第2天后再次出现术区肿胀,予以二次腰池引流,保持10天后拔出,最终预后良好。随访显示CSF漏患者最终预后均良好,未出现感染、脑膜炎、皮肤窦道等二次并发症。
3 讨论
对于颈椎病的治疗,前路手术(椎间盘摘除、椎体次全切)作为一种直接有效的减压方式被广泛运用。颈椎前路手术出现硬脊膜破损,导致CSF漏的概率为0.5%~3%[10~13]。其中,OPLL手术出现CSF漏的概率更高,为4.3%~32%[5,13~19]。Hannallah等研究发现OPLL是CSF漏的主要原因,合并有OPLL的患者,经颈前手术减压出现CSF漏的概率是无OPLL患者的13.7倍[11]。CSF漏可以继发多种二次并发症,包括脑膜炎、伤口延期愈合、气道阻塞、皮肤窦道、假性脑膜膨出等。早期有效地处理CSF漏,可防止二次并发症[12,17~22]。CSF处理有多种方式,包括术中直接缝合修补、使用凝胶海绵、脂肪、人工硬膜等材料,配合纤维蛋白胶进行修补,术后伤口硬膜外引流、腰池引流或腰穿、术区CSF腔隙-腹腔分流、脑室外引流以及脑室腹腔分流等[22~24]。更为重要的是术前对于发生CSF漏的可能性进行评估。术前影像学的表现极为重要,往往通过颈椎CT可发现钙化的硬脊膜[2](图1)。对于多个节段或基底较宽的后纵韧带钙化(图2),术中发生CSF漏可能性极大。
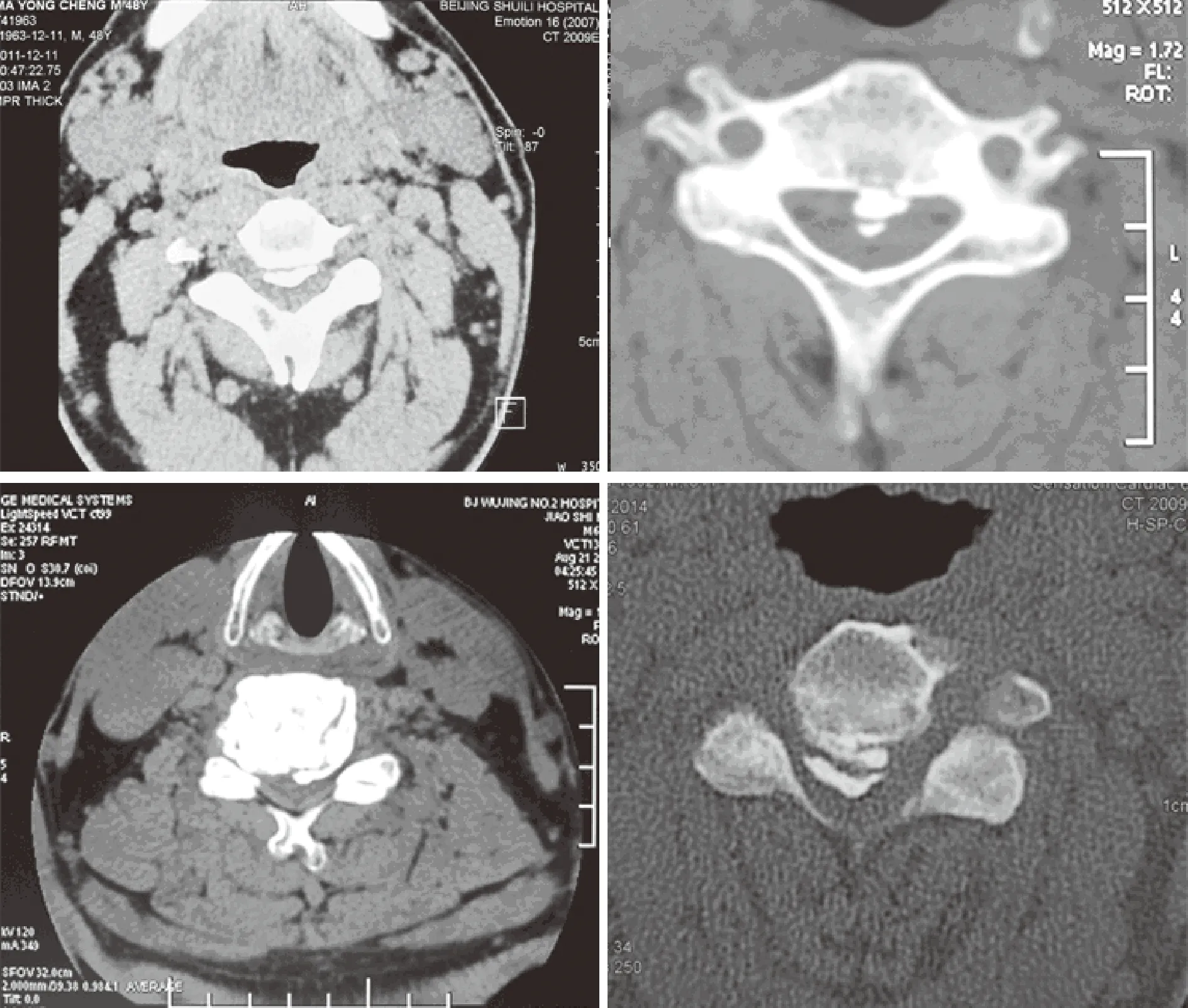
图1 颈部轴位CT
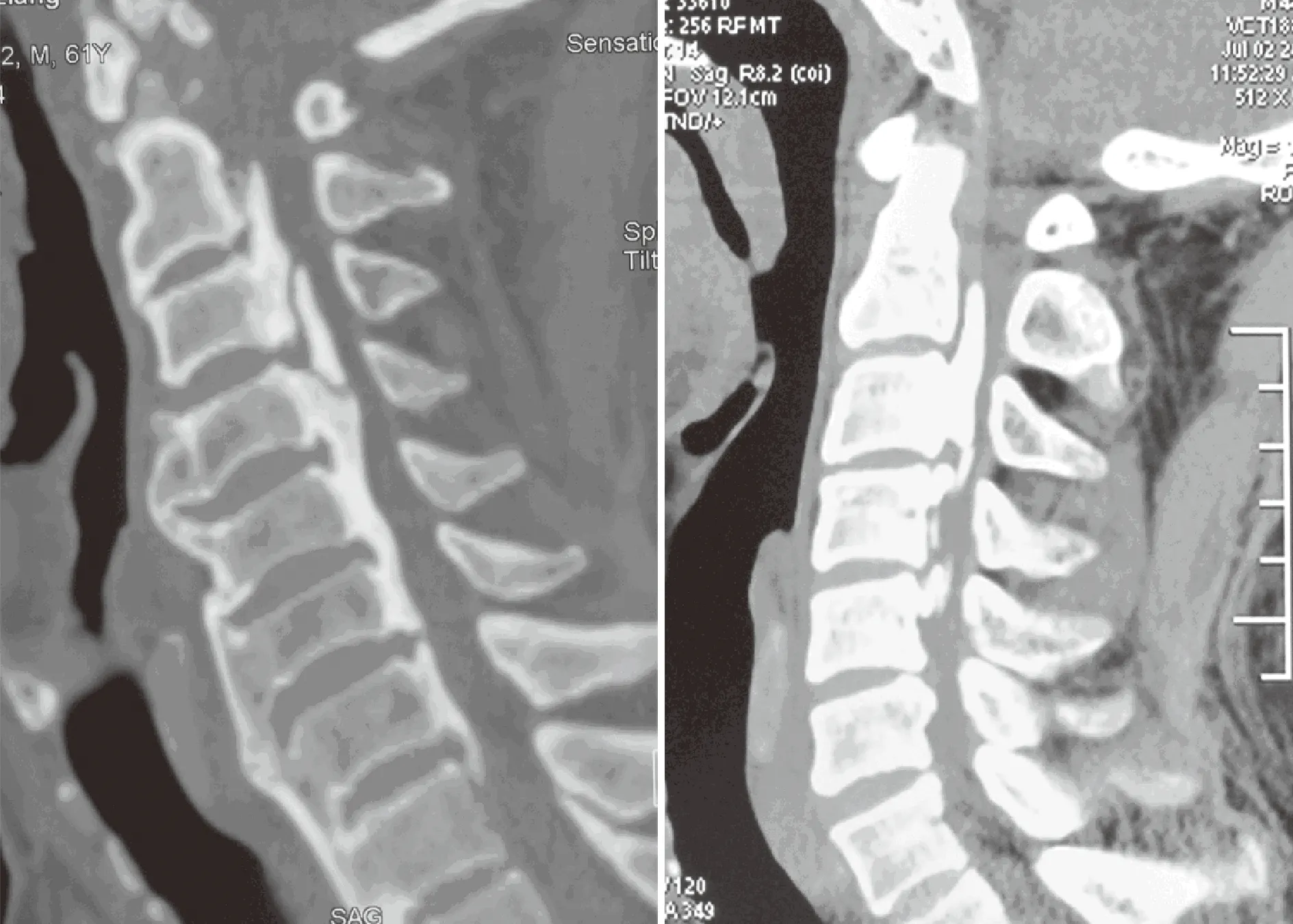
图2 颈椎侧位片 可见多节段的后纵韧带钙化,与硬膜囊粘连
因此,有术者在麻醉时先放置腰池引流,如果术中发生CSF漏,就打开腰池引流,这样可迅速有效地减少CSF的溢出,从而帮助人工硬膜进行封粘贴修补,或直接缝合修补。对于难以分离的硬脊膜或钙化的硬脊膜,可采用漂浮技术,尽量避免损伤硬脊膜。显微镜及高速磨钻的应用,可减少硬脊膜破损概率,有助于防止CSF漏。术中直接修补一般需要在显微镜下进行,将破损的硬脊膜水密缝合,无疑是CSF漏的最佳处理方法,但是由于技术要求高,操作空间不足很难实施。Hannallah等[12]报道20例CSF漏的患者中只有5例能够术中直接修补。研究显示,CSF漏术中直接修补失败率达到5%~10%。如果面对钙化的硬脊膜,或者与钙化的后纵韧带粘连紧密,很难直接缝合修补。直接缝合修补容易失败的另一原因是缝合后的针眼还可以流出CSF[2,18,25]。笔者曾试图直接使用8~0缝合线直接修补,均以失败告终,分析原因,主要由于破损往往在侧方,很难有空间操作。纤维蛋白凝胶的使用在临床上比较普遍,对于直接缝合的针眼及连接处建议用纤维蛋白胶加固。实验室研究证实纤维蛋白凝胶在配合严密缝合后可以在术后抵抗较高的CSF压力[26]。对于无法直接缝合修补的患者,若硬脊膜破损较小的可用脂肪及自体筋膜,配合纤维蛋白胶进行粘贴修补,若破损较大则可用人工硬膜配合纤维蛋白胶修补。纤维蛋白胶一般在术后5~7天吸收。因此,纤维蛋白胶只是在术后初期可以同人工硬膜或脂肪形成水密修补。在使用纤维蛋白胶时需要尽可能干燥的硬脊膜表面,吸引器尽量将CSF吸尽,如果术前已放置腰池引流,打开腰池引流将非常有助于纤维蛋白胶粘连。值得注意的是,由于纤维蛋白胶凝固后较硬,因此不能过多使用纤维蛋白胶,以免形成新的致压物。对于CSF漏的术后处理最为常用的是腰池引流,可以直接有效地降低CSF压力,减少CSF渗出,有利于硬脊膜的生长修复。由于硬脊膜的修复一般需要4~5天时间,因此建议术后腰池引流放置4~5天,引流量5~15 ml/h[27]。对于有条件的医院建议在腰池引流中使用自动调节压力和流量的泵,对于患者会相对安全。通常患者在腰池引流时,应当严格卧床休息,防止过度引流造成的低颅压、小脑扁桃体下疝以及硬脊膜破损处压力梯度增大。腰池引流需严格无菌操作,避免感染,可以预防性使用抗生素。大便软化剂可常规使用,可以避免Valsalva动作导致CSF压力梯度的巨大改变,从而破坏硬脊膜的修复。对于术后术区硬膜外引流目前存在一定争议,对于CSF漏的患者,有学者不主张放置伤口深部引流,尤其是负压吸引,担心引流可能导致硬脊膜破损处CSF压力差增大,不利于修复。笔者经验,术区硬膜外引流有助于伤口渗液的排放,促进伤口愈合,以及便于观察CSF漏的程度。脑室腹腔引流术或术腔硬膜外-腹腔分流术是最后的治疗方案,是在所有治疗手段都无效时才使用。由于分流手术存在潜在的风险,如感染、分流管阻塞、移位、过度分流或分流不足等,因此较少采用,笔者宁可选择二次手术修补CSF漏[28]。
综上所述,对于颈椎OPLL的前路手术,术前评估及手术技巧是减少CSF漏的关键。对于发生CSF漏的处理策略包含了术前影像学的判断(是否术前即放置腰池引流),术中显微镜下直接缝合修补,或使用脂肪,筋膜或人工硬脊膜,配合纤维蛋白胶进行粘连修补,术后术区引流、腰池引流等。早期干预,及时处理会取的良好预后,减少二次并发症的发生。
[1] Schmidt MH,Quinones-Hinojosa A,Rosenberg WS.Cervical myelopathy associated with degenerative spine disease and ossification of the posterior longitudinal ligament[J].Semin Neurol,2002,22:143-148.
[2] Mizuno J,Nakagawa H,Matsuo N,et al.Dural ossification associated with cervical ossification of the posterior longitudinal ligament: frequency of dural ossification and comparison of neuroimaging modalities in ability to identify the disease [J].J Neurosurg Spine,2005,2:425-430.
[3] Tani T,Ushida T,Ishida K,et al.Relative safety of anterior microsurgical decompression versus laminoplasty for cervical myelopathy with a massive ossified posterior longitudinal ligament[J].Spine,2002,27:2491-2498.
[4] Jain SK,Salunke PS,Vyas KH,et al.Multisegmental cervical ossification of the posterior longitudinal ligament: anterior vs posterior approach t[J].Neurol India,2005,53:283-286.
[5] Joseph V,Kumar GS,Rajshekhar V.Cerebrospinal fluid leak during cervical corpectomy for ossified posterior longitudinal ligament: incidence,management,and outcomet[J].Spine,2009,34:491-494.
[6] Kala M.Cerebrospinal fluid pseudocyst after anterior stabilization for cervical spine injury treated by ventricular drainage: case report t[J].Surg Neurol,1995,45:293-295.
[7] Smith MD,Bolesta MJ,Leventhal M,et al.Postoperative cerebrospinal-fluid fistula associated with erosion of the dura.Findings after anterior resection of ossification of the posterior longitudinal ligament in the cervical spine t[J].J Bone Joint Surg Am,1992,74:270-277.
[8] Epstein NE,Hollingsworth R.Anterior cervical micro-dural repair of cerebrospinal fluid fistula after surgery for ossification of the posterior longitudinal ligament t[J].Surg Neurol,1999,52:511-514.
[9] Kojima T,Waga S,Kubo Y,et al.Anterior cervical vertebrectomy and interbody fusion for multi-level spondylosis and ossification of the posterior longitudinal ligament[J].Neurosurgery,1989,24:864-872.
[10] Cammisa FP,Girardi FP,Sangani PK,et al.Incidental durotomy in spine surgery[J].Spine,2000,25: 2663-2667.
[11]Fountas KN,Kapsalaki EZ,Johnston KW.Cerebrospinal fluid fistula secondary to dural tear in anterior cervical discectomy and fusion: case report[J].Spine,2005,30: E277-E280.
[12]Hannallah D,Lee J,Khan M,et al.Cerebrospinal fluid leaks following cervical spine surgery[J].J Bone Joint Surg Am,2008,90:1101-1105.
[13]Hida K,Yano S,Iwasaki Y.Considerations in the treatment of cervical ossification of the posterior longitudinal ligament t[J].Clin Neurosurg,2008,55:126-132.
[14]Belanger TA,Roh JS,Hanks SE,et al.Ossification of the posterior longitudinal ligament.Results of anterior cervical decompression and arthrodesis in sixty-one North American patientst[J].J Bone Joint Surg Am,2005,87: 610-615.
[15]Chen Y,Guo Y,Chen D,et al.Diagnosis and surgery of ossification of posterior longitudinal ligament associated with dural ossification in the cervical spine t[J].Eur Spine J,2009,18:1541-1547.
[16]Choi S,Lee SH,Lee JY,et al.Factors affecting prognosis of patients who underwent corpectomy and fusion for treatment of cervical ossification of the posterior longitudinal ligament: analysis of 47 patients[J].J Spinal Disord Tech,2005,18: 309-314.
[17]Epstein N.Anterior approaches to cervical spondylosis and ossification of the posterior longitudinal ligament: review of operative technique and assessment of 65 multilevel circumferential procedures[J].Surg Neurol,2001,55:313-324.
[18]Min JH,Jang JS,Lee SH.Clinical results of ossification of the posterior longitudinal ligament (OPLL) of the thoracic spine treated by anterior decompression [J].J Spinal Disord Tech,2008,21: 116-119.
[19]Andrew SA,Sidhu KS.Cervical-peritoneal shunt placement for postoperative cervical pseudomeningocele [J].J Spinal Disord Tech,2005,18:290-292.
[20]Chang HS,Kondo S,Mizuno J,et al.Airway obstruction caused by cerebrospinal fluid leakage after anterior cervical spine surgery.A report of two cases [J].J Bone Joint Surg Am,2004,86-A:370-372.
[21]Saxler G,Kramer J,Barden B,et al.The long-term clinical sequelae of incidental durotomy in lumbar disc surgery[J].Spine,2005,30:2298-2302.
[22]Nakajima S,Fukuda T,Hasue M,et al.New technique for application of fibrin sealant: rubbing method devised to prevent cerebrospinal fluid leakage from dura mater sites repaired with expanded polytetrafluoroethylene surgical membranes[J].Neurosurgery,2001,49:117-123.
[23]Epstein NE.Wound-peritoneal shunts: part of the complex management of anterior dural lacerations in patients with ossification of the posterior longitudinal ligament [J].Surg Neurol,2009,72: 630-634.
[24]Black P.Cerebrospinal fluid leaks following spinal surgery: use of fat grafts for prevention and repair[J].J Neurosurg,2002,96 (2 Suppl):250-252.
[25]Narotam PK,Jose S,Nathoo N,et al.Collagen matrix (DuraGen) in dural repair: analysis of a new modified technique [J].Spine,2004,29:2861-2869.
[26]Shaffrey CI,Spotnitz WD,Shaffrey ME,et al.Neurosurgical applications of fibrin glue: augmentation of dural closure in 134 patients [J].Neurosurgery,1990,26:207-210.
[27]Cain JE,Rosenthal HG,Broom MJ,et al.Quantification of leakage pressures after durotomy repairs in the canine [J].Spine,1990,15:969-970.
[28]Mazur M,Jost GF.Schmidt MH.Management of cerebrospinal fluid leaks after anterior decompression for ossification of the posterior longitudinal ligament: a review of the literature[J].Neurosurg Focus,2011,30 (3):E13.
The managements of intra-and postoperative CSF leakage of cervical surgery of OPLL
WUHao,QIMeng,JIANFeng-zeng
(XuanwuHospitalAffiliatedtoCapitalMedicalUniversity,Beijing100053,China)
Objective To discuss the managements of intra-and postoperative cerebrospinal fluid (CSF) leakage during cervical surgery of ossification of the posterior longitudinal ligament (OPLL).Methods The authors reviewed the 124 cases of cervical surgery of OPLL from Aug.2010 to Dec.2014.Of these cases,75 cases underwent the anterior cervical corpectomy and fusion (ACCF) while 49 cases underwent the anterior cervical hybrid decompression and fusion (ACHDF) combined with corpectomy and discectomy.The data were summarized to identify the treatment options and outcomes for various situations.A treatment algorithm was identified based on these findings and the experiences of the authors.Results The incidence of CSF leakage after the operation was 3.2% (4/124).No special treatment for the cases just presented the dural tears but arachnoid was intact.These patients had a good prognosis and no CSF leakage. Patients with postoperative CSF leakage were repaired with fat or artificial dural mater with fibrin glue.The postoperative lumbar puncture and CSF drainage were performed for 4~5 days.All the end results were good.No patients with CSF leakage had the second complications such as concurrent meningitis or skin antrum.Conclusion Techniques for managements of CSF leakage including preventative measures,intra-operative dural repair with various materials,and postoperative drainage or shunt placement have all been used.Although direct dural repair is the preferred treatment for the CSF leakage,this technique is not always practically possible.Intra operative adjuncts combined with postoperative measures are an effective way to treat the CSF leakage for cervical myelopathy associated with OPLL.
Cervical OPLL;Anterior approach surgery;CSF leakage
吴 浩,男,博士,副主任医师。中华医学会脊柱脊髓分会委员,中国医师协会神经外科分会委员,华人神经脊柱外科讲师团秘书长。研究方向:脊柱退行性病变、脊髓肿瘤、椎体肿瘤、脊髓空洞、寰枕畸形等疾病的研究及治疗。
R651.2
A
1672-6170(2015)03-0004-04
2015-01-22)