Effect of row needling in muscle regions combined with seven-star needle tapping on cognitive function and quality of life in patients with post-stroke upper limb spasticity
2015-06-19HanShukai韩淑凯HaoHaiyan郝海燕LiuFenghui刘凤辉LiQing李卿LiXuefei李学飞YangWeihong杨伟红
Han Shu-kai (韩淑凯), Hao Hai-yan (郝海燕), Liu Feng-hui (刘凤辉), Li Qing (李卿), Li Xue-fei (李学飞), Yang Wei-hong (杨伟红)
1 Wangdu County Hospital of Chinese Medicine, Hebei 072450, China
2 Laishui County Hospital, Hebei 074100, China
3 Gaoling Township Health Center, Wangdu County, Hebei 072450, China
4 Dingxing County Hospital, Hebei 072650, China
5 Affiliated Hospital of Hebei University, Hebei 071000, China
Clinical Study
Effect of row needling in muscle regions combined with seven-star needle tapping on cognitive function and quality of life in patients with post-stroke upper limb spasticity
Han Shu-kai (韩淑凯)1, Hao Hai-yan (郝海燕)2, Liu Feng-hui (刘凤辉)2, Li Qing (李卿)3, Li Xue-fei (李学飞)4, Yang Wei-hong (杨伟红)5
1 Wangdu County Hospital of Chinese Medicine, Hebei 072450, China
2 Laishui County Hospital, Hebei 074100, China
3 Gaoling Township Health Center, Wangdu County, Hebei 072450, China
4 Dingxing County Hospital, Hebei 072650, China
5 Affiliated Hospital of Hebei University, Hebei 071000, China
Objective:To observe the effect of row needling in muscle regions combined with seven-star needle tapping on cognitive function and quality of life (QOL) in patients with post-stroke upper limb spasticity.
Methods:A total of 448 eligible cases were randomly allocated into a treatment group and a control group, 244 in each group. Based on standard conventional treatment, cases in the treatment group received row needling in muscle regions combined with seven-star needle tapping, whereas cases in the control group took oral Western medication. After 3 weeks of treatment, the cognitive functions were assessed using comprehensive functional assessment (CFA) and mini-mental state examination (MMSE). The QOL was evaluated using the Chinese-version 36-item short-form health survey (SF-36).
Results:After treatment, the CFA and MMSE scores were significantly improved in both groups (P<0.05); and there were between-group statistical differences (P<0.05), showing a better effect in the treatment group than that in the control group. In addition, there were between-group statistical significances in scores of QOL (P<0.05, P<0.01).
Conclusion:Row needling in muscle regions combined with seven-star needle tapping can significantly improve the cognitive function and QOL of patients with post-stroke upper limb spasticity.
Acupuncture Therapy; Cutaneous Acupuncture; Muscle Spasticity; Poststroke Syndrome; Cognition Disorders; Quality of Life
Stroke severely affects general population in China. It is characterized by high rates of morbidity, disability and relapse, and greatly endangers human health. Approximately 89% stroke survivors may develop functional disturbances in varying degrees. Spastic paralysis is a common pathologic process during stroke recovery. Muscle spasticity in most stroke patients affects recovery of the limb function. The daily quality of life (QOL) relies on normal motor function of the upper limbs. As a result, the upper limb spasticity often affects the patients’ QOL.To explore an effective treatment protocol for poststroke upper limb spasticity, we’ve adopted a multicenter randomized controlled clinical trial to measure and evaluate how row needling in muscle regions combined with seven-star needle tapping improves the patients’ cognitive function and QOL. The results are now summarized as follows.
1 Clinical Data
1.1 Diagnostic criteria
The diagnosis of cerebral infarction and cerebral hemorrhage was based on the Key Diagnostic Points for Cerebrovascular Diseases[1], coupled with skull CT scan or MRI examination. The diagnosis of upper limb spasticity was based on Clinical Practice Guidelines: Physical Medicine and Rehabilitation[2]: increased resistance in passive motion of the upper limb, joint rigidity in flexion or extension in severe spasticity; local joint and muscle pain and muscle or tendon contracture induced by long-time spasm; tendon hyperreflexia of the spastic upper limb; and limitations of the upper limb motor function and daily activities.
1.2 Inclusion criteria
Those who met the above diagnostic criteria; aged between 47 and 80 years with stable vital signs and clear consciousness; grade 1-4 of spasticity (according to modified Ashworth scale (MAS) (including grade 1 but excluding grade 4) and grade II-V of Brunnstrom stages; having a duration of less than 3 months; and voluntarily participated in the study and signed the informed consent.
1.3 Exclusion criteria
Those having unstable, critical or acute medical conditions; having disturbance of consciousness or severe cognitive impairment; having complications of severe heart, lung, liver and kidney conditions, diabetes or hemorrhagic tendency; and having been taking sedatives or muscle relaxants.
1.4 Rejection and termination criteria
Those who failed to follow the treatment protocol with a poor compliance; those who couldn’t continue with the treatment due to severe adverse reactions or events; those who need emergent measures due to severe complications or deterioration.
1.5 Statistical method
1.6 General materials
The therapeutic efficacies of 488 cases treated at Wangdu County Hospital of Chinese Medicine, Affiliated Hospital of Hebei University, Baoding No.1 Hospital of Traditional Chinese Medicine and No.252 Hospital of the Chinese People's Liberation Army between March 2007 and March 2013 were observed and the database of these cases was set up, 122 cases in each center. There were 362 inpatients and 126 outpatients. The 488 cases were randomly allocated into a treatment group and a control group, 244 in each group. Cases in the treatment group were aged between 45 and 72 years, and their duration lasted from 7 d to 2 months. Cases in the control group were aged between 47 and 81 years and their duration lasted from 6 d to 2 months. There were no between-group statistical differences in general materials (all P>0.05), indicating that the two groups were comparable (Table 1).

Table 1. Between-group comparison of general materials
1.7 Clinical trial design method
This study adopted a multi-center, randomized, controlled clinical trial design. There were four centers, a treatment group and a control group in each center. There were at least 60 cases in each center. A total of 480 cases were recruited. Considering a 15% dropout rate, the samples were expanded to 552 cases. Randomization was performed in each center simultaneously using the Visual-Basic 6.0 version software. The case ratio between the treatment group and the control group was 1:1. With random allocation concealment, patients were allocated into a treatment or control group by random envelope method. The study then started upon approval by the Ethics Committee and signature of patients on the informed content. To ensure the measurement quality, the survey crew was trained prior to the study. This study used multiple observation methods.
2 Treatment Methods
2.1 Treatment group
The meridians in upper limbs were divided into three groups according to interior-exteriorly connected relationship of the twelve regular meridians: the Lung Meridian with the Large Intestine Meridian, the Pericardium Meridian with the Triple Energizer Meridian, and the Heart Meridian with the Small Intestine Meridian.
2.1.1 Seven-star needle tapping
Tapping area: A seven-star needle was used to tap along the Lung, Pericardium and Heart Meridians, especially the Five Shu-Transmitting points, Yuan-Primary points, Luo-Connecting points, Xi-Cleft points and points around the joints. For internal rotation of the upper limb, medial border of the shoulder blade was also tapped.
Method: After sterilizing with 75% alcoholic cotton ball, the practitioner held the handle of the seven-star needle with the thumb and middle finger of the right hand, placed index finger on the upper part of the handle, used the ring and small fingers to immobilize the handle to the hypothenar, and tapped the above areas with moderate force (exerting force from the wrist until the local area turned red but not bled). The needle tip was perpendicular to the skin.
The treatment was done once a day, two meridians for each treatment, and seven times made up a course of treatment.
2.1.2 Row needling in muscle regions
Points: Five Shu-Transmitting (Jing-Well, Ying-Spring, Shu-Stream, Jing-River and He-Sea) points, Jianjing (GB 21), Jianliao (TE 14) and Jianzhen (SI 9).
Methods: The patient took a supine lying position. Filiform needles of 0.25 mm in diameter and 50 mm in length were used in this study. Bloodletting method was applied to Jing-Well points. The other points were needled perpendicularly to the superficial layer of tendons. One needle was inserted every 1-2 cun along the line connecting two adjacent points (5-7 points for each line), followed by reinforcing manipulation upon needling sensation every 10 min. The needles were retained for 30 min. The treatment was done once a day, 7 d for a course of treatment.
The treatment sequence was as follows: tap the three yin meridians of hand with a seven-star needle, row needling in muscle regions and then tap the three yang meridians of hand.
2.2 Control group
Patients received intravenous dripping of 4 g Piracetam Injection (manufactured by Shandong Lukang Cisen Pharmaceutical Co. Ltd., China Food and Drug Administration approval number: H20045019,) and 20 mL Cerebroprotein Hydrolysate in 250 mL 0.9% saline once a day, 7 d for a course of treatment. The therapeutic efficacies were evaluated after 3 courses of treatment.
3 Therapeutic Efficacy Observation
3.1 Measurement parameters
3.1.1 Cognitive function
The cognitive functions of patients in both groups were evaluated using comprehensive functional assessment (CFA)[3-4]and mini-mental state examination (MMSE)[5].
3.1.2 QOL
The Chinese-version 36-item short-form health survey (SF-36)[6]was used to evaluate the patients’ QOL. It covers 36 questions in physical, mental and subjective health summary measures, including an 8-scale profile of functional health and 1 change of health (CH). A higher score defines a more favorable QOL.
Physical function (PF): To evaluate limitations in physical activities because of health problems.
Role-physical (RP): To measure interference with work or other daily activities due to physical problems.
Bodily pain (BP): To measure pain intensity and limitations in daily activities due to pain.
General health (GH): To measure personal perception regarding health status and development tendency.
Vitality (VT): To measure personal perception regarding energy and fatigue.
Social functioning (SF): To measure the degree to which individual’s emotional or physical problems disrupt his/her normal (quantity and quality) social activities.
Role-emotional (RE): To measure the degree to which individual’s emotional problems interfere with his/her work or other daily activities.
Mental health (MH): To measure four categories of mental health items: motivation, depression, anger or emotional outburst and subjective feeling.
Each item was scored according to the score conversion.
Score conversion = (Actual score - The lowest possible score) ÷ (The highest possible score - The lowest possible score) × 100%.
Before the SF-36 form was filled in, it’s necessary to interview with the patients and explain the research objective, followed by one-to-one questionnaire survey to make sure they answer every question according to their actual health state. For illiteracy patients, a nursewas assigned to read each question. It’s important for the nurse to stay neutral and not give any hints while reading questions.
3.2 Results
3.2.1 Between-group comparison of cognitive functions
After treatment, the CFA and MMSE scores were significantly improved in both groups (P<0.05); and there were between-group statistical differences in CFA and MMSE scores (P<0.05), indicating a better improvement in cognitive function in the treatment group than that in the control group (Table 2).
3.2.2 Between-group comparison of QOL
After treatment, the scores of QOL in the treatment group were significantly higher than that in the control group (P<0.05, P<0.01), indicating a better effect in the treatment group than that in the control group (Table 3).
Table 2. Between-group comparison of cognitive function before and after treatment
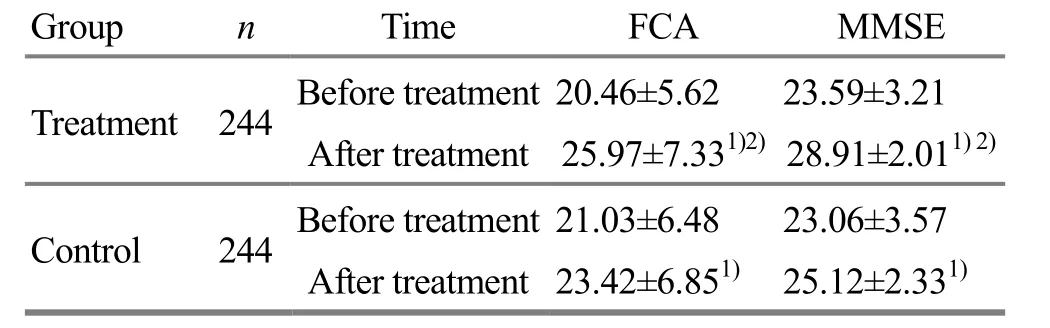
Table 2. Between-group comparison of cognitive function before and after treatment
Note: Intra-group comparison before and after treatment, 1) P<0.05; compared with the control group after treatment, 2) P<0.05
Group nTime FCA MMSE Treatment 244Before treatment 20.46±5.62 23.59±3.21 After treatment 25.97±7.331)2)28.91±2.011)2)Control 244Before treatment 21.03±6.48 23.06±3.57 After treatment 23.42±6.851)25.12±2.331)
Table 3. Between-group comparison of QOL before and after treatment
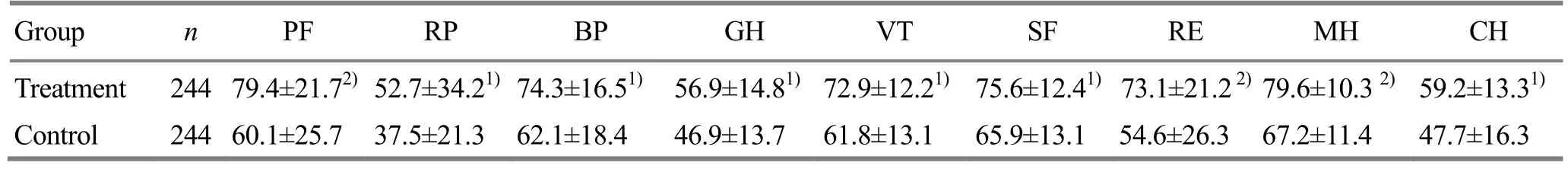
Table 3. Between-group comparison of QOL before and after treatment
Note: Compared with the control group, 1) P<0.05; 2) P<0.01
Group n PF RP BP GH VT SF RE MH CH Treatment 244 79.4±21.72)52.7±34.21)74.3±16.51)56.9±14.81)72.9±12.21)75.6±12.41)73.1±21.22)79.6±10.32)59.2±13.31)Control 244 60.1±25.7 37.5±21.3 62.1±18.4 46.9±13.7 61.8±13.1 65.9±13.1 54.6±26.3 67.2±11.4 47.7±16.3
4 Discussion
Stroke frequently affects the middle-aged and elderly population and can greatly endanger human health. Approximately 89% of stroke survivors may develop functional disorders. Spastic paralysis is a common pathologic process during stroke recovery. It can severely affect the patient’s limb function and cause economic burden to families and society. In addition to limb function, stroke patients may also manifest dysfunctions in cognitive ability. Over the recent years, along with the transformation of new biopsychosocial medical model, the focuses of evaluation on diseases and clinical efficacy have gradually turned to physiology, psychology and social functioning, especially the patient’s QOL.
In Chinese medicine, post-stroke upper limb spasticity falls under the category of ‘wind stroke’ and ‘spasm syndrome’. Contributing factors include wind-phlegm obstructing the meridians, disorders of qi and blood, malnourishment of tendons and yin-yang imbalance. This condition is characterized by ‘flaccidity in the yang side and spasticity in the yin side’. The three yang meridians of hand pertain to Fu organs and connect with Zang organs, whereas the three yin meridians of hand pertain to Zang organs and connect with fu-organs. The three yang meridians of hand and three yin meridians of hand are internal-externally connected. Consequently, this study established the treatment strategy of reinforcing deficiency, reducing excess and balancing yin and yang by row needling along the muscle regions.
Muscle regions are external connecting parts of the twelve regular meridians, referring to tendons, muscles and regions where qi and blood of the twelve regular meridians gather. They often originate from the four extremities (between finger/toe nails) and terminate over the head and face. Muscle regions act to circulate qi and blood, soften tendons and bones, lubricate joints and contribute to motor system of the body. Since they travel superficially, muscle regions are easily affected by external pathogens. Main pathogenic factors affecting muscle regions include phlegm, deficiency and stasis. Invasion by external pathogens or acute lesion may impair anti-pathogenic qi and result in phlegm-stasis in meridians and subsequently, disorders of muscle regions. This study adopted row needling of muscle regions of the three yang meridians of hand to harmonize qi and blood to alleviate flaccidity and also to unblock meridians and lubricate joints to activate flaccid muscle regions.
The stroke affects the brain. All three yang meridians of hand ascend to the head. Since meridians are indicated for problems along the pathway of meridians, stimulating the muscle regions along the upper limbs can refresh the mind, activate meridian qi and blood and thus nourish muscle regions and benefit recovery of the upper limb functions.
In addition, row needling in muscle regions can extensively stimulate nerves of the upper limb, improve neurotrophy and excitability, boost metabolism of nerve tissue and speed up recovery of affected nerves. This method can also increase local circulation of blood,generate muscle contraction on the flaccid limb and improve the muscle tone.
Cutaneous regions are superficial divisions of the twelve regular meridians on the surface of the body. External pathogenic factors often affect the cutaneous regions first and transmit into Zang-fu organs via meridians. On the other hand, problems of Zang-fu organs may manifest on cutaneous regions via meridians. Consequently, stroke patients may have ropy band of fibers along the pathways of three yin meridians of hand. That’s why we adopted seven-star needling tapping cutaneous regions of the three yin meridians of hand in this study, with the goal of harmonizing Zang-fu organs and brain and balancing excitability and inhibition through optimally stimulating cutaneous regions, minute collaterals, collaterals, meridians and Zang-fu organs. Previous studies have suggested that acupuncture can reflexively excite cerebral cortex, accelerate blood flow, increase brain cell activity, speed up the absorption of focal lesion, and facilitate the compensation of undamaged cells. In addition, it can activate brain cells in an inhibitory state and benefit recovery of the limb function[7].
The study findings regarding the effect of row needling in muscle regions combined with seven-star needling tapping for post-stroke upper limb spasticity have shown that there were between-group statistical differences in comparing CFA and MMSE scores (P<0.05), indicating that this method can significantly improve the patient’s cognitive function. The SF-36 includes an 8-scale profile of physical and mental health summary measures. It has proven useful in surveys of general and specific populations, comparing the relative burden of diseases, and in differentiating the health benefits produced by a wide range of different treatments[8]. Accordingly, it has better reliability, validity and reactivity. After treatment, the QOL scores in the treatment group were significantly higher than that in the control (P<0.05 or P<0.01), indicating that row needling in muscle regions combined with sevenstar needle tapping can substantially improve the patient’s QOL.
Clinical studies have confirmed the distinctive effect of acupuncture for stroke[9-11]. Based on continuous circulation of qi and blood through meridians and holistic view in Chinese medicine, this study adopted row needling in muscle regions combined with sevenstar needle tapping therapy to regulate the whole body and balance yin and yang. As a result, this method can increase stimulation to points and activate functions of meridians and points. Additionally, the two methods can integrate reinforcing and reducing, connect the interior with the exterior, achieve yin-yang balance and work well for post-stroke upper limb spasticity.
Conflict of Interest
The authors declared that there was no conflict of interest in this article.
Acknowledgments
This work was supported by Scientific Research Project of Hebei Provincial Administration Bureau of Traditional Chinese Medicine (河北省中医药管理局科研计划项目, No. 2009180).
Statement of Informed Consent
All of the patients signed the informed consent.
Received: 30 August 2014/Accepted: 12 October 2014
[1] Chinese Neuroscience Society, Chinese Neurosurgical Society. Key diagnostic points for cerebrovascular diseases. Zhonghua Shenjingke Zazhi, 1996, 29(6): 379-380.
[2] Chinese Medical Association. Clinical Practice Guidelines: Physical Medicine and Rehabilitation. Beijing: People’s Medical Publishing House, 2005: 11-14.
[3] Hu YS, Wu Y, Fan WK, Yang XB. Study on comprehensive functional assessment scale (I): scale design. Zhongguo Kangfu Yixue Zazhi, 2002, 17(1): 35-38.
[4] Fan WK, Hu YS, Wu Y, Yang XB. A research on validity of comprehensive functional assessment. Zhongguo Kangfu Yixue Zazhi, 2003, 18(6): 325-329.
[5] Xu SF, Zhuang LX, Jia C, Chen XH, Wu SP, Jiang GM, Zhu BC, Xu DJ, Pan CA. Effect of ‘Jin three-needle therapy’ on cognitive function and activity of daily living in patients of hemiplegia after stroke: a multi-center randomized controlled study. Zhongguo Zhen Jiu, 2009, 29(9): 689-694.
[6] Xu MM, Luo CE, Lin MH. Assessment of Chinese-version SF-36 scale on rehabilitative care of patients with coronary artery disease. Int J Nurs, 2006, 25(5): 369-370.
[7] Li JC, Wang SX, Du ZS, Dong HL. Point injection for 116 cases with spastic cerebral palsy. Linchuang Yixue, 2000, 20(9): 32-33.
[8] Ware JE, Snow KK, Kosinski M, Gandek B. SF-36 Health survey-manual and interpretation guide. Boston, MA: The Health Institute, New England Center, 1993.
[9] Liao FR, Fu CW. Clinical study of yin-yang harmonizing acupuncture plus rehabilitation training for the treatment of post-stroke spastic paralysis. Shanghai Zhenjiu Zazhi, 2013, 32(4): 250-252.
[10] Li FL. Observation on the efficacy of antagonistic muscle acupuncture plus rehabilitation training in treating post-stroke spastic hemiplegia. Shanghai Zhenjiu Zazhi, 2012, 31(11): 794-796.
[11] Hou LJ, Han SK, Gao WN, Xu YN, Yang XW, Yang WH. Aligned acupuncture at muscle regions plus cutaneous needle for upper limb spasticity after stroke: a multicenter randomized controlled trial. J Acupunct Tuina Sci, 2014, 12(3): 141-145.
Translator: Han Chou-ping (韩丑萍)
经筋排刺配合皮肤针疗法对脑卒中后上肢痉挛患者认知功能及生活质量的影响
目的: 观察经筋排刺配合皮肤针疗法对脑卒中后上肢痉挛患者认知功能及生活质量的影响。方法: 将488例脑卒中后上肢痉挛患者随机分为治疗组和对照组, 每组244例, 在必要康复治疗的基础上, 治疗组给予经筋排刺配合皮肤针疗法, 对照组给予常规西药治疗。两组均连续治疗3星期后观察疗效。采用功能综合评定量表(functional comprehensive assessment, FCA)和简易精神状态检查量表(mini-mental state examination, MMSE)评价患者认知功能;采用健康状况调查问卷(36-item short-form health survey, SF-36)中文版评价患者的生活质量。结果:治疗后, 两组FCA、MMSE评分均较治疗前有明显改善(P<0.05), 且治疗组改善情况均优于对照组, 两组间差异均有统计学意义(P<0.05)。治疗组患者各项生活质量评分均明显高于对照组, 差异有统计学意义(P<0.05, P<0.01)。结论: 经筋排刺配合皮肤针疗法能明显改善脑卒中后上肢痉挛患者的认知功能, 提高其生活质量。
针刺疗法; 皮肤针疗法; 肌痉挛; 中风后遗症; 认知障碍; 生活质量
R246.6 【
】A
in both groups
anti-spasm rehabilitation training, such as placing of normal upper limb position, maintaining the joint range of motion, alleviation of body motion control points around the spasm, static muscle stretch, passive movement and massage.
Author: Han Shu-kai, vice chief physician.
E-mail: hanshukai1975@163.com
猜你喜欢
杂志排行
Journal of Acupuncture and Tuina Science的其它文章
- Therapeutic effect of tuina combined with Jin Gui Shen Qi Decoction on lumbar spinal stenosis
- Clinical observation of warm needling moxibustion for rheumatoid arthritis
- Electroacupuncture down-regulates the expressions of colonic NGF and NGFR in visceral hypersensitivity rats
- Summary of Professor Jin Yi-cheng’s academic thoughts on pediatric tuina therapy
- Triple needling plus moxibustion and Tanbo-plucking tender points for the third lumbar vertebra transverse process syndrome
- Effect of ginger-partitioned moxibustion on immunocytokines in patients with chronic nonbacterial prostatitis