Epidemiological Study of Heart Failure in China
2015-05-22YangGuoDongZhaoandJingLiu
Yang Guo, Dong Zhao and Jing Liu
1Department of Epidemiology, Beijing Anzhen Hospital, Capital Medical University, Beijing Institute of Heart, Lung and Blood Vessel Diseases, Beijing, China
Introduction
Heart failure (HF) is a complex clinical syndrome that results from any structural or functional impairment of ventricular filling or ejection of blood. The cardinal manifestations of HF are dyspnea and fatigue, which may limit exercise tolerance, and fl uid retention, which may lead to pulmonary and/or splanchnic congestion and/or peripheral edema.HF is one of the most important and severe end stages of many cardiovascular diseases [1, 2]. Epidemiological studies of HF have focused mainly on the prevalence, incidence, mortality, fatality, and distribution and temporal trends of these indicators among different populations. The purpose of this review is to highlight important epidemiological studies of HF in China.
Prevalence
The prevalence of HF refers to the rate of patients with HF in the specific population at the time of investigation. The prevalence of HF varies with time, population, area, and characteristics ( Table 1).
The Chinese Multicenter Cooperation Study on Cardiovascular Health [4], the first national investigation of chronic HF prevalence in China, enrolled 15,518 adults aged 35–74 years from 10 provinces(f i ve northern and fi ve southern) using a four-stage random-sampling method. The prevalence rates of chronic HF were 0.9%, 0.7%, and 1.0% for the overall population, males, and females, respectively. When stratif i ed by age, the prevalence rates of chronic HF were 0.4%, 1.0%, 1.3%, and 1.3% for groups aged 35–44, 45–54, 55–64, and 65–74 years,respectively, demonstrating the substantial increase in the prevalence of chronic HF with aging. The risk of chronic HF was higher in northern China (1.4%)than in southern China (0.5%), and was higher in urban areas (1.1%) than in rural areas (0.8%).
A large-scale study of regional chronic HF prevalence investigated the epidemiological characteristics and treatment of chronic HF in ruralareas of Liaoning province [3]. By means of cluster random sampling, 33,027 rural residents aged 25–95 years were recruited. The study demonstrated that the rates of chronic HF prevalence were 1.61%, 0.95%, and 2.28% in the overall, male, and female populations, respectively. The prevalence rates of 0.12%, 0.79%, 1.98%, 3.71%, and 7.51%in groups aged 25–34, 35–44, 45–54, 55–64, and 65–74 years, respectively, demonstrated a substantial increase with age. The prevalence of chronic HF in females was substantially higher than that in males in every age group.
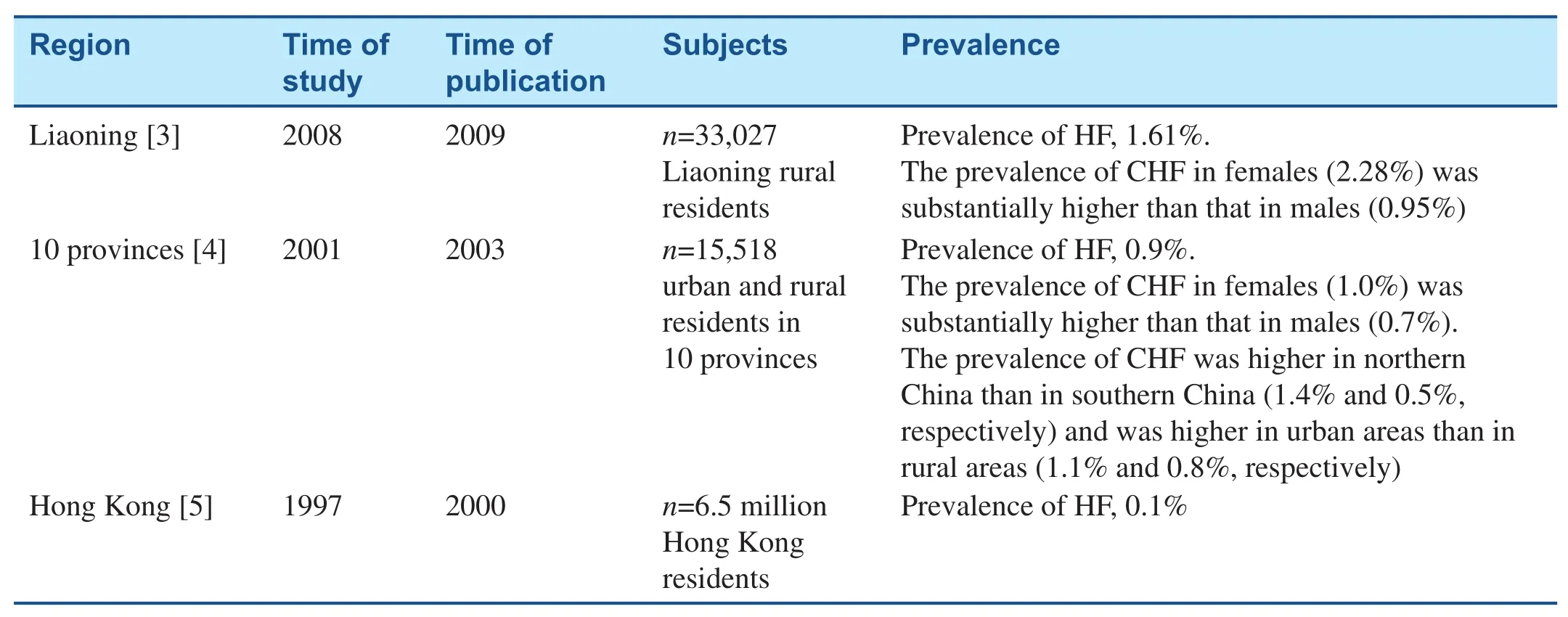
Table 1 Studies on the Prevalence of Heart Failure (HF) in China.
In 1997, Hung et al. [5] conducted a retrospective study of HF in Hong Kong by recruiting all patients admitted to the 11 hospitals of the Hospital Authority, Hong Kong, with a primary diagnosis of HF. A total of 6,203 patients were admitted from the emergency departments of these hospitals, among which 4,589 were new cases and 1,614 were old cases. To calculate the prevalence of HF that required hospital admission, the numbers of old and new cases were added; the corresponding prevalence rates for the 55–64-year and 65–74-year age groups were 1.3 and 4.4 per 1,000 men and 0.9 and 3.9 per 1,000 women, respectively.This study was based on hospitalization data rather than data from a population survey, which may partly explain the lower prevalence of HF in this study.
Incidence
The incidence of HF refers to the rate of new HF cases occurring during a certain time period (generally 1 year) in the population at risk.
In China, the only study [5] reporting the incidence of HF was the afore mentioned study in Hong Kong. Among the 6,203 patients admitted from 11 hospitals, 4,589 were new cases. The incidence of HF was about 0.07% (number of new cases divided by the population of Hong Kong that year) and, when stratif i ed by age groups, showed a rising trend with age. In the group aged more than 85 years, the incidence for women was 2% and that for men was 1.4%.
Etiology
HF is the severe end stage of a number of heart diseases, and its causes differ with economic performance/geographical area, living conditions, and living habits. The spectrum of causes of HF has changed with alterations in living conditions and habits caused by socioeconomic transformation(Table 2).
In the 1980s, almost 50% of HF cases were attributable to rheumatic valvular heart disease, but the incidence of HF has declined signifi cantly in the past three decades. Damage to the heart can be mitigated early because of improvements in living conditions and habits that have resulted from fast economic
development and popularization of rheumatic valvular heart disease prevention and early detection and treatment. There has been a clear increase in the incidence of coronary heart disease (CAD) because of unhealthy lifestyles and the concomitant rise in risk factors for atherosclerosis. The CAD mortality rate, however, has gradually decreased because of improved management of acute CAD events.Therefore, CAD has become the main cause of HF in China.
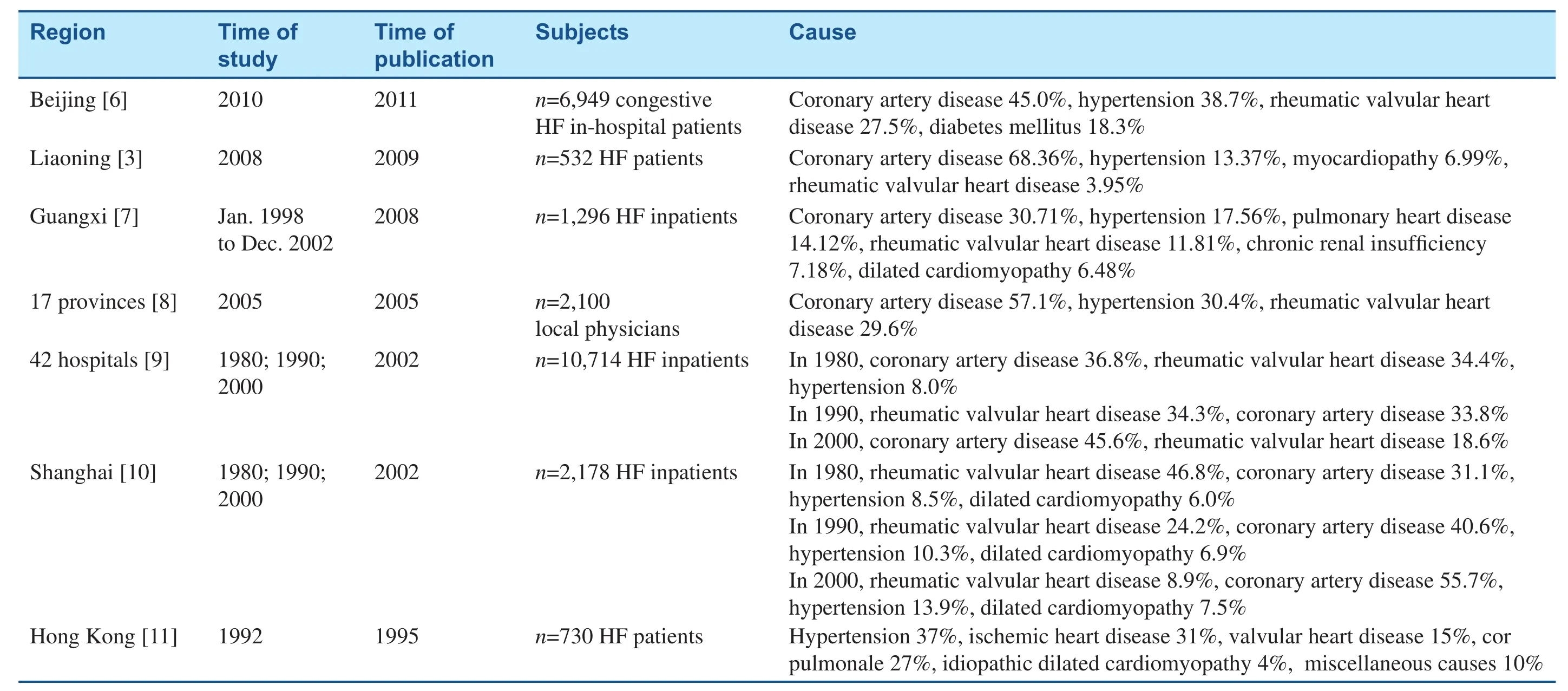
Table 2 Studies of the Causes of Heart Failure (HF) in China.
A retrospective investigation of hospitalized patients with HF in some parts of China in 1980, 1990, and 2000 [9] analyzed the data of patients with primary diagnoses of chronic HF from 42 hospitals in urban China. This study demonstrated that the common causes of HF were CAD, rheumatic valvular heart disease, and hypertension. From 1980 to 2000, the rate of CAD rose from 36.8% to 45.6%, and the rate of hypertension rose from 8.0% to 12.9%. Over the same period, the rate of rheumatic valvular heart disease fell from 34.4% to 18.6%, and the proportion of all cardiac deaths caused by HF remained unchanged.
A study from a tertiary hospital in Beijing [6]identif i ed 6,949 patients (4,344 males and 2,605 females) with a principal International Classification of Diseases, Ninth Revision, Clinical Modif i cation (ICD-9-CM) discharge diagnosis of congestive HF. The reasons for hospitalization of patients with congestive HF were CAD (45.0%), hypertension(38.7%), valvular heart disease (27.5%), and diabetes mellitus (18.3%).
A pilot survey of the main causes of chronic HF in patients treated in primary hospitals in China was conducted by Cao et al. [8]. Local physicians from 2,066 local hospitals (at least one cardiologist,emergency department physician, or attending physician from each hospital) in 17 areas (11 provinces,three municipalities, and three autonomous regions)responded to questionnaires regarding hospitalized HF patients, and 2,100 valid responses were obtained. The research showed that the top three main causes of chronic HF were CAD (57.1%),hypertension (30.4%), and rheumatic heart disease(29.6%). In some places, chronic pulmonary heart disease was also a main cause of admission for chronic HF in primary hospitals.
The Shanghai Investigation Group of Heart Failure [10] analyzed evolving trends in the epidemiological factors and treatment of hospitalized patients with congestive HF in Shanghai during 1980, 1990,and 2000 using a retrospective method based on case records. A total of 2,178 patients were enrolled(mean age, 64.0 ± 16.0 years). The results showed that the cause of HF had shifted signifi cantly from rheumatic valvular disease to CAD during the first two decades; the rate of HF due to rheumatic valvular disease decreased from 46.8% to 8.9%, and that of HF due to CAD rose from 31% to 55.7%.
An investigation of epidemiological characteristics and treatment of chronic HF in rural areas of Liaoning province [3] was conducted by cluster random sampling. A total of 33,027 rural residents aged 25–95 years from six counties of Liaoning province were enrolled: 532 were found to have HF.The study demonstrated that the causes of chronic HF were CAD (68.36%), hypertension (13.37%),myocardiopathy (6.99%), rheumatic valvular disease (3.95%), congenital heart disease (1.69%), and other cardiovascular disease (5.27%). Compared with previous studies, the proportion of HF cases caused by CAD increased signifi cantly, ranking first; the prevalence of hypertension and myocardiopathy increased slightly, whereas the proportion of HF cases due to rheumatic valvular disease decreased substantially.
A retrospective study by Li [7] analyzed disease causes and prognosis of 1,296 hospitalized chronic HF patients in Guangxi province. The causes of chronic HF were CAD (30.71%), hypertensive heart disease (17.56%), pulmonary heart disease(14.12%), rheumatic valvular disease (11.81%),chronic renal insuff i ciency (7.18%), and dilated cardiomyopathy (6.48%).
Sanderson et al. [11] conducted the first epidemiological study of HF in Hong Kong. The prospective study of 730 consecutive HF patients (mean age,73.5 ± 11.7 years) was performed to identify the main risk factors for or possible causes of HF. The main identif i able risk factors were hypertension(37%), CAD (31%), valvular heart disease (15%),cor pulmonale (27%), idiopathic dilated cardiomyopathy (4%), and miscellaneous factors (10%).
Medical Therapy
The common pathogenesis of HF is myocardial remodeling resulting in myocardial death (e.g.,necrosis, apoptosis, and autophagy) and systemic reaction to overactivation of the renin-angiotensinaldosterone system and the sympathetic nervous system. The foundation of effective HF prevention and treatment is to interfere with the disease process of this neurohormonal system [1] (Table 3).
The Bridging the Gap on CHD Secondary Prevention in China (BRIG) project [12] enrolled 65 hospitals from 31 provinces in mainland China and the Hong Kong Special Administrative Region using a multistage nonrandomized sampling approach.A questionnaire was completed according to the medical records of 3,168 patients with acute coronary syndrome. There were 706 patients (22.3%)with acute HF, and 262 (8.3%) HF patients did not have an acute episode during hospitalization.The prescription rates were determined for aspirin(90.1%/92.7%), β-blockers (76.3%/77.6%), angiotensin-converting enzyme inhibitors (ACEIs)/angiotensin-receptor blockers (63.7%/67.6%),statins (59.2%/70.4%), and clopidogrel/ticlopidine(30.5%/40.1%) in HF patients without acute HF and acute HF patients, respectively.
The investigation of hospitalized patients with HF in some parts of China in 1980, 1990, and 2000 [9] demonstrated that medical treatment during hospitalization was mainly diuretic (55.4%),nitrate (43.2%), and digoxin (48.2%) therapy. The administration of digoxin decreased slightly (51.7%in the 1980s, 45.5% in the 1990s, and 40.3% in the first decade of this century, respectively). The use of β-blockers and ACEIs increased gradually,from 8.5% and 14.0%, respectively, in the 1980s to 19.0% and 40.4%, respectively, in the first decade of this century.
The Shanghai Investigation Group of Heart Failure [10] study showed that medical treatment has remained mostly conventional in the past decades,and determined the proportions of diuretics (77.1%),nitrate (74.4%), and digoxin (60.0%) administered.ACEI and β-blocker administration substantially increased, but the use of digoxin decreased.
The survey of local physicians by Cao et al. [14]showed that current chronic HF medications used in primary hospitals in China were not optimal.The usage rate of high-dose digitalis (≥0.25 mg/day) was 10%. The rates of β-blocker and ACEI administration were still low (40% and 80%,respectively), and the usage rates of target doses of β-blocker and ACEI were even lower (1% and 2%, respectively), and in some underdeveloped areas (e.g., Qinghai and Guizhou provinces) were zero. The usage rate of diuretics in symptomatic chronic HF patients was 90%.
An investigation of the epidemiological characteristics and treatment of chronic HF in some rural areas of Liaoning province [3] demonstrated that traditional Chinese medicine was widely used in this rural area and that the administration of recommended medicine was still very limited. The drugs used were digoxin (6.8%), furosemide (2.45%),hydrochlorothiazide (1.69%), spironolactone(0.38%), ACEIs (4.33%), β-blockers (3.77%), and nitrate (3.77%).
An investigation of the prevalence and related factors of medicinal therapy in patients with chronic systolic HF was done by Yu et al. [13].Data on 16,681 patients hospitalized with chronic systolic HF were taken from 12 tertiary hospitals in eight cities of Hubei province in 2000 to 2010.Analysis determined the usage rates of β-blockers(46.58%), ACEIs (51.60%), angiotensin-receptor blockers (18.68%), digitalis (46.24%), and diuretics (69.13%). The use of angiotensin II–receptor blockers increased with age, and the distribution of digitalis, diuretics, β-blockers, and ACEIs showed an inverted-U shape. Sex differences were seen between different age groups.
Prognosis
The indicators of prognosis include mortality and rehospitalization rate. Mortality refers to the rate of death among HF patients, including in-hospital mortality and long-term mortality (1–5 years).The prognosis of HF is closely associated with the patient’s age and quality of life, the disease course,and the severity. A declining trend has been demonstrated for HF mortality with improving treatment over the past few decades (Table 4).
The BRIG project [12] demonstrated the in-hospital mortality rates of HF patients and acute HF patients were 1.9% and 10.8%, respectively. The incidence of composite end point (death, myocardial reinfarction /infarction, serious dysrhythmia,and stroke) in HF patients and acute HF patients was 6.9% and 30.3%, respectively. The median lengths of hospital stay were 11.3 days for HF patients and 13.2 days for acute HF patients.
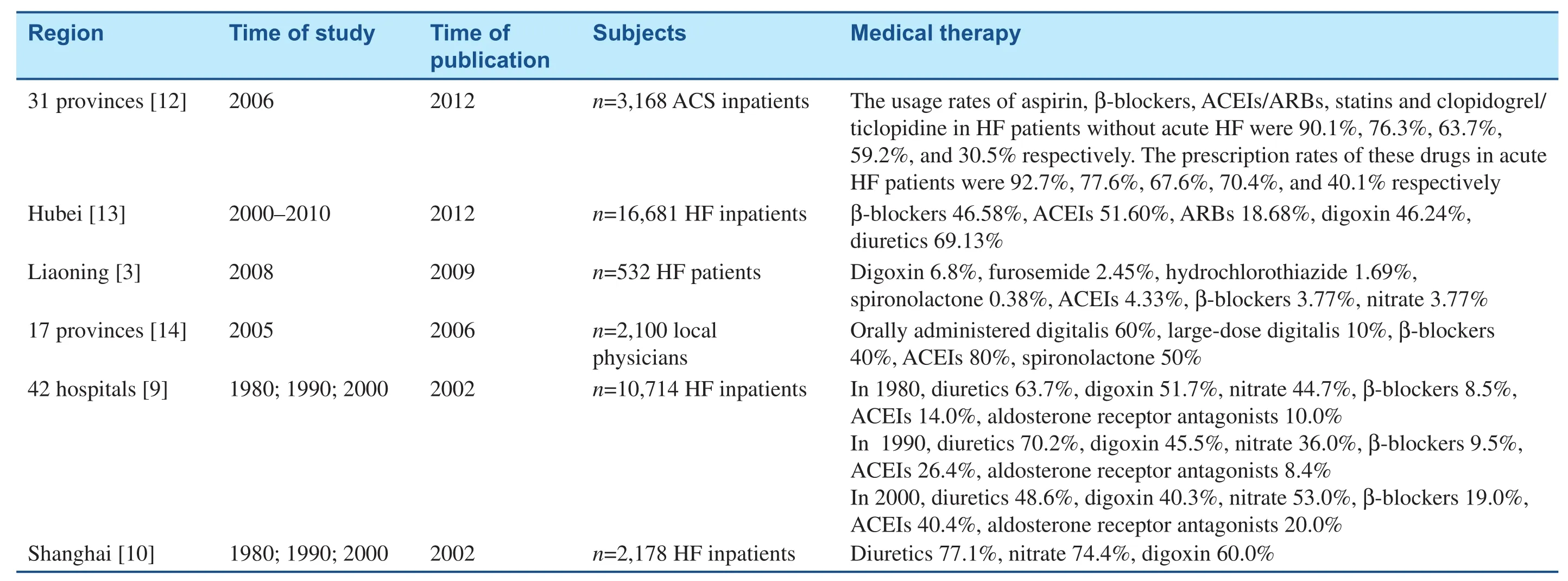
Table 3Studies on Medical Therapy for Heart Failure (HF) in China.
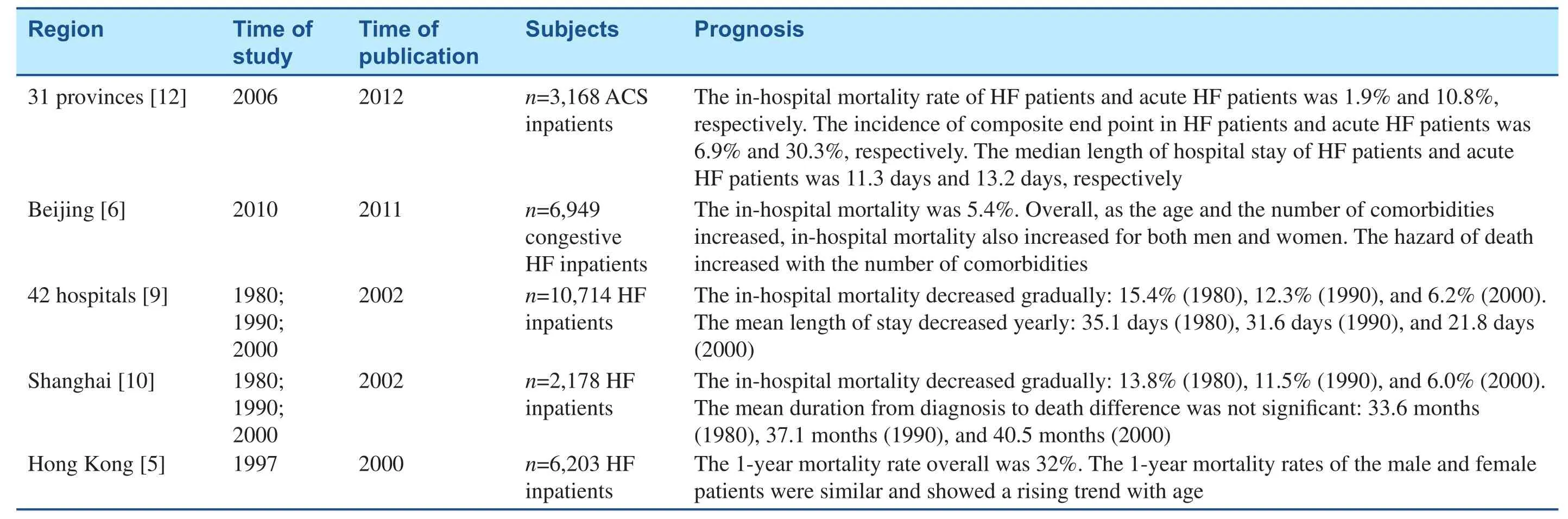
Table 4 Studies on the Prognosis of Heart Failure (HF) in China.
A retrospective investigation of hospitalized patients with HF in some parts of China in 1980,1990, and 2000 [9] found that the rates of correction of HF during hospitalization were 15.5% in 1980, 19.6% in 1990, and 22.2% in 2000. Mortality decreased signifi cantly in those years, from 15.4%in 1980 to 12.3% in 1990 to 6.2% in 2000, but was still higher than that of all cardiac diseases during the same period. The mean length of stay decreased from 35.1 days in 1980 to 31.6 days in 1990 to 21.8 days in 2000.
In a Beijing study [6] of 6,949 congestive HF patients , in-hospital mortality was 5.4%. Overall,in-hospital mortality increased with age and the number of comorbidities in both men and women.The hazard of death increased with the number of comorbidities.
The Shanghai Investigation Group of Heart Failure [10] retrospective study of 2,178 patients revealed that in-hospital mortality declined from 13.8% in 1980 to 11.5% in 1990 to 6% in 2000.The mean duration from diagnosis to death was 33.6 months in 1980, 37.1 months in 1990, and 40.5 months in 2000. The average number of emergency visits and hospital admissions within 1 year before the current hospitalization numbered 3.1 in 1980,2.8 in 1990, and 2.0 in 2000. The major causes of death were progressive HF (53.2%) and complications (38.2%).
A retrospective study [5] of HF in Hong Kong began in 1997 and analyzed survival status up to 1 year. The 1-year mortality rate overall was 32%;the 1-year mortality rates of male and female patients were similar and showed a rising trend with age. Old cases of HF had a 5–10% higher mortality rate than new cases across all age groups.
Conclusion and Take-Home Message
HF is becoming more prevalent in China, especially in older people. This results in increasing medical costs and increasing rates of disability and mortality.At present, evidence from epidemiological research on HF in China is not yet suff i cient to guide the development of prevention strategies. Therefore,large-scale epidemiological studies should be conducted to assess the current situation and overall trends, and to provide a scientif i c basis for effective prevention strategies.
Conflict of Interest
The authors declare no conf l ict of interest.
Funding
This work was supported by grants from the National Science & Technology Pillar Program during the 12th Five-Year Plan Period (contract nos. 2011BAI08B00 and 2011BAI11B03). This funding body had no role in the study design,data analysis, data interpretation, or writing of the manuscript.
1. Huang J, Yang JF, Zhang J. China heart failure diagnosis and treatment guideline 2014. Chin J Cardiol 2014;(2):98–122.
2. Yancy CW, Jessup M, Bozkurt B,Butler J, Casey Jr DE, Drazner MH,et al. 2013 ACCF/AHA guideline for the management of heart failure:a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2013;62(16):e147–239.
3. Sun XQ, Li JS, Lang YJ, Sui YY,Fu Y, Wang XH, et al. Investigation of epidemiologic features and treatment of chronic heart failure in some rural parts of Liaoning province. Chinese J Pract Intern Med 2009;(11):1000–2.
4. Gu DF, Huang GY, He J, Wu XG,Duan XF, MacMahon S, et al. Investigation of prevalence and distributing feature of chronic heart failure in Chinese adult population.Chin J Cardiol2003;(1):3–6.
5. Hung YT, Cheung NT, Ip S, Fung H. Epidemiology of heart failure in Hong Kong, 1997. HKMJ 2000;6:159–62.
6. Yin Q, Zhao Y, Li J, Xue Q, Wu X, Gao L, et al. The coexistence of multiple cardiovascular diseases is an independent predictor of the 30-day mortality of hospitalized patients with congestive heart failure: a study in Beijing. Clin Cardiol 2011;34(7):442–6.
7. Li X. Clinical epidemiologic analysis of 1296 patients with chronic heart failure. Practical Journal of Cardiac Cerebral Pneumal and Vascular Disease 2008;(6):71–2.
8. Cao YM, Hu DY, Wu Y, Wang HY.A pilot survey of the main causes of chronic heart failure in patients treated in primary hospitals in China. Zhonghua nei ke za zhi 2005;(7):487–9.
9. Cheng KA. Retrospective investigation of hospitalized patients with heart failure in some parts of China in 1980, 1990 and 2000. Chin J Cardiol 2002;(8):5–9.
10. Shanghai Investigation Group of Heart Failure. The evolving trends in the epidemiologic factors and treatment of hospitalized patients with congestive heart failure in Shanghai during years of 1980, 1990, 2000. Chin J Cardiol 2002;(1):24–27.
11. Sanderson JE, Chan SK, Chan WW, Hung YT, Woo KS. The aetiology of heart failure in the Chinese population of Hong Kong– a prospective study of 730 consecutive patients. Int J Cardiol 1995;51(1):29–35.
12. Wang N, Zhao D, Liu J, Liu J,Yu CM, Wang W, et al. Impact of heart failure on in-hospital outcomes of acute coronary syndrome patients in China – results from the Bridging the Gap on CHD Secondary Prevention in China (BRIG) project. Int J Cardiol 2012;160(1):15–9.
13. Yu SB, Zhao QY, Cui HY, Qin M,Liu T, Kong B, et al. Investigation on the prevalence and related factors of medicinal therapy in patients with chronic systolic heart failure. Zhonghua liu xing bing xue za zhi 2012;33(2):229–33.
14. Cao YM, Hu DY, Wang HY, Wu Y. A survey of medical therapies for chronic heart failure in primary hospitals in China. Zhonghua nei ke za zhi 2006;(11):907–9.
杂志排行
Cardiovascular Innovations and Applications的其它文章
- Mechanical Circulatory Support for the Failing Heart: Which Device to Choose
- Continuous Flow Left Ventricular Assist Device Therapy: A Focused Review on Optimal Patient Selection and Long-Term Follow-up Using Echocardiography
- Cardiac Resynchronization Therapy in 2015:Lessons Learned
- Pulmonary Arterial Hypertension and the Failing Ventricle: Getting It Right
- The Evaluation of the Heart Failure Patient by Echocardiography: Time to go beyond the Ejection Fraction
- Noninvasive Hemodynamic Monitoring for Heart Failure: A New Era of Heart Failure Management