氨基末端脑钠肽对老年血液透析合并充血性心力衰竭的心功能诊断分级的判断价值
2014-07-18刘玉华闫国强王月娥
孙 波,刘玉华,李 晟,闫国强,孙 岩,陈 杰,王月娥
氨基末端脑钠肽对老年血液透析合并充血性心力衰竭的心功能诊断分级的判断价值
孙 波1,刘玉华2,李 晟1,闫国强1,孙 岩1,陈 杰1,王月娥1
目的探讨氨基末端脑钠肽(N terminal-pro brain nalriuretic peptide,NT-proBNP)水平变化对老年血液透析合并充血性心力衰竭诊断和心功能分级的判断价值。方法选择尿毒症维持性血液透析(maintenance hemodialysis,MHD)合并心力衰竭患者36例作为血透心衰组,选择非血液透析、CKD3期以上[eGFR>60 ml/(min·1.73m2)]的心力衰竭患者38例作为对照组,测定两组心力衰竭及治疗好转后心功能不同等级时的NT-proBNP,采用受试者工作特征(receive operating characteristic,ROC)曲线评价NT-proBNP的诊断效能。结果血透心衰组和对照组治疗后随心功能好转,血清NT-proBNP水平下降, 不同心功能分级间NT-proBNP水平有统计学差异(P<0.05或P<0.01)。血透心衰组各心功能分级NT-proBNP水平明显高于对照组,差异有统计学意义(P<0.05)。血透心衰组心功能Ⅳ级AUC值为0.847,NT-proBNP>11 100 ng/L作为界值(cutoff值)的敏感度为83%,特异度为79%;心功能Ⅲ级AUC值为0.794,NT-proBNP>6465 ng/L作为界值的敏感度为100%,特异度为56.4%,心功能Ⅰ级和Ⅱ级时无统计学差异。结论老年MHD合并心力衰竭时NT-proBNP可作为判断心力衰竭及心功能Ⅲ级、Ⅳ级的分级指标。
维持性血液透析;氨基末端脑钠肽;纽约心脏病协会;受试者操作特征曲线下面积
尿毒症维持性血液透析患者心力衰竭患病率明显高于健康人群[1]。血清NT-proBNP已经作为心力衰竭诊断、评价疗效和预后的重要指标[2,3],但对于该指标在MHD合并心力衰竭患者中的动态变化,以及判断预后和心功能分级的评价还有不同观点[3-7]。笔者发现,老年MHD患者无心力衰竭时NT-proBNP升高,而出现心力衰竭时NT-proBNP波动幅度较大,给NT-proBNP用于诊断此类患者心力衰竭,判断心功能分级带来困扰。本研究旨在观察NT-proBNP在老年MHD患者心力衰竭中的动态变化及与心功能分级的关系,探讨其在老年MHD并心力衰竭患者诊断及心功能分级评估中的应用价值。
1 对象与方法
1.1 对象 选择2010-01至2013-12因MHD合并心力衰竭住我院患者36例作为血透心衰组,男22例,女14例;年龄60~83岁,平均(70.44±6.51)岁;透析时间3~168个月。初始心力衰竭治疗时按美国纽约心脏病协会(New Youk Heart Association,NYHA)分级心功能为Ⅳ级。原发病:各种肾小球肾炎22例,糖尿病肾病6例,良性小动脉肾硬化3例,高血压肾损害5例。其中合并心房颤动6例,左室扩大16例,左室肥厚8例。血液透析均使用碳酸氢盐透析液,透析2~3次/周, 4 h/次,选用聚砜膜透析器(FreseniusF6HPS),面积1.3 m2,血流量180~240 ml/min,透析液流量500 ml/min。
选择同期住我院的非血液透析、CKD3期以上[eGFR>60 ml/(min·1.73m2)]的心力衰竭38例作为对照组,男23例,女15例,年龄60~80岁,平均(68.97±5.83)岁。初始心力衰竭治疗时心功能依据NYHA分级为Ⅳ级。原发病:冠心病26例,高血压性心脏病10例,扩张性心肌病2例。除外慢性阻塞性肺疾病、1个月内发生急性心肌梗死、急性脑血管意外、恶性肿瘤者。其中合并心房颤动5例,左室扩大14例,左室肥厚10例。两组年龄、性别、合并症、NYHA分级比较,差异无统计学意义。
1.2 血清NT-proBNP测定 两组于治疗开始前(心功能Ⅳ级)及治疗后心功能为Ⅲ、Ⅱ、Ⅰ级时分别抽取血样测定NT-proBNP,其中血透心衰组于透析前抽取血样。测定方法:采用电化学发光法,用E-601全自动免疫分析仪(RocheElecsys,美国)检测血清NT-proBNP,试剂由罗氏公司提供,NT-proBNP检测范围5~35 000 ng/L。
1.3 左心室肥厚的评估 两组治疗前行心脏超声检查,观察以下指标:左室EF值(LVEF);左室舒张末内径(LVEDD),男≥5.5 cm、女≥5.0 cm诊断为左室扩大[8];左室舒张末期室间隔厚度(IVST);左室舒张末期后壁厚度(LVPWT)。左室心肌质量(LVMM)按Devereux公式计算,LVMM(g)=1.04[(LVEDD+IVST+LVPWT)3-LVEDD3]-13.6[9]。体表面积(BSA)按Stevenson公式计算,BSA(m2)=0.0061×身高(cm)+0.0128×体质量(kg)-0.1529[10]。左室心肌质量指数[LVMMI(g/m2)]=LVMM/BSA,LVMMI≥125 g/m2(男), 120 g/m2(女)为左室肥厚[10]。
1.4 实验室检查 两组治疗前采血测定血常规、钾、钠、氯、血钙、磷、血红蛋白、血清肌酐、尿素氮、铁蛋白、血清白蛋白等。血透心衰组于透析前检测。

2 结 果
2.1 两组临床资料比较 两组患者年龄、性别比、左室扩大和左室肥厚以及心房颤动例数、体重指数、收缩压和舒张压、左室EF值、血钾、血钠、血氯、血钙、血尿酸、白蛋白水平均无统计学差异(P>0.05);血透心衰组与对照组比较,血红蛋白、肾小球滤过率(eGFR)水平明显降低,铁蛋白、血磷、血肌酐、尿素氮明显升高,两组比较差异有统计学意义(P<0.01)。见表1。
2.2 两组不同心功能分级间血清NT-proBNP水平比较 血透心衰组和对照组治疗后随心功能好转,血清NT-proBNP水平下降, 不同心功能分级间NT-proBNP水平有统计学差异(P<0.05或P<0.01)。血透心衰组各心功能分级NT-proBNP水平明显高于对照组,差异有统计学意义(P<0.05)。见表2。
2.3 ROC曲线诊断效能 血透心衰组不同心功能分级时AUC值、敏感度、特异度见表3,ROC曲线见图1、2。

表1 血透心衰组与对照组相关参数比较 ±s)
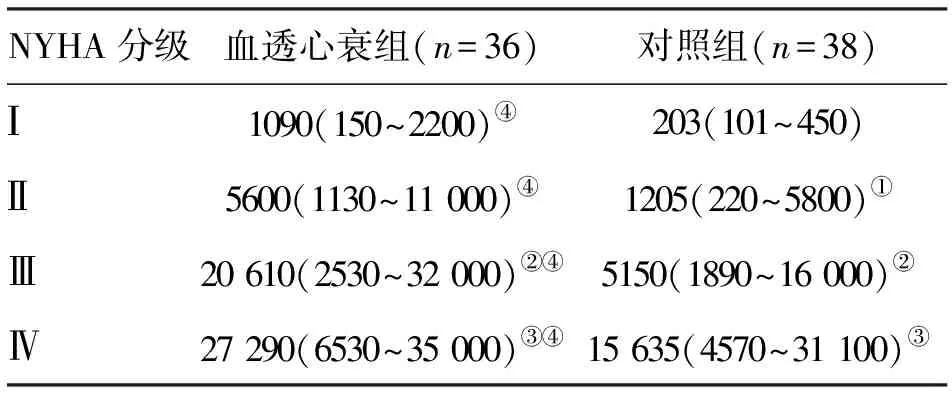
表2 血透心衰组及对照组不同NYHA分级间血清NT-proBNP比较 [ng/L;中位数(范围)]
注:与心功能Ⅰ级比较,①P<0.05;与心功能Ⅱ级比较,②P<0.01;与心功能Ⅲ级比较, ③P<0.05;与对照组比较, ④P<0.05

表3 ROC曲线对血透心衰组心力衰竭的诊断效能
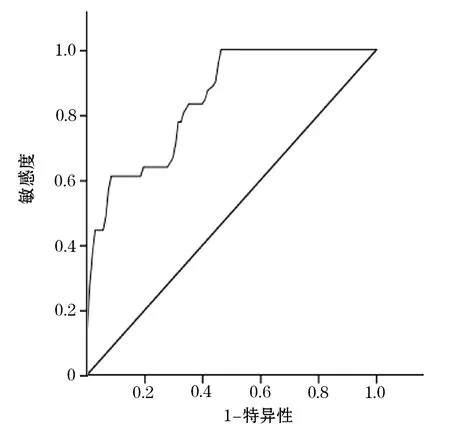
图1 血透心衰组NYHA Ⅳ级ROC曲线

图2 血透心衰组Ⅲ级ROC曲线
3 讨 论
NT-proBNP升高在慢性肾脏病患者中常见,心脏功能不全是NT-proBNP升高的主要因素[11,12]。NT-proBNP对MHD患者心血管事件发生率、病死率具有一定的预测价值[13]。而根据年龄制定NT-proBNP诊断心力衰竭的截点可以更好地提高NT-proBNP诊断的敏感度和特异度。本研究发现,血透心衰组各心功能分级的NP-proBNP值均较对照组明显升高,考虑是两组肾功能及血红蛋白差异影响所致[14]。随心功能改善,血透心衰组和对照组NP-proBNP水平均下降,其中血透心衰组心功能Ⅱ至Ⅳ级中,相邻分级间NP-proBNP值比较亦有统计学差异,提示在老年MHD合并心力衰竭时NP-proBNP值变化与心功能变化趋势一致,NP-proBNP值变化可以反映心功能变化程度[15]。但血透心衰组心功能Ⅰ级和Ⅱ级间NP-proBNP值无统计学差异,与已有研究认为该指标适用于轻、中度心力衰竭心功能分级诊断[16]的结论不同。另外,从ROC结果看到,AUC在两组心功能Ⅲ级和Ⅳ级时均达到0.7以上,说明其界值可以作为老年MHD合并心力衰竭患者心功能Ⅲ级和Ⅳ时的诊断及心功能分级指标,但在血透心衰组心功能Ⅰ级和Ⅱ级AUC值未达到有意义的诊断界值,提示NP-proBNP对老年MHD合并心力衰竭患者心功能Ⅰ级和Ⅱ级的诊断及心功能分级判别价值不大。其原因考虑是由于MHD患者肾功能减退,导致NT-proBNP从肾小球的滤过异常,加上本研究样本年龄偏高,合并心血管疾病、左室扩大、左室肥厚及心房颤动比例较高。另外,还有MHD患者少尿、无尿比例高导致透析间期心脏前负荷重,可使NP-proBNP在心力衰竭前即维持在较高水平[14]。这些因素都给NT-proBNP判断轻、中度心力衰竭时的心功能程度带来困难。
综上所述,老年MHD合并心力衰竭时,NT-proBNP可作为判断心力衰竭及心功能Ⅲ级、Ⅳ级的分级指标,对心功能Ⅰ级和Ⅱ级时诊断价值有限。
[1] Sudoh T,Kangawa K,Minamino N,etal.A new natriuretic peptide in porcine brain[J].Nature,1988,332(159):78-81.
[2] 汪 芳,李 卫,黄 洁,等.血浆N末端原脑利钠肽水平对慢性心力衰竭患者长期预后的预测价值[J].中华心血管病杂志,2006,34(1):28-32.
[3] Maisel A S,Krishnaswamy P,Nowak R M,etal.Rapid measurement of B-type natriuretic peptide in the emergency diagnosis of heart failure[J].N Eng J Med,2002,347(3):161-167.
[4] Austin W J,Bhalla V,Hernandez-Arce I,etal.Correlation and prognostic utility of B-type natriuretic peptide and its amino-terminal fragment in patients with chronic kidney disease[J].Am J Clin Pathol,2006,126(4):506-512.
[5] Van Kimmenade R R,Januzzi J L,Baggish A L,etal.Amino-terminal probrain natriuretic peptide,renal function,and outcomes in acute heart failure:redefining the cardiorenal interaction[J].J Am Coll Cardiol,2006,48(8):1621-1627.
[6] Tagore R,Ling L H,Yang H,etal.Natriuretic peptides in chronic kidney disease[J].Clin J Am Soc Nephrol,2008,3(6):1644-1651.
[7] Van Kimmenade R R,Januzzi J L,Bakker J A,etal.Renal clearance of B-type natriuretic peptide and amino terminal pro-B-type natriuretic peptide: a mechanistic study in hypertensive subjects[J].J Am Coll Cardiol,2009,53(10):884-890.
[8] 王新房.超声心动图学[M].3版.北京:人民卫生出版社,1999:311.
[9] Reichek N,Devereux R B.Left ventricular hypertrophy:Relationship of anatomic,echocardiographic and elecchocardiographic findings[J].Circulation,1981,63(6):1391-1398.
[10] Zhu Y,Zhang F,Zhang F C,etal.Risk factors elated to left ventricular hypertrophy in elderly hypertension patients[J].J Chin Clin Med,2006,13(6):308-313.
[11] Roberts M A,Hedley A J,Ierino F L.Understanding cardiac biomarkers in end-stage kidney disease: frequently asked questions and the promise of clinical application[J].Nephrology(Carlton),2011,16(3):251-260.
[12] Choi S Y,Lee J E,Jang E H,etal.Association between changesin N-terminal pro-brain natriuretic peptide 1evels and changes in left ventricular mass index in stable hemodialysis patients[J].Nephron clin Pract,2008,110(2):93-100.
[13] Madsen L H,ladefoged S,Corell P,etal.N-terminal pro brain natriuretic peptide predicts mortality in patients with end-stage renal disease in hemodialysis[J].Kidney Int,2007,71(6):548-554.
[14] Januzzi J L,Van K R,Lainchbury J,etal. NT-proBNP testing for diagnosis and short-term prognosis in acute destabilized heart failure: an international pooled analysis of 1256 patients: the International Collaborative of NT-proBNP Study[J].Eul-Heart J,2006,27(3):330-337.
[15] Weber T,Auer J,Eber B,etal.the diagnostic and prognostic value of brain natriuretic peptide and aminoterminal(nt)-pro brain natriuretic peptide[J].Curr Pharm Des,2005,11(4):511-525.
[16] Tsutamoto T,Sakai H,Nishiyama K,etal.Direct comparison of transcardiac increase in brain natriuretic peptide(BNP) and N-terminal proBNP and prognosis in patients with chronic heart failure[J].Circ J,2007,71(12):1873-1878.
(2014-01-06收稿 2014-03-09修回)
(责任编辑 尤伟杰)
Self-controlstudyofchangesinserumNT-proBNPonelderlyhemodialysisandnon-dialysispatientswithheartfailure
SUN Bo1, LIU Yuhua2, LI Sheng1, YAN Guoqiang1, SUN Yan1, CHEN Jie1, and WANG Yuee1. 1. No.2 Department of Internal Medicine, Hospital Attached to Aeromedicine Institute of PLA, Beijing100089, China; 2. Hemodialysis?Center of No.205 Hospital of PLA, Jinzhou 121001, China
ObjectiveTo evaluate the changes level of amino terminal brain natriuretic peptide(NT-proBNP) as well as its relationship between the changes and cardiac function classification in elderly maintenance hemodialysis patients with congestive heart failure.MethodsSelf-reflection methods was used to analyze clinical data in 36 maintenance hemodialysis patients with congestive heart failure (hemodialysis heart failure group)aged≥60 years and compared with 38 non-maintenance hemodialysis patients with congestive heart failure (control group)aged≥60 years whose estimated glomerular filtration rate (eGFR) >60 ml/(min·1.73 m2) more than 60 years old among the same period in this hospital. The NT-proBNP level of different grades classified by NYHA (New York Heart Association) in the two group’s patients was measured after the treatment to improve cardiac function. ROC curve was used to evaluate diagnosis efficiency of NT-proBNP in different cardiac function classification of hemodialysis heart failure group.ResultsIn hemodialysis heart failure group, compared with control group, NT-proBNP level of various cardiac function classification, median NT-proBNP values of Ⅰ, Ⅱ, Ⅲ, Ⅳ cardiac function classification respectively were significantly higher (P<0.05 orP<0.01). Comparing NT-proBNP level between different heart function classification in hemodialysis heart failure group, adjacent grading levels Ⅱ-Ⅳ also had significant difference (P<0.05 orP<0.01), and levels Ⅰ-Ⅱ have no significant difference (P>0.05). The same comparison in control group, adjacent grading levels Ⅰ-Ⅳ all have significant differences (P<0.05 orP<0.01). AUC value results in hemodialysis heart failure group: AUC value in grade Ⅳ was 0.847, NT-proBNP>11 100 ng/L as boundary values, sensitivity was 83%, specificity was 79%; AUC value in grade Ⅲ was 0.794, NT-proBNP> 6465 ng/L as boundary values, sensitivity was 100%, specificity was 56.4%; cardiac function classification Ⅰ, Ⅱ were meaningless.ConclusionsNT- proBNP can be regarded as diagnostic index and grading index of Ⅲ Ⅳ in elderly hemodialysis patients with congestive heart failure.
maintenance hemodialysis; N terminal-pro brain nalriuretic peptide; New York Heart Association; under receiver-operator characteristic curve
孙 波,硕士,副主任医师,E-mail:sunbo5526@sina.com
1.100089北京,解放军航空医学研究所附属医院内二科;2.121001锦州,解放军第205医院血液净化中心
R692.5
