主动脉夹层术后谵妄的临床特点和相关危险因素研究*
2014-07-12李晓晴马闻建姜霁纹
李晓晴 马闻建 姜霁纹 王 超 王 力 毕 齐
主动脉夹层术后谵妄的临床特点和相关危险因素研究*
李晓晴 马闻建 姜霁纹 王 超 王 力 毕 齐
目的 研究主动脉夹层术后谵妄的发生率和相关危险因素。方法对84例主动脉夹层术后患者采用意识错乱评估方法进行谵妄诊断,并结合临床资料分析术后谵妄的危险因素。结果主动脉夹层术后谵妄的发生率为33.3%。21例(75%)为一过性谵妄(<24h);7例(25%)为持续性谵妄。Logsistic多因素回归分析结果表明脑梗死、深低温停循环时间、重症监护病房持续时间是术后谵妄的危险因素。结论既往脑梗死、深低温停循环时间、重症监护病房持续时间是主动脉夹层患者术后谵妄的独立危险因素。
主动脉夹层 术后谵妄 发生率 危险因素
主动脉夹层(aortic dissection,AD)是病死率最高的心血管事件之一,该病起病急,进展快,病情凶险,24 h内病死率高达20%[1,2]。Stanford分类 A型主动脉夹层90 d的病死率更是高达70% ~90%[3,4],外科手术是最主要的治疗方法之一。随着主动脉外科手术、麻醉技术和医疗器械的日益成熟,术后病死率明显降低,但术后并发症仍然很常见,其中神经系统的并发症日益受到重视。术后谵妄(postoperative delirium,POD)是主动脉夹层术后常见的神经系统并发症之一。POD是在手术、麻醉后出现的急性、波动性认知功能障碍,以觉醒水平和认知功能紊乱为主要特点[5];POD延长住院时间[6],增加医疗费用,甚至增加术后病死率[7]。本研究拟对主动脉夹层术后谵妄的临床特点进行初步分析,探讨POD的相关危险因素,为制定有效预防措施提供依据。
1 对象与方法
1.1 对象 选取2013年1~12月北京安贞医院心外科主动脉夹层术后经神经科会诊的住院患者98例为研究对象。谵妄诊断标准:采用美国精神疾病诊断与统计手册第四版(DSM-IV)推荐的意识错乱评估方法(Confusion Assessment Method,CAM)作为谵妄评估诊断工具。根据DSM-IV制定的标准:(1)急性起病且病程波动;(2)注意力不集中;(3)思维紊乱;(4)意识水平改变。诊断谵妄要求具备特征(1)、(2)、(3)或者(1)、(2)、(4),即可诊断谵妄。排除标准:既往患有认知或精神系统疾病,酒精或者药物滥用,严重的视听障碍无法沟通,昏迷。84例患者符合纳入、排除标准,达到CAM诊断标准的POD患者共计28例,归为研究组;非谵妄患者56例归为对照组。
1.2 方法 将观察指标分为三大类,分别为术前因素(既往病史和一般资料),术中因素(手术过程),术后因素(术后监护室以及返回病房后)。术前因素包括年龄、性别、吸烟、饮酒、糖尿病、左室射血分数(Left Ventricular Ejection Fraction,LVEF)、高血压、房颤(Arterial Fibrillation,AF)、马凡氏综合征、脑梗死、脑出血、慢性阻塞性肺疾病 (ChronicObstructive Pulmonary Disease,COPD);术中因素包括手术时间、体外循环持续时间、主动脉阻断时间、选择性脑灌注时间、深低温停循环(deep hypothermic circulatory arrest,DHCA)时间;术后因素包括重症监护病房(Intensive Care Unit,ICU)持续时间、机械通气时间(Controlled Mechanical Ventilation,CMV)、平均动脉压、血氧饱和度(Arterial Oxygen Saturation,SaO2)、体温、心率、血红蛋白(hemoglobin,Hb)。
1.3 统计学方法 采用SPSS7.0统计学软件进行分析。计量资料采用±s表示,组间比较采用t检验;计数资料采用样本率或者构成比表示,组间比较采用χ2检验。危险因素分析采用多因素Logistic回归分析。P<0.05为差异有统计学意义。
2 结果
2.1 术后谵妄发生率和临床特点 主动脉夹层术后谵妄的发生率为33.3%。发生谵妄的28例患者中21例(75%)为一过性谵妄(<24 h);4例(14.3%)谵妄持续2 d;3例(10.7%)持续3~5 d。术后谵妄最常见的症状是精神运动性兴奋(82.1%),患者躁动,有拔出尿管、胃管的动作,需要约束制动;其次是睡眠-觉醒周期紊乱(75.0%),夜间失眠,白天嗜睡;多数患者表现有思维紊乱或者不连贯、定向力障碍、意识水平改变;精神运动性迟缓的患者为之甚少,只有 1例(3.6%)。见表1。
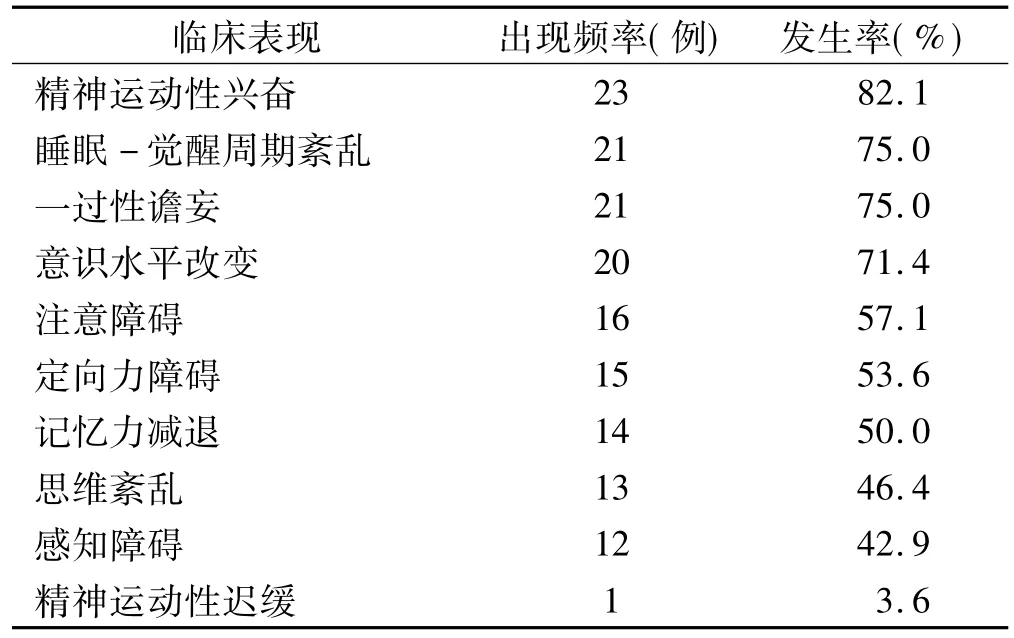
表1 术后谵妄的临床表现
2.2 术后谵妄的单因素分析结果 将两组患者围手术期指标分为三大类型,分别为术前、术中和术后危险因素,并对这三大类指标进行单因素分析。与谵妄发生有关的术前危险因素包括LVEF≤30%、脑梗死;术中危险因素包括手术持续时间、DHCA时间;术后危险因素包括机械通气时间、血氧饱和度、ICU持续时间,上述各因素对术后谵妄的影响有统计学意义(P<0.05)。见表2、3、4。
2.3 术后谵妄的多因素分析结果 多因素Logistic逐步回归分析结果显示,与术后谵妄发生有关的因素包括脑梗死、DHCA时间、ICU持续时间(AdjR2=0.874,F=32.14,P=0.00)。见表5。
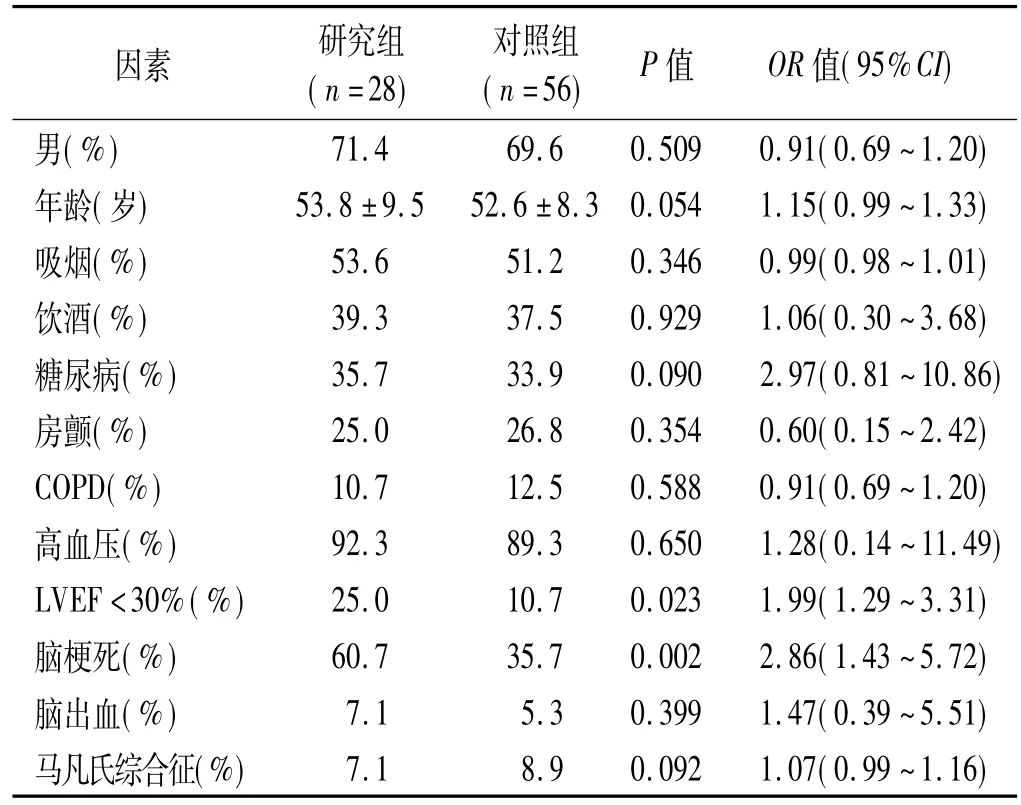
表2 谵妄的术前危险因素分析
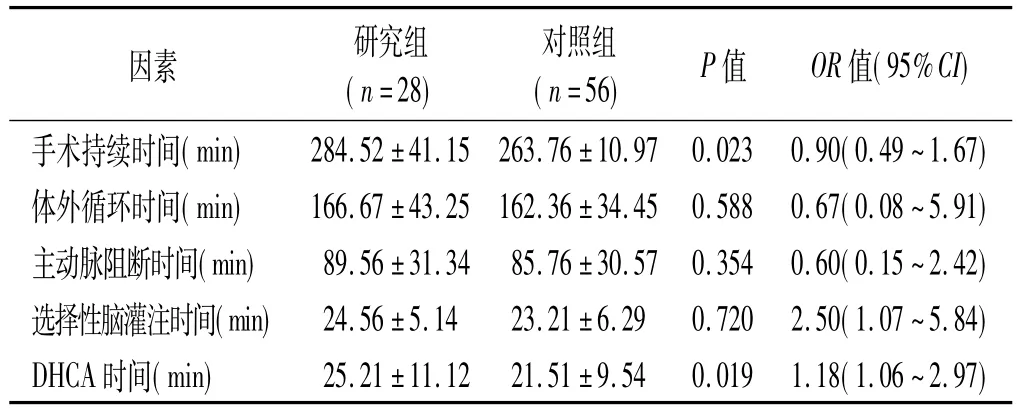
表3 谵妄的术中危险因素分析
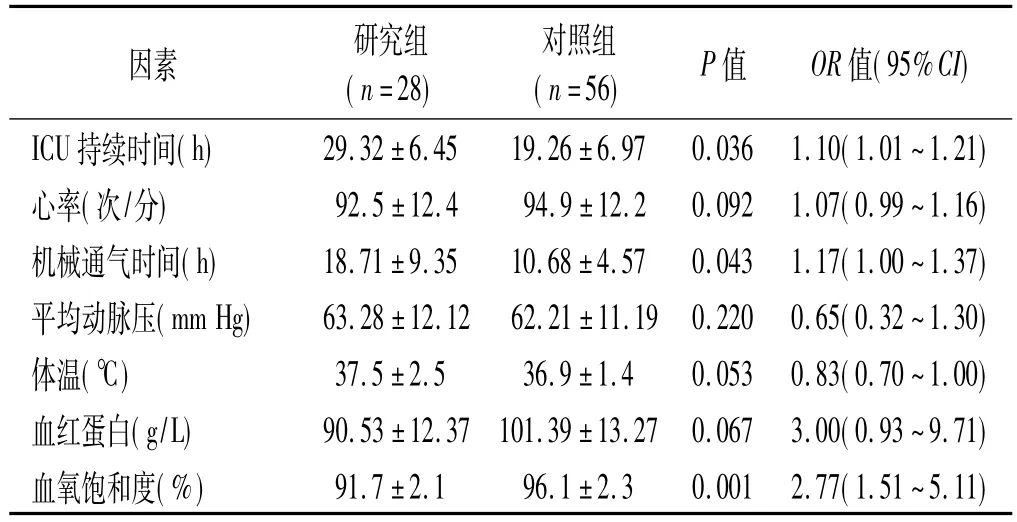
表4 谵妄的术后危险因素分析
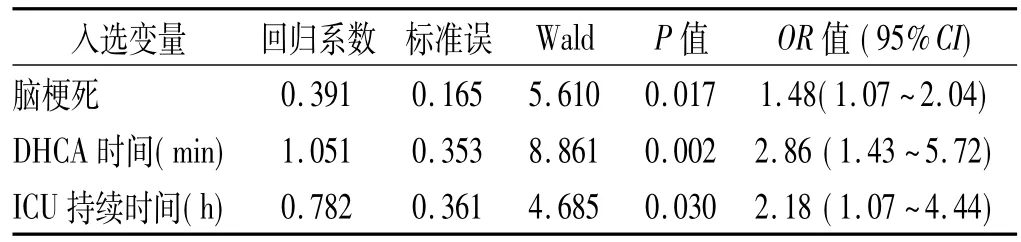
表5 术后谵妄的Logsistic多因素回归分析结果
3 讨论
随着外科手术和麻醉技术的日益改进和提高,主动脉夹层术后病死率显著降低;如何减少术后神经系统并发症逐渐成为研究热点[8~10]。谵妄是主动脉夹层术后神经系统并发症之一,发生率为 12% ~37%[11],与预后不良相关[12]。在本研究中,术后谵妄的发生率为33.3%,与国外研究一致;但我们的研究对象仅包括术后请神经科会诊的患者,样本规模小,故主动脉夹层术后谵妄的发生率有待进一步深入研究。
本次研究结果显示,既往脑梗死、术中DHCA时间以及ICU持续时间与谵妄发生相关,故术后谵妄是由围手术期的多种因素共同促发所致。
Fleck TM等[13]学者研究发现DHCA时间是主动脉夹层术后发生谵妄的最重要的预测因子。Immer FF等[14]亦发现DHCA延长会严重降低患者术后的中期生活质量(mid-term quality of life)。尽管低温能显著降低代谢,发挥保护作用,但动物实验显示[15],体温即使降至20℃时,脑组织仍保留20%的正常代谢水平;即使体温降至 18℃亦只能提供不完全的脑保护(incomplete cerebral protection),因此,低温持续时间越长,脑损伤的可能性越大。本研究结果显示DHCA时间与术后谵妄发生密切相关,与国外研究结果相一致。
本次研究结果提示脑梗死是发生术后谵妄的危险因素之一。术后谵妄的发生与亚临床微栓塞和全脑灌注不良有关[16,17]。在脑血管硬化狭窄的基础上,微栓子导致脑组织缺血缺氧进而引起神经功能障碍[18~20]。微栓子有多种类型,如气泡、血栓、脱落的钙化斑块等,产生栓子负荷进而导致脑损伤可能是发生谵妄的重要机制[21,22]。脑梗死提示脑组织受损,中枢神经系统易损性增加,特别是皮层下多发梗死灶使得神经环路受损,进而发生执行功能和认知障碍以及谵妄。
国外研究显示,谵妄与ICU时间延长相关[23];在ICU的特殊环境下,谵妄的发生率高达70%~80%甚至更高[24]。ICU内常有肢体约束、留置导尿甚至睡眠剥夺,故重症监护环境易导致谵妄[25],本次研究结果亦证实ICU持续时间是术后谵妄发生的独立危险因素。
综上所述,谵妄是主动脉夹层术后常见的并发症,既往有脑梗死的患者更易发生,缩短术中DHCA时间,减少不必要的ICU治疗时间,可能对减少术后谵妄的发生有一定的作用。
[1] Nienaber CA,Eagle KA.Aortic dissection:new frontiers in diagnosisand management: PartI: from etiology to diagnostic strategies[J].Circulation,2003,108(5):628-635
[2] Mehta RH,Suzuki T,Hagan PG,et al.International Registry of Acute Aortic Dissection(IRAD)Investigators.Predicting death in patients with acute type A aortic dissection[J]. Circulation,2002,105(2):200-206
[3] Myrmel T,Lai DT,Miller DC.Can the principles of evidence-based medicine be applied to the treatment of aortic dissections?[J].Eur J Cardiothorac Surg,2004,25:236–245
[4] Chan SH,Liu PY,Lin LJ,et al.Predictors of inhospital mortality in patients with acute aortic dissection[J].Int J Cardiol,2005,105:267–273
[5] Inouye SK.Delirium in older persons[J].N Engl J Med,2006,354:1157–1165
[6] Franco K,Litaker D,Locala J,et al.The cost of delirium in the surgical patient[J].Psychosomatics,2001,42:68–73
[7] Rudolph JL,Jones RN,Rasmussen LS,et al.Independent vascular and cognitive risk factors for postoperative delirium[J].Am J Med,2007,120:807–813
[8] Nakamura K,Onitsuka T,Yano M,et al.Predictor of neurologic dysfunction after elective thoracic aorta repair using selective cerebral perfusion[J].Scand Cardiovasc, 2005,39:96-101
[9] Ehrlich MP,Ergin MA,McCullough JN,et al.Predictors of adverse outcome and transient neurological dysfunction after ascending aorta/hemiarch replacement[J].Ann Thorac Surg,2000,69:1755-1763
[10] Ergin MA,Galla JD,Lansman L,et al.Hypothermic circulatory arrest in operations on the thoracic aorta.Determinants of operative mortality and neurological outcome[J].J Thorac Cardiovasc Surg,1994,107:788-797
[11] Zierer A,Moon MR,Melby SJ,et al.Impact of perfusion strategy on neurologic recovery in acute type A aortic dissection[J].Ann Thorac Surg,2007,83:2122-2129
[12] Girard TD,Pandharipande PP,Ely EW.Delirium in the intensive care unit[J].Crit Care,2008,12:S3-S8
[13] Fleck TM,Czerny M,Hutschala D,et al.The incidence of transient neurologic dysfunction after ascending aortic replacement with circulatory arrest[J].Ann Thorac Surg,2003,76(4):1198-1202
[14] Immer FF,Lippeck C,Barmettler H,et al.Improvement of Quality of Life After Surgery on the Thoracic Aorta Effect of Antegrade Cerebral Perfusion and Short Duration of Deep Hypothermic Circulatory Arrest[J].Circulation,2004,110(11):Ⅱ250-255
[15] Ehrlich MP,McCullough JN,Zhang N,et al.Effect of hypothermia on cerebral blood flow and metabolism in the pig[J].Ann Thorac Surg,2002,73:191-197
[16] Gaul C,Dietrich W,Friedrich I,et al.Neurological symptoms in type A aortic dissections[J].Stroke,2007,38(2):292-297
[17] Estrera AL,Garami Z,Miller CC,et al.Cerebral monitoring with transcranial Doppler ultrasonography improves neurologic outcome during repairs of acute type A aortic dissection[J]. J Thorac Cardiovasc Surg,2005,129(2):277-285
[18] Whitaker D,Motallebzadeh R.Intraoperative cerebral highintensity transientsignals and postoperative cognitive function:a systematic review[J].Am J Surg,2009,198: 295-297
[19] Selnes OA,Goldsborough MA,Borowicz LM,et al.Determinants of cognitive change after coronary artery bypass surgery:a multifactorial problem[J].Ann Thorac Surg,1999,67: 1669-1676
[20] Bokeriia LA,Golukhova EZ,Polunina AG.Postoperative delirium in cardiac operations:microembolic load is an important factor[J].Ann Thorac Surg,2009,88:349-350
[21] Blauth CI.Macroemboli and microemboli during cardiopulmonary bypass[J].Ann Thorac Surg,1995,59:1300-1303
[22] Tagarakis GI,Karangelis D,Tsolaki F,et al.Embolism as major cause of neurocognitive complications after heart surgery[J].Interact Cardiovasc Thorac Surg,2011,12: 383
[23] Lat I,McMillian W,Taylor S,et al.The impact of delirium on clinical outcomes in mechanically ventilated surgical and trauma patients[J].Crit Care Med,2009,37: 1898-1905
[24] McNicoll L,Pisani MA,Zhang Y,et al.Delirium in the intensive care unit:occurrence and clinical course in older patients[J].J Am Geriatr Soc,2003,51:591-598
[25] Whitlock EL,Vannucci A,Avidan MS.Postoperative delirium[J].Minerva Anestesiol,2011,77:448-456
Clinical characteristics and risk factors of postoperative delirium in patients with aortic dissection
.
LI Xiaoqing,MA Wenjian,JIANG Jiwen,et al.
Capital Medical University Affiliated Beijing Anzhen Hospital,Beijing 100029,China
Objective To study the incidence rate and risk factors of postoperative delirium in patients with aortic dissection.Methods84 patients after aortic dissection surgery were evaluated with Confusion Assessment Method(CAM)to make the diagnosis of postoperative delirium.Patients’clinical informations were analyzed to detect the risk factors of postoperative delirium.ResultsThe incidence rate of postoperative delirium was 33.3%in patients after aortic dissection surgery,in which 21 cases(75%)were transient delirium and 7 cases(25%)were persistent delirium.Logistic multifactor stepwise regression analysis indicated that the risk factors of postoperative delirium included history of brain infarction,deep hypothermic circulatory arrest(DHCA)time and ICU stay time.ConclusionPrevious brain infarction,DHCA time and ICU stay time are independent risk factors of postoperative delirium in patients with aortic dissection.
Aortic dissection Postoperative delirium Incidence rate Risk factors
R749.2
A
1009-7201(2014)-03-0175-03
10.3969/j.issn.1009-7201.2014.03.005
2014-03-18)
国家自然科学基金项目(编号:30800350)
100029,首都医科大学附属北京安贞医院
李晓晴(1978~),女,河北张家口人,博士,主治医师,研究方向:神经病学
毕齐,E-mail:anzhenneurologist@126.com
