肺门作为躯干重心对强直性脊柱炎胸腰段后凸畸形矫形的意义
2014-02-14张永刚李杰静唐翔宇张国营郑国权张雪松毛克亚
宋 凯 张永刚 李杰静 余 文 唐翔宇 张国营 郑国权 崔 赓 张雪松 毛克亚 王 征 王 岩
. 强直性脊柱炎 Ankylosing spondylitis .
肺门作为躯干重心对强直性脊柱炎胸腰段后凸畸形矫形的意义
宋 凯 张永刚 李杰静 余 文 唐翔宇 张国营 郑国权 崔 赓 张雪松 毛克亚 王 征 王 岩
目的探索能够代表强直性脊柱炎 ( ankylosing spondylitis,AS ) 胸腰段后凸畸形躯干重心的影像学标记,进而设计 AS 胸腰段后凸畸形的截骨矫形方案。方法不规则物体的重心可通过两个不同方向的悬吊或支撑力线获得,通过手术前后髋轴的支撑力线可寻找 AS 胸腰段后凸畸形患者的躯干重心。38 例无脊髓神经症状体征、双髋活动良好的 AS 胸腰段后凸畸形患者纳入研究。比较 AS 矫形患者手术前后矢状面平衡距离 ( sagittal vertical axis,SVA )、C7距髋轴中心水平距离 ( horizontal distance between hip axis and C7,HDHC )、T5距髋轴中心水平距离 ( horizontal distance between hip axis and T5,HDHT5)、T9距髋轴中水平距离 ( horizontal distance between hip axis and T9,HDHT9)、肺门距髋轴中心水平距离 ( horizontal distance between hip axis and hilus pulmonis,HDHH ),将矫形前后测量值做统计描述及配对 t 检验。采用组内相关系数 ( ICC ) 衡量 HDHH 的观察者间信度 ( inter-observer reliability ) 及观察者内复测信度 ( intra-observer reliability )。结果矫形前 SVA、HDHC、HDHT5、HDHT9、HDHH 分别为 21.1 cm、12.7 cm、3.5 cm、-3.8 cm、2.7 cm;矫形后分别为 9.1 cm、4.2 cm、-2.1 cm、-5.6 cm、0.9 cm。SVA、HDHC、HDHT5、HDHT9矫形前后变化有统计学意义,HDHH 矫形前后变化无统计学意义。HDHH 的观察者间总体信度与观察者内总体复测信度分别为 0.958、0.963 ( P<0.001 )。结论矫形前后肺门垂线通常总是落在髋轴上,肺门可作为躯干重心的影像学标记应用于 AS 胸腰段后凸畸形的矫形设计。
脊柱炎,强直性;椎体后凸成形术;肺门;矫形外科手术;胸椎;腰椎
健康人群自然站立时,躯干重心落在髋轴上,此时骨盆处于中立位[1-4]。强直性脊柱炎 ( ankylosing spondylitis,AS ) 患者晚期易伴发僵硬固定的胸腰段后凸畸形,会导致患者躯干重心病理性前置,落在髋轴前方。此时,躯干在矢状面上失平衡。由于AS 后凸患者脊柱强直失去代偿能力,为重新取得平衡及最小的能量消耗,患者只能通过伸髋、屈膝,进而代偿性后旋骨盆,试图将躯干重心再次落在髋轴上 ,最终达到相对的平衡状态[5-12]。因此,患者的骨盆旋转状态其实由躯干重心的位置变化决定,而躯干重心恢复至正常位置可确保矫形后骨盆中立位。
然而,人体躯干结构复杂,在矢状面上,骨骼、肌肉、内脏等组织分布并不对称。因此,寻找躯干重心的影像学标记并不容易。目前,国内外相关研究虽然证实 C7垂线并非重力线,但却未能给出躯干重心的影像学标记[1-2,6,12]。本部分利用简单的物理学原理,通过分析矫形前后不同影像学标记距离髋轴的水平距离,寻找并探讨能够代表 AS 后凸患者躯干重心的较好的影像学标记,并应用于截骨矫形的手术设计。
资料与方法
一、一般资料
2004 年 1 月至 2010 年 3 月,收治的 38 例无脊髓神经症状体征、双髋活动良好的 AS 胸腰段后凸畸形患者。男 24 例,女 14 例;最小年龄 22 岁,最大年龄 57 岁,平均年龄 35 岁。
自然站立位拍摄外观像及全脊柱侧位 X 线像,测量矫形前后患者的矢状面平衡距离 ( sagittal vertical axis,SVA )、C7距髋轴中心水平距离 ( horizontal distance between hip axis and C7,HDHC )、T5距髋轴中心水平距离 ( horizontal distance between hip axis and T5,HDHT5)、T9距髋轴中水平距离 ( horizontal distance between hip axis and T9,HDHT9)、肺门距髋轴中心水平距离 ( horizontal distance between hip axis and hilus pulmonis,HDHH ) ( 图 1a )。
肺门侧位像上主要由四部分组成:左主支气管、中间支气管、右肺动脉、左肺动脉。一般情况下,肺门各部分结构清晰可见 ( 图 1b、c ),尤其是左主支气管,一卵圆形高透亮影,一般位于肺门中心,也位于肺野中央。即便在胸廓形状发生变化时,此影像学标志位置仍然相对固定[13-14]。本研究将左主支气管作为肺门中心测量 HDHH。
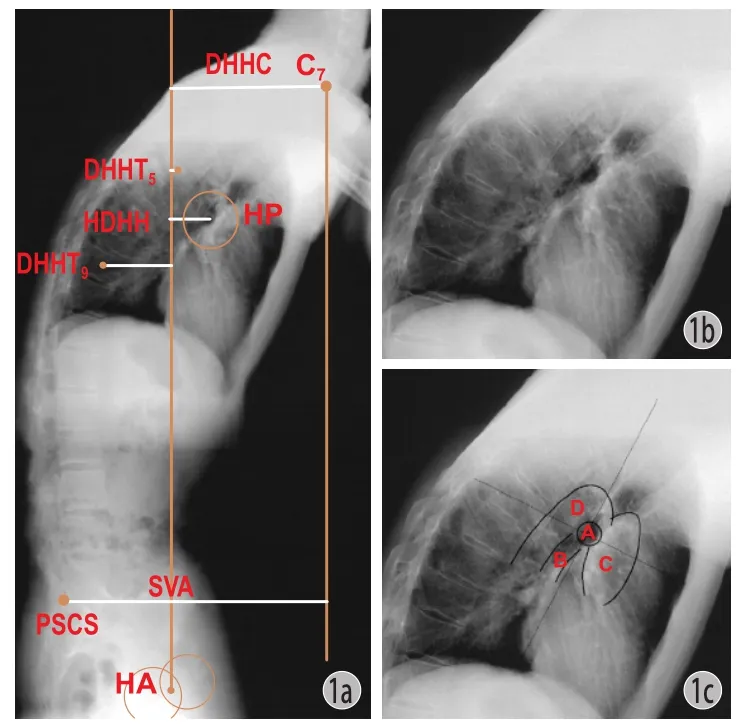
图1 a:全脊柱侧位像 HA,髋轴;PSCS,骶骨后上角;HP,肺门;DHHC,C7距髋轴水平距离;DHHT5,T5距髋轴水平距离;HDHH,肺门距髋轴水平距离;DHHT9,T9距髋轴水平距离;SVA,矢状面平衡距离,C7距骶骨后上角水平距离。b:肺门侧位像大体观。c:肺门侧位像:A 左主支气管;B 中间支气管;C 右肺及叶间动脉;D 左肺动脉Fig.1 a: Lateral view of the whole spine. HA: hip axis; PSCS: Posterior superior corner of S1; HP: Hilus pulmonis; HDHC: Horizontal distance between hip axis and C7; HDHT5: Horizontal distance between hip axis and T5; HDHH: Horizontal distance between hip axis and hilus pulmonis; HDHT9: Horizontal distance between hip axis and T9; SVA: Sagittal vertical axis, or horizontal distance between the C7vertical line and the posterior superior corner of S1. b: Close-up view of the lateral hilus pulmonis. c: Lateral view of the hilus pulmonis; A Left main bronchus; B Bronchus intermedius; C Right pulmonary artery and interlobar artery; D Left pulmonary artery
二、手术方法
行后路经椎弓根单节段 ( L12 例,L214 例,L38 例 ) 或双节段 ( T12与 L11 例,T12与 L23 例,T12与L32 例,L1与 L38 例 ) 楔形闭合截骨矫形椎弓根螺钉内固定术。
三、统计学分析
将矫形前后测量值做统计描述及配对 t 检验。采用组内相关系数 ( ICC ) 衡量 HDHH 的观察者间信度 ( inter-observer reliability ) 及观察者内复测信度( intra-observer reliability )。使用 SPSS 16.0 统计学软件 ( SPSS 公司,美国 ),以 P<0.05 为差异有统计学意义。
结 果
矫形前 SVA、HDHC、HDHT5、HDHT9、HDHH 分别为 21.1 cm、12.7 cm、3.5 cm、-3.8 cm、2.7 cm;矫形后分别为 9.1 cm、4.2 cm、-2.1 cm、-5.6 cm、0.9 cm。SVA、HDHC、HDHT5、HDHT9矫形前后均有统计学意义,HDHH 矫形前后无统计学意义 ( 表 1 )。
表1 矫形前后影像学参数统计描述及配对 t 检验 ( n=38,±s )Tab.1 Statistical description and paired t-test results of the preoperative and postoperative radiological parameters ( n=38,±s )
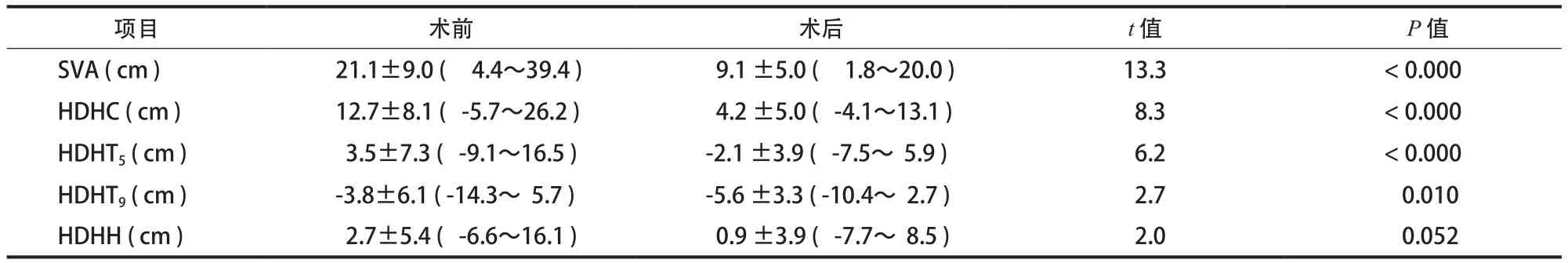
表1 矫形前后影像学参数统计描述及配对 t 检验 ( n=38,±s )Tab.1 Statistical description and paired t-test results of the preoperative and postoperative radiological parameters ( n=38,±s )
注:SVA:矢状面平衡距离,HDHC:C7距髋轴中心水平距离,HDHT5:T5距髋轴中心水平距离,HDHT9:T9距髋轴中水平距离,HDHH:肺门距髋轴中心水平距离Notice: SVA: Sagittal vertical axis; HDHC: Horizontal distance between hip axis and C7; HDHT5: Horizontal distance between hip axis and T5; HDHT9: Horizontal distance between hip axis and T9; HDHH: Horizontal distance between hip axis and hilus pulmonis
项目 术前 术后 t 值 P 值SVA ( cm ) 21.1±9.0 ( 4.4~39.4 ) 9.1 ±5.0 ( 1.8~20.0 ) 13.3 < 0.000 HDHC ( cm ) 12.7±8.1 ( -5.7~26.2 ) 4.2 ±5.0 ( -4.1~13.1 ) 8.3 < 0.000 HDHT5( cm ) 3.5±7.3 ( -9.1~16.5 ) -2.1 ±3.9 ( -7.5~ 5.9 ) 6.2 < 0.000 HDHT9( cm ) -3.8±6.1 ( -14.3~ 5.7 ) -5.6 ±3.3 ( -10.4~ 2.7 ) 2.7 0.010 HDHH ( cm ) 2.7±5.4 ( -6.6~16.1 ) 0.9 ±3.9 ( -7.7~ 8.5 ) 2.0 0.052
HDHH 的总体观察者间总体信度与观察者内总体复测信度分别为 0.958、0.963,P<0.001。观察者中,笔者得出最大的复测信度 ( ICC=0.993,P<0.001 ),而一非专业者得到最低的复测信度 ( ICC=0.932,P<0.001 )。
讨 论
一、躯干重心的位置与骨盆旋转的关系
健康成人自然站立位时,躯干重心落在髋轴中点上,而骶骨岬恰好也落在髋轴中点上[3,15],躯干重心、骶骨岬、髋轴中点三点共线。我们可以将髋轴中点与骶骨岬的连线称作为骨盆中立位线 ( pelvic neutral position line,PNP-line ),其位置状态直接反映骨盆的旋转情况。正常情况下,躯干重心在 PNP-line 上,而 PNP-line 也因此垂直地面,这个时候骨盆处于中立位状态。
对矢状面失衡的脊柱畸形患者而言,其躯干重心相对位置变化 ( 重心偏离 PNP-line,落在其前方或后方 ),但机体为再次获得躯干平衡并节约能量消耗,骨盆会向相反的方向旋转代偿,仍然试图将躯干重心落在髋轴中心之上。于是,骶骨岬会落在髋轴中心的前方或后方,而 PNP-line 则不再垂直地面,我们可以将 PNP-line 的垂线角 ( 也就是骶骨岬与髋轴中点连线的垂线角 ) 作为骨盆的旋转角度( pelvic rotation angle,PRA )。
AS 后凸畸形患者骨盆处于后旋状态,当矫形程度不同时,骨盆的旋转状态不同,可以通过躯干重心与 PNP-line ( 骶骨岬与髋轴连线 ) 的关系确定( 图 2 )。
由此可以看出,AS 胸腰段后凸畸形矢状面失平衡的实质就是:躯干重心偏离了骨盆中立位线。而矢状位平衡重建的目标为:通过截骨矫形,将躯干重心重置于骨盆中立位线上。
二、躯干重心的影像学标记
人体躯干形状、结构复杂,在矢状面上,骨骼、肌肉、内脏等组织分布并非不对称,如何寻找躯干重心点?力学原理告诉我们,对于不规则物体,可以通过悬吊法或支撑法寻找重心。基于此,我们将可以将髋轴作为支点,通过矫形前后的两条支撑线交点确定重心 ( 图 3a、b )。
但是,同时应当指出,矫形前后的躯干形状并不恒定。不过,如果我们以截骨节段将躯干分为近端、远端两部分。远端躯干质量远远大于近端躯干质量,而且,远端躯干相对髋轴的力臂同样远远大于近端躯干[16]。通过力学、几何学分析,我们可以近似的将远端躯干的重心点看作整体躯干的重心点。而远端躯干的形态及质量密度分布并无明显变化 ( 图 3c、d )。
结果显示,矫形前后肺门垂线落在近髋轴上。因此,可将肺门作躯干重心的影像学标记。而矫形前肺门垂线落在髋轴稍前则说明患者骨盆后旋肌群及腰背肌群的张力作用与重心偏于髋轴支点的抵消现象。
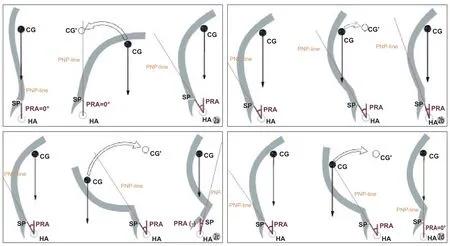
图2 矫形程度与骨盆旋态示意图 a:代偿机制 ( 1 ) 正常脊柱序列,重心落在髋轴上,PNP-line 垂直地面,骨盆位于中立位;( 2 ) AS胸腰段后凸畸形,骨盆中立位时,重心远离 PNP-line,落在髋轴前方,此状态不稳定;( 3 ) 为将重心再次落于髋轴上,骨盆后旋至旋后位,PNP-line 向后倾斜。b:矫形不足 ( 1 ) AS 后凸畸形,重心于 PNP-line 前方,骨盆位于旋后位;( 2 ) 矫形后,躯干重心后移,落在髋轴后方,但仍在 PNP-line 前方,此状态不稳定。( 3 ) 为将重心再次落于髋轴上,骨盆前旋,PNP-line 后倾程度减小,骨盆仍位于旋后位。c:矫形过度 ( 1 ) AS 后凸畸形,重心于 PNP-line 前方,骨盆位于旋后位;( 2 ) 矫形后,躯干重心后移,远远落在髋轴后方,并落在PNP-line 后方,此状态不稳定;( 3 ) 为将重心再次落于髋轴上,骨盆前旋,PNP-line 前倾,骨盆位于旋前位。d:矫形恰当 ( 1 ) AS 后凸畸形,重心于 PNP-line 前方,骨盆位于旋后位;( 2 ) 矫形后,躯干重心后移,落在髋轴后,但恰将重心重置于 PNP-line 上,即重心、骶骨岬、髋轴三点共线,此状态不稳定;( 3 ) 为将重心再次落于髋轴上,骨盆前旋,PNP-line 再次垂直地面,骶骨岬恰落在髋轴上,骨盆位于中立位Fig.2 Diagram of correction degree and pelvic rotation a: Compensatory mechanism. ( 1 ) For a healthy adult, CG fell on HA. Pelvic neutral position line ( PNP-line ) was vertical to the ground, and the pelvis was located in neutral position; ( 2 ) In the patients with AS TLK, CG was anterior to HA and far from PNP-line when the pelvis was in neutral position. It was not a stable state; ( 3 ) In order to make CG fall on HA again, the pelvis was rotated backward and PNP-line tilted backwards. b: Insufficient pedicle subtraction osteotomy ( PSO ) angle. ( 1 ) Before the operation, CG was anterior to PNP-line and the pelvis was in supination position; ( 2 ) After PSO, CG was behind HA but still anterior to PNP-line, and it was not a stable state; ( 3 ) In order to make CG fall on HA again, the pelvis was rotated forward but still in supination position and the retroversion degree of PNP-line became less. c: Excess PSO angle. ( 1 ) Before the operation, CG was anterior to PNP-line and the pelvis was in backward rotation; ( 2 ) After PSO, CG was far behind HA and posterior to PNP-line. It was not a stable state; ( 3 ) In order to make CG fall on HA again, the pelvis was rotated forward but still in pronation position and PNP-line tilted forwards. d: Adequate PSO angle. ( 1 ) Before the operation, CG was anterior to PNP-line, and the pelvis was in backward rotation; ( 2 ) After PSO, CG was behind HA, and on PNP-line again. The 3 points of CG, sacral promontory ( SP ) and HA was on the same line. It was not a stable state; ( 3 ) In order to make CG fall on HA again, the pelvis was rotated forward and located in neutral position, with PNP-line vertical to the ground again and SP on HA
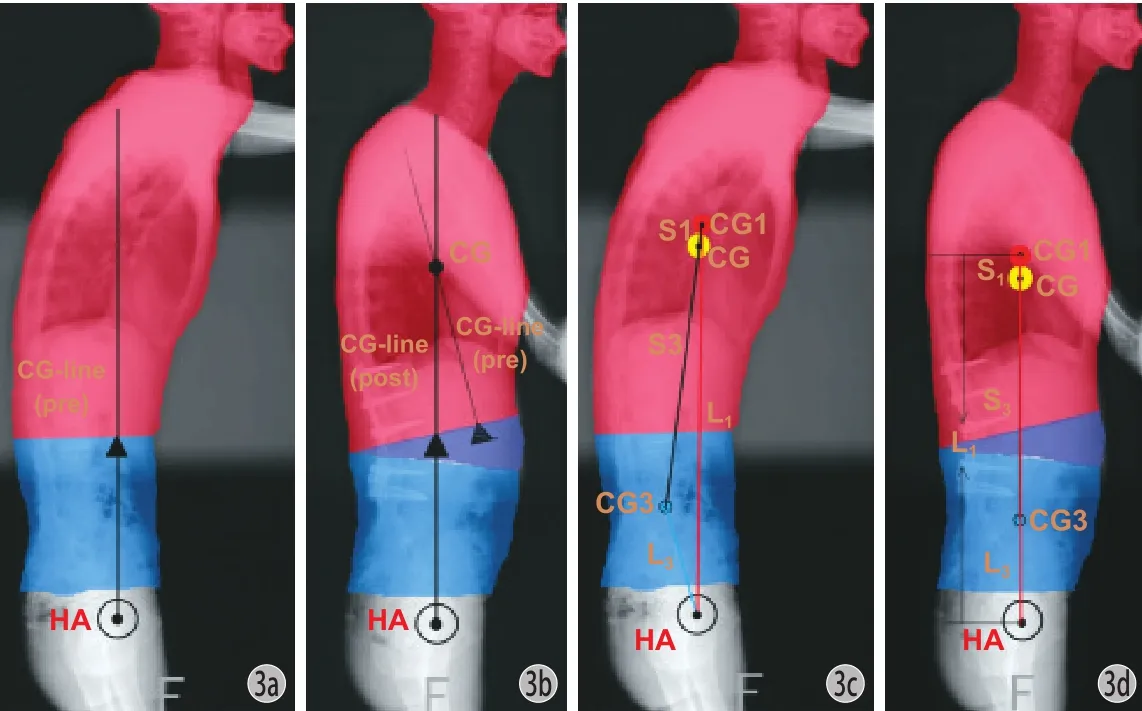
图3 寻找重心示意图 ( HA,髋轴中点;CG,整体躯干重心;CG1,远端躯干重心;CG3,近端躯干重心;L1,远端躯干力臂;L3,近端躯干力臂;S1,CG与 CG1 间距离;S3,CG 与 CG3 间距离 ) a:矫形前髋轴支撑线;b:矫形后髋轴支撑线,交点可近似认为是远端躯干重心;c~d:矫形前后 CG1 > CG3,L1>L3,故 CG1 × L1>> CG3 × L3,而 S1/ S3= CG3 × L3/ CG1 × L1,故 S1<< S3。也就是说,远端躯干重心位置非常接近整体躯干重心位置,因此可通过寻找远端躯干重心来定位整体躯干重心Fig.3 Diagram of CG ( HA: Hip axis; CG: Center of gravity of the entire trunk; CG1: Center of gravity of the proximal part of the trunk; CG3: Center of gravity of the distal part of the trunk; L1: Distal end of the arm of force of the trunk; L3: Primary end of the arm of force of the trunk; S1: Distance between CG and CG1; S3: Distance between CG and CG3 ) a: Preoperative HA vertical line; b: Postoperative HA vertical line. The crossing point of the preoperative and postoperative vertical lines could be taken as CG3; c-d: Before and after the correction. CG1>CG3 and L1>L3, so CG1×L1>>CG3×L3. However, S1/S3=CG3×L3/CG1×L1, so S1<<S3. CG3 was far away from CG, so CG could be found once CG3 was confirmed
此外,本研究结果还提示:一般情况下,对 AS胸腰段后凸畸形,C7总是位于躯干重心之前 ( 术前12.7 cm,术后 4.2 cm ),其相对骶骨后上角更为靠前 ( 术前 SVA=21.1 cm,术后 SVA=9.1 cm ),传统的矫形方案试图将 C7重置于骶骨后上角 ( 即 SVA=0 cm ) 其实是一个不可能实现的任务,Van Royen在其矫形设计中将 SVA 设定为 7.5 cm,其实在另一个方面同样说明了 SVA=0 cm 的不可能性[5-6]。T5矫形前位于重心之前 ( 3.5 cm ),矫形后位于重心后方 ( -2.1 cm )。T9总是位于躯干重心之后 ( 术前-3.8 cm,术后 -5.6 cm )。
三、矢状面平衡的截骨矫形设计
既然肺门可以近似的看作重心的影像学标记,当以骶骨岬与髋轴作为骨盆中立位线时 ( PNP-line )作为骨盆中立位标准时,肺门、骶骨岬、髋轴三点共线可保证矫形后骨盆中立位 ( 图 4 )。
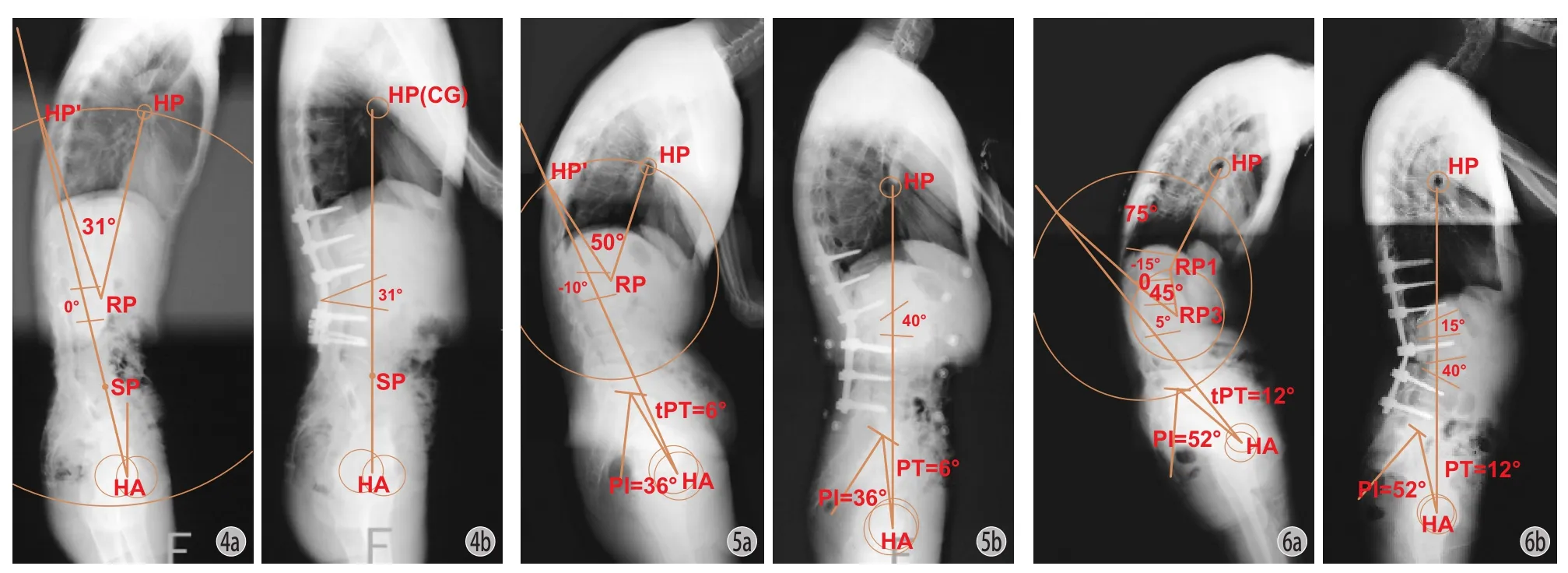
图4 截骨设计示意图 ( HA,髋轴中点;SP,骶骨岬;HP,肺门;RP,截骨椎体前缘闭合点 ) a:连接 HA、SP 并做延长线 ( PNP-line ),以 RP 为圆心,RP-HP 为半径作圆,交 HA-SP 与 HP’。∠ HP-RP-HP’ = 32° 即为设计截骨角度;b:L3截骨 31°,术后骶骨岬再次落在髋轴上,PNP-line 垂直地面,骨盆处于中立位图 5 单节段截骨设计实例 a:( 1 ) 测量术前 PI = 36°,则 tPT = 0.37 × PI-7 = 0.37 × 36-7 = 6°,通过理论 PT 做出直线 HA-HP’,我们将此线作为该患者骨盆中立位线;( 2 ) 选择 L2作为截骨节段,将椎体皮质前缘闭合点标记为 RP,并作为圆心,RP-HP 为半径作圆交骨盆中立位线于 HP’,也就是将肺门位置重置于骨盆中立位线上,则∠ HP-RP-HP’ = 50° 即为设计截骨角度。b:L2取得 40° + ( -10° ) = 50°的截骨角度,矫形后自然站立位实际 PT = 6°,骨盆处于中立位图 6 双节段截骨设计实例 a:( 1 ) 测量术前 PI = 52°,则 tPT = 0.37 × PI-7 = 0.37 × 52-7 = 12°,通过理论 PT 做直线 HA-HP’,我们将此线作为该患者骨盆中立位线。( 2 ) 选择 L1、L3作为截骨节段,将椎体皮质前缘闭合点分别标记为 RP1、RP3。以 RP3 为圆心,RP1-RP3为半径作圆,于圆周上取一点 O,∠ O-RP3-RP1 = 45☒ ( 自选角度 ) 即为 L3设计截骨角度;以 O 为圆心,RP1-HP 为半径作圆交骨盆中立位线 于 HP’,将肺门位置再次重置于骨盆中立位线上。∠ HP’-O-RP1-HP- ∠ O-RP3-RP1 = 75°-45° = 30° 为 L1截骨角度。b:L1取得15° + ( -15° ) =30° 的截骨角度,L3取得 40° + ( -5° ) = 45° 的截骨角度,矫形后患者自然站立位实际 PT = 12°,骨盆处于中立位Fig.4 Osteotomy design. ( HA: Hip axis; SP: Sacral promontory; HP: Hilus pulmonis; RP: Rotation point of the middle point at the front edge of PSO vertebra ) a: A straight line was deawn through SP and HA ( PNP-line ), and a circle was made with RP as the center and RP-HP as the radius. And then HP’ was the intersection with SP-HA. Theoretical osteotomy angle=∠HP’-RP-HP=31°; b: After a PSO=31°, CG and SP were on HA. PNP-line was vertical to the ground, and the pelvis was in neural positionFig.5 Personalized single-segment osteotomy design a: First, the preoperative PI was measured as 36°, and then tPT=0.37×PI-7=0.37×36-7=6°. Second, the theoretic PT was used to locate exact pelvic neutral positional line ( HA-HP’ ). Third, RP was marked, and a circle was made with RP as the center and RP-HP as the radius. At last, HP’ was the intersection with SP-HA. In conclusion, theoretical osteotomy angle=∠HP’-RP-HP=50°; b: After a PSO=40° ( postoperative lordosis ) +10° ( preoperative kyphosis ) =50°, the postoperative PT=6° and individual pelvic neutral positon was reconstructed successfullyFig.6 Personalized double-segment osteotomy design ( nunchuck design ) a: First, the preoperative PI was measured as 52°, and then tPT=0.37×PI-7=0.37×52-7=12°. Second, the theoretic PT was used to locate exact pelvic neutral positional line ( HA-HP’ ). Third, rotation point at L3: the middle point at the front edge of PSO vertebra ( RP3 ) and rotation point at L1: the middle point at the front edge of PSO vertebra ( RP1 ) were marked, and a circle was made with RP3 as the center and RP3-RP1 as the radius. And then, a little was made on the circle and marked as O, by which the osteotomy angle for L3was decided. Next, another circle was made with O as the center and RP1-HP as the radius. HP’ was the intersection with SP-HA. Theoretical osteotomy angle for L3=∠O-RP3-RP1=45°. Theoretical osteotomy angle for L1=∠HP’-O-RP1-HP-∠O-RP3-RP1=75°-45°=30°; b: After a PSO angle in L3of 45° ( 40° postoperative lordosis+5° preoperative kyphosis ), and a PSO angle in L1of 30° ( 15° postoperative lordosis+15° preoperative kyphosis ), for a total of 75°, the postoperative PT=12°, and individual pelvic neutral positon was reconstructed successfully
传统的骨盆中立位标准多采取固定的骨盆倾斜角,骶骨倾斜角或者骶骨岬恰好落在髋轴上等,因此并不个性化[3,5-6]。近年来众多研究证实了骨盆参数之间相关性,并通过骨盆形态学参数 ( PI,pelvic incidence,骨盆入射角 ) 预测骨盆体位性参数 ( PT,pelvic tilt,骨盆倾斜角 ),从而可使不同个体骨盆中立位的标准更为合理、科学[17-19]。手术设计方案:( 1 ) 通过 PI 预测理论 PT ( tPT=0.37×PI-7 )[19];( 2 )将肺门重置于 tPT ( theoretic PT,理论 PT ) 的骨盆中立位线上 ( 图 5,6 )。
四、颌眉角的纠正 ( 图 7 )
AS 胸腰段后凸畸形的矫形目标除了恢复脊柱-骨盆的矢状面失衡外,最为关键的即矫正其颌眉角( chin-brow vertical angle,CBVA )。Suk 教授等认为,对于颈椎强直的 AS 患者,CBVA 在 -10°~10°时最为合理,但在标准的伸髋伸膝位测量颌眉角的方法,并不合理,因为 AS 后凸患者髋关节本身已处于过伸状态[20]。因此,合理的颌眉角测量方式应为“自然站立位”,而其骨盆中立位时颌眉角则需要通过 X 线侧位片追加骨盆后旋的角度“PT-tPT”,即:骨盆中立位时颌眉角=外观照自然站立位颌眉角+X 线自然站立位 PT-tPT[21]。多数情况下,纠正颌眉角的理论截骨角度与重建矢状面的理论截骨角度并不相同,基于截骨方法的几何原理,我们可以调整截骨节段,当颌眉角纠正角度大于重建矢状面平衡角度时,我们可以将截骨节段向头端调整,反之则向尾端调整截骨节段[5,11]。术前评估患者颈椎屈伸活动度可为设计截骨角度提供了更大的可选择空间。另外,截骨设计时应当考虑患者职业,手术预期等因素,最终在矢状面重建及颌眉角纠正间找到一个最优平衡点。具体的介绍及设计方案我们将在专门文献中详细阐述。
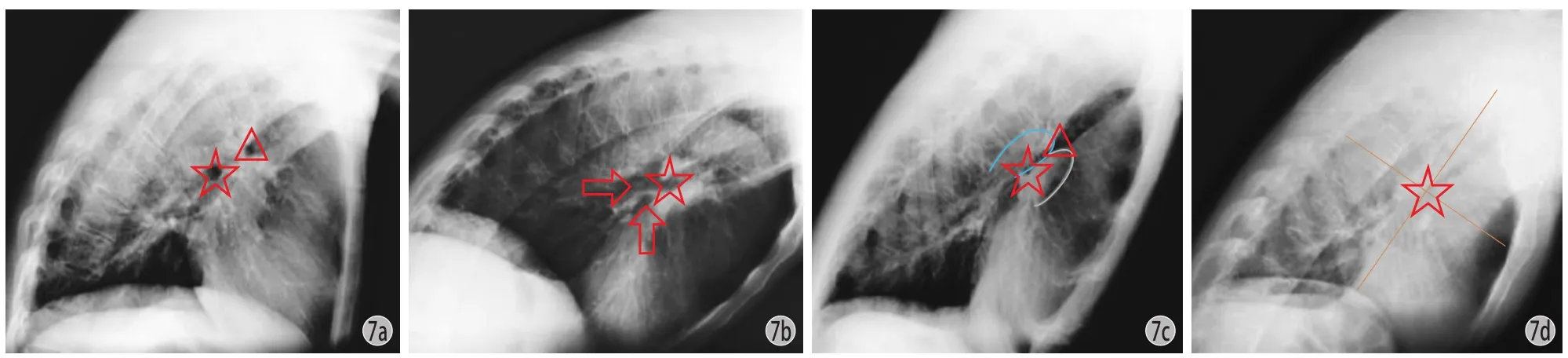
图7 胸部 X 线侧位片 a:左主支气管,右侧支气管;b:左主支气管,左支气管分支;c:蓝色轮廓,左肺动脉;灰色轮廓,右肺及间叶动脉;左主支气管,右主支气管;d:近似当作左主支气管,即肺门中心Fig.7 Lateral X-rays of the cervical vertebra a: Left main bronchus (); Right upper lobe bronchial orifice (). b: Left main bronchus ( asterisk ); Bronchus (). c: Left main bronchus (); Left pulmonary artery ( blue outline ); Right pulmonary artery and interlobar artery ( gray outline ). d: Left main bronchus () was supposed in the middle of the lung
五、本研究的不足
肺门由四部分组成:左主支气管、中间支气管、右肺动脉、左肺动脉。本研究将左主支气管作为肺门中心,一般情况下,肺门各部分结构清晰可见,而左主支气管为一卵圆形高透亮影,位于肺门中心,也位于肺野中央。即便在胸廓形状发生变化时,此影像学标志位置仍然相对固定[13-14]。本研究的信度分析同样证明了该影像学标志的可靠性 ( 观察者间总体信度,ICC=0.958;观察者内总体复测信度,ICC=0.963 )。
即便如此,在测量过程中,由于 X 线曝光情况的不确定性,在部分 X 线片上,寻找肺门依然是一个相对困难的事情。笔者之一作为研究者,经验相对丰富,得出最大的复测信度 ( ICC=0.993 ),而一非专业者得到最低的复测信度 ( ICC=0.932 )。因此,经验同样成为更好寻找肺门的影响因素之一。图 7 介绍了几个容易误读的肺门图片:a:示两个软圆形透亮影,上面一个为右主支气管 ( 三角形 ),而下方为左主支气管 ( 五角星 ) ,其更为接近肺野中央。b:中两个更为透亮的区域 ( 箭头 ) 是支气管分支而非左主支气管,左主支气管 ( 五角星 ) 在其上方并发出支气管分支,其同样更靠近肺野中央。c:很难鉴别左主支气管 ( 五角星 ),但左右肺动脉影相对清晰 ( 蓝色及灰色轮廓 ),可根据其相对位置寻找左主支气管。d:曝光显影不清,在此状态下,连接肺尖及肺底中点,连接肺前后壁中点,通过两线交点近似确定肺野中心,将此点作为左主支气管位置( 五角星 ),此法最为无奈但却最为简单方便。
本研究证明肺门近似为 AS 胸腰段后凸畸形的躯干重心,是通过多样本统计后所得,绝非严格意义上的重心替代影像学标记,因此,在个案中,我们常发现,肺门垂线并未落在髋轴上方,而是或前或后。这与 SVA 评定矢状面平衡类似,个案中的极少能能够见到 C7恰落在骶骨后上角上。本研究所有入组患者均为双髋活动良好患者,因此能够在最大程度上代偿后凸畸形,如将双髋强直患者入组,则可能得出不一样的结论。同样,对于存在侧凸的患者,由于双肺冠状面上的倾斜及严重不对称性,肺门也很难被扩大应用。受限于实验条件,本研究未能做更为深入的力学测试,因此也同样遗憾。
综上所述,AS 胸腰段后凸畸形矫形前后,自然站立位时,肺门垂线落在近髋轴上,因此可将肺门作为躯干重心的影像学标记应用于矫形设计。
[1]Schwab F, Lafage V, Boyce R, et al. Gravity line analysis in adult volunteers: age-related correlation with spinal parameters,pelvic parameters, and foot position. Spine, 2006, 31(25): E959-967.
[2]Legaye J, Duval-Beaupere G. Gravitational forces and sagittal shape of the spine. Clinical estimation of their relations. Int Orthop, 2008, 32(6):809-816.
[3]Chang KW, Leng X, Zhao W, et al. Quality control of reconstructed sagittal balance for sagittal imbalance. Spine, 2011, 36(3):E186-197.
[4]Bridwell KH, Lewis SJ, Lenke LG, et al. Pedicle subtraction osteotomy for the treatment of fixed sagittal imbalance. J Bone Joint Surg (Am), 2003, 85-A(3):454-463.
[5]van Royen BJ, Gast AD, Smit TH. Deformity planning for sagittal plane corrective osteotomies of the spine in ankylosing spondylitis. Eur Spine J, 2000, 9(6):492-498.
[6]van Royen BJ, Scheerder FJ, Jansen E, et al. ASKyphoplan: a program for deformity planning in ankylosing spondylitis. Eur Spine J, 2007, 16(9):1445-1449.
[7]Debarge R, Demey G, Roussouly P. Radiological analysis of ankylosing spondylitis patients with severe kyphosis before and after pedicle subtraction osteotomy. Eur Spine J, 2010, 19(1):65-70.
[8]Bridwell KH, Lewis SJ, Rinella A, et al. Pedicle subtraction osteotomy for the treatment of fixed sagittal imbalance. Surgical technique. J Bone Joint Surg (Am), 2004, 86-A(Suppl 1): 44-50.
[9]Le Huec JC, Leijssen P, Duarte M, et al. Thoracolumbar imbalance analysis for osteotomy planification using a new method: FBI technique. Eur Spine J, 2011, 20(Suppl 5): 669-680.
[10]宋凯, 张永刚, 郑国权. 强直性脊柱炎后凸畸形矫形前后生活质量与影像学参数分析. 中华骨科杂志, 2012, 32(5): 404-408.
[11]宋凯, 张永刚, 郑国权, 等. 强直性脊柱炎胸腰段后凸畸形矫形前后影像学参数分析. 脊柱外科杂志, 2012, 10(2):93-96.
[12]Roussouly P, Gollogly S, Noseda O, et al. The vertical projection of the sum of the ground reactive forces of a standing patient is not the same as the C7 plumb line: a radiographic study of the sagittal alignment of 153 asymptomatic volunteers. Spine, 2006, 31(11):E320-325.
[13]Feigin DS. Lateral chest radiograph a systematic approach. Acad Radiol, 2010, 17(12):1560-1566.
[14]McComb BL. The chest in profile. J Thorac Imag, 2002, 17(1):58-69.
[15]Takemitsu Y, Harada Y, Iwahava T, et al. Lumbar degenerative kyphosis. Clinical, radiological and epidemiological studies. Spine, 1988, 13(11):1317-1326.
[16]Clin J, Aubin CE, Lalonde N, et al. A new method to include the gravitational forces in a finite element model of the scoliotic spine. Med Biol Eng Comput, 2011, 49(8):967-977.
[17]Legaye J, Duval-Beaupere G, Hecquet J, et al. Pelvic incidence: a fundamental pelvic parameter for three-dimensional regulation of spinal sagittal curves. Eur Spine J, 1998, 7(2): 99-103.
[18]Vaz G, Roussouly P, Berthonnaud E, et al. Sagittal morphology and equilibrium of pelvis and spine. Eur Spine J, 2002, 11(1): 80-87.
[19]Vialle R, Levassor N, Rillardon L, et al. Radiographic analysis of the sagittal alignment and balance of the spine in asymptomatic subjects. J Bone Joint Surg (Am), 2005, 87(2): 260-267.
[20]Suk KS, Kim KT, Lee SH, et al. Significance of chinbrow vertical angle in correction of kyphotic deformity of ankylosing spondylitis patients. Spine, 2003, 28(17):2001-2005.
[21]Song K, Zheng G, Zhang Y, et al. A new method for calculating the exact angle required for spinal osteotomy. Spine, 2013, 38(10):E616-620.
( 本文编辑:王永刚 )
Signifcance of the hilus pulmonis as the center of gravity of the trunk for deformity correction in thoracolumbar kyphosis secondary to ankylosing spondylitis
SONG Kai, ZHANG Yong-gang, LI Jie-jing, YU Wen, TANG Xiangyu, ZHANG Guo-ying, ZHENG Guo-quan, CUI Geng, ZHANG Xue-song, MAO Ke-ya, WANG Zheng, WANG Yan. Department of Orthopedics, Chinese PLA General Hospital, Beijing, 100853, PRC
ObjectiveTo investigate a radiological marker for the center of gravity ( CG ) of the trunk in the treatment of thoracolumbar kyphosis ( TLK ) secondary to ankylosing spondylitis ( AS ), so as to design deformity planning.MethodsThe CG of an irregular object could be obtained through hanging or supporting it in 2 different directions or points, and the CG of the trunk in the patients with AS TLK would be located by using the preoprative and postoperative hip axis vertical lines. A total of 38 patients with AS TLK were included in this study, who had good hips and no spinal cord injuries. The preoperarive and postoperative radiological parameters were measured, including sagittal vertical axis ( SVA ), horizontal distance between hip axis and C7( HDHC ), horizontal distance between hip axis and T5( HDHT5), horizontal distance between hip axis and T9( HDHT9) and horizontal distance between hip axis and hilus pulmonis ( HDHH ). The preoperative and postoperative measurement results were compared by statistical analysis and paired t-tests. The intraclass correlation coeffcient ( ICC ) was used to determine the intraobserver and interobserver reliabilities of HDHH.ResultsThe preoperative SVA, HDHC, HDHT5, HDHT9and HDHH values were 21.1 cm, 12.7 cm, 3.5 cm, -3.8 cm and 2.7 cm respectively, and the postoperative values were 9.1 cm, 4.2 cm, -2.1 cm, -5.6 cm and 0.9 cm respectively. The differences between the preoprative and postoperative values of SVA, HDHC, HDHT5and HDHT9were statistically significant, and while the differences between the preoprative and postoperative values of HDHH were not. The ICC for overall interobserver reliability was 0.958, and it was 0.963 for overall intraobserver reliability ( P<0.001 ).ConclusionsThe hilus pulmonis falls approximately on the hip axis bothpreoperatively and postoperatively. It is a better radiological marker for the CG of the trunk for deformity planning in AS TLK.
Spondylitis, ankylosing; Kyphoplasty; Hilus pulmonis; Orthopedic procedures; Thoracic vertebrae; Lumbar vertebrae
10.3969/j.issn.2095-252X.2014.10.008
R681.5, R682.3
100853 北京,解放军总医院骨科
张永刚,Email: zhangyg301@hotmail.com
2014-07-17 )
