Recurrent Seizures Manifestations in a Case of Congenital Hypoparathyroidism:a Case Report
2013-11-18ShengyuWangWeiWuandXuanMa
Sheng-yu Wang*,Wei Wu,and Xuan Ma
Internal Medicine Department,Affiliated Hospital of Xi’an Medical University,Xi’an 710077,China
HYPOPARATHYROIDISM is characterized by hypocalcemia,hyperphosphatemia and low or inappropriately normal levels of parathyroid hormone (PTH).PTH is a key calcium regulating hormone essential for calcium homeostasis,vitamin D-dependent calcium absorption,renal calcium reabsorption and renal phosphate clearance.Hypoparathyroidism may be due to congenital or acquired disorders.Causes include autoimmune diseases,genetic abnormalities,destruction or infiltrative disorders of the parathyroid glands.The most common cause of hypoparathyroidism is iatrogenic in the setting of anterior neck surgery.We present a case of recurrent hypocalcemic seizures due to congenital hypoparathyroidism.
CASE DESCRIPTION
A 20-year-old female presented to us with a history of generalized tonic clonic seizures of 20-minute duration.Her father said she had episodes of seizures with a frequency of four to five times a month since she was 12 years of age.There was no history of head trauma in childhood.Detailed treatment history was not available.After seizures were controlled with anticonvulsants,the general physical examination revealed normal vitals,mild pallor.Carpopedal spasm was present and other signs of latent tetany such as Chovstek's sign and Trousseau's sign were present.Cardiovascular system and respiratory system examinations were normal.Central nervous system examination revealed moderate mental retardation in higher function testing.
Investigations revealed a normal hemogram.Random blood glucose level was normal.Serum Na+and K+levels were normal;serum calcium level was 1.3 mmol/L (normal reference range 2.1-2.6 mmol/L),serum Mg2+0.78 mmol/L(normal reference range 0.7-1.1 mmol/L),serum phosphorus 1.79 mmol/L (normal reference range 0.80-1.45 mmol/L);serum PTH level 8.66 pg/ml (normal reference range 15-24 pg/ml).The corrected QT interval on the electrocardiogram was 0.47 seconds.Brain computed tomography (CT)revealed extensive intraparenchymal calcifications (Fig.1).
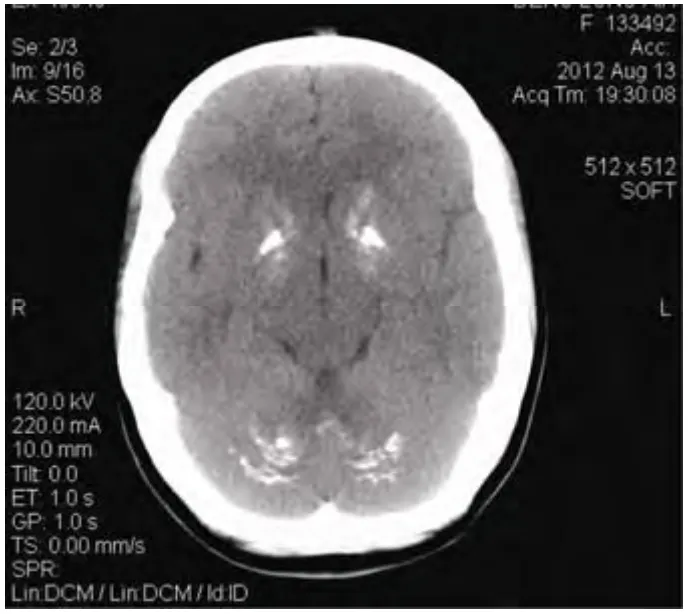
Figure 1.Computed tomography scan demonstrating extensive basal ganglia calcification.
Adiagnosis of congenital/hereditary hypoparathyroidism was made.The patient was treated with anticonvulsants,oral calcium 1 g/d and vitamin D 1 mg/d.During the hospital stay of 5 days,she had three attacks of seizures with documented hypocalcemia.After 3 months of follow-up,frequency of seizures was slightly decreased (three attacks)and evidence of latent tetany was absent.
DISCUSSION
Hypoparathyroidism is decreased function of the parathyroid glands with under production of PTH.This can lead to low levels of calcium in the blood,often causing cramping and twitching of muscles or tetany (involuntary muscle contraction),and several other symptoms.The condition can be inherited,but it is also encountered after thyroid or parathyroid gland surgery,and it can be caused by immune system-related damage as well as a number of rarer causes.
Acquired hypoparathyroidism is usually due to inadvertent removal of parathyroid gland during neck surgeries for hyperthyroidism,or it can result due to removal of too much parathyroid gland during surgery for hyperparathyroidism.1Other rare causes of acquired hypoparathyroidism include radiation induced damage subsequent to radio iodine therapy,sarcoidosis,haemochromatosis,haemosiderosis,Wilson's disease and metastatic infiltration of parathyroid gland.1,2
Laboratory evaluation to diagnose hypoparathyroidism should include serum calcium (total as well as ionized),phosphorous,serum albumin,creatinine,magnesium,intact PTH and 25-hydroxyvitamin D levels.2Serum calcium levels are low,phosphate levels are high and intact PTH level are inappropriately low in hypoparathyroidism.Patients with pseudohypoparathyroidism also have low calcium,high phosphorus but high PTH levels.2Measurement of 25-hydroxyvitamin D levels is important to rule out vitamin D deficiency as a cause of hypocalcemia.Measurement of magnesium is also important as magnesium depletion or excess can also cause hypocalcaemia by inducing functional hypoparathyroidism.3Hypoparathyroidism was diagnosed in our patient on the basis of low serum calcium (ionized and total),high phosphate and very low PTH levels in face of normal magnesium levels.
Electroencephalogram in the presence of hypocalcemia can show evolution from alpha through theta and delta dominance,generalized spikes and sharp-waves burst of delta activity with sharp components.4Unfortunately,facility of electroencephalogram was not available at our center.
Radiological features of hypoparathyroidism include intracranial calcification most commonly involving bilateral basal ganglia.5Calcification can also occur in the cerebellum,subcortical white matter,corona radiata and thalamus.
Intracranial calcification can also be physiological in 0.3%-1.5% of subjects.6Most common pathological causes of basal ganglia calcification are hypoparathyroidism and pseudohypoparathyroidism.Other causes of basal ganglia calcification are Fahr's syndrome,tuberous sclerosis,Cockayne's syndrome,mitochondrial disease,familial idiopathic basal ganglia calcification,diffuse neurofibrillary tangles with calcification,Down's syndrome and post-infectious.
For most of the patients,vitamin D in a dose of 40 000-120 000 U/d (1-3 mg/d) with elemental calcium in a dose of ≥ 1 gm/d are usually satisfactory.1Oral calcium and vitamin D restore the overall calcium-phosphate balance but do not reverse hypercalcuria seen in hypoparathyroidism,therefore after vitamin D and calcium replacement excessive urinary calcium excretion can lead to kidney stone formation.Thiazides diuretics can lower urinary calcium excretion in such patients.1
Long-term treatment of hypoparathyroidism is with vitamin D analogs and calcium supplementation may be ineffective in some due to potential renal damage.7The N-terminal fragment of PTH (PTH 1-34) has full biological activity.The use of pump delivery of synthetic PTH 1-34 provides the closest approach to physiologic PTH replacement therapy.8Teriparatide,a recombinant form of PTH (presently registered for osteoporosis) might become the treatment of choice for PTH supplementation.9Currently,hypoparathyroidism is the only hormonal insufficiency state that does not have a hormone-replacement-therapy approved,but research is being conducted to establish recombinant human PTH (1-84) (rhPTH [1-84]) as just such a replacement.
1.Potts JT.Diseases of the parathyroid gland and other hyper and hypocalcemic disorders.In:Fauci AS,Braunwald E,Kasper DL,et al,editors.Harrison's principles of internal medicine.17th ed.New York:McGraw Hills;2008.p.2377-96.
2.Shoback D.Clinical practice.Hypoparathyroidism.N Engl J Med 2008;359:391-403.
3.Tong GM,Rude RK.Magnesium deficiency in critical illness.J Intensive Care Med 2005;20:3-17.
4.Castilla-Guerra L,del Carmen Fernández-Moreno M,López-Chozas JM,et al.Electrolytes disturbances and seizures.Epilepsia 2006;47:1990-8.
5.Fulop M,Zeifer B.Case report:Extensive brain calcification in hypoparathyroidism.Am J Med Sci 1991;302:292-5.
6.Verulashvili IV,Glonti LSH,Miminoshvili DK,et al.Basal ganglia calcification:Clinical manifestations and diagnostic evaluation.Georgian Med News 2006;140:39-43.
7.Winer KK,Yanovski JA,Cutler GB Jr.Synthetic human parathyroid hormone 1-34vs.calcitriol and calcium in the treatment of hypoparathyroidism:Results of a randomized crossover trial.JAMA 1996;276:631-6.
8.Winer KK,Zhang B,Shrader J,et al.Synthetic human parathyroid hormone 1-34 replacement therapy:A randomized crossover trial comparing pumpversusinjections in the treatment of chronic hypoparathyroidism.J Clin Endocrinol Metab 2012;97:391-9.
9.Winer KK,Ko CW,Reynolds JC,et al.Long-term treatment of hypoparathyroidism:A randomized controlled study comparing parathyroid hormone-(1-34)versuscalcitriol and calcium.J Clin Endocrinol Metab 2003;88:4214-20.
杂志排行
Chinese Medical Sciences Journal的其它文章
- Primary Endodermal Sinus Tumor in the Posterior Cranial Fossa:Clinical Analysis of 7 Cases
- Coronary Artery Perforation Complicated With Acute Aortic Valve Regurgitation During Percutaneous Coronary Intervention:Report of Two Cases
- CORRECTION
- Mechanical Stimulus Inhibits the Growth of a Bone Tissue Model Cultured In Vitro△
- What Moved into the Lung? An Unusual Case of Foreign Body Migration
- Reconstruction of the Medial Patellofemoral Ligament Using Hamstring Tendon Graft With Different Methods: a Biomechanical Study
