Reconstruction of the Medial Patellofemoral Ligament Using Hamstring Tendon Graft With Different Methods: a Biomechanical Study
2013-04-20WeiHeYumingYangMingLiuAiyuanWangandYujieLiu
Wei He, Yu-ming Yang, Ming Liu, Ai-yuan Wang, and Yu-jie Liu*
1Department of Orthopedics, The 305 Hospital of Chinese People’s Liberation Army, Beijing 100017, China
2Department of Orthopedics, The 261 Hospital of Chinese People’s Liberation Army, Beijing 100094, China
3Department of Orthopedics, General Hospital of Chinese People’s Liberation Army, Beijing 100853, China
PATELLAR dislocation or subluxation is a common injury in young adults, and it is easy to cause cartilage damage, associated with complicated patellofemoral arthritis. The deeper study on the normal anatomy of medial patellofemoral ligament (MPFL) is help for clearer understanding the mechanism of the patellar lateral displacement and outward dislocation caused by MPFL injury. How to reconstruct the anatomy of MPFL and restore the stability of the patellofemoral joint is the focus of recent studies. There are many surgical procedures for MPFL reconstruction, such as tendon transposition operation, repair enhancing surgery, tendon graft reconstruction,1-6and so on. The previous study of our group demonstrated good clinical effects using the tendon graft sutured on the medial patella to reconstruct MPFL. For the biomechanical purpose, we compared the tensile strength of the normal MPFL and the hamstring tendon graft on the patella with different fixation methods in this study, in order to assess the clinical reliability of the four-suture method.
MATERIALS AND METHODS
MPFL specimens
Eight fresh frozen normal cadaver knees from donors were used in this study. All specimens were stored at -20˚C and thawed at room temperature 24 hours before use. The incision was made in the lateral knee joint. The femoral quadriceps, the patellar tendon and other tissues were removed to allow the MPFL to be exposed, which is located deep to the retinaculum of the medial patella. The proximal edge of the MPFL inserts into the undersurface of the vastus medialis obliquus, and the distal edge can be identified by palpation and transillumination (Fig. 1). The MPFL was next detached from the surrounding tissue, being the only connection between the patella and femoral entocondyle. Then the specimens were wrapped by the wet gauze and carefully preserved.
Model reconstruction
The MPFL was reconstructed with the hamstring tendon graft using three methods of the patella fixation. The reconstruction points were located in the medial edge of the patella. The medial hamstring tendon was preconditioned by 20 N, stretched for 15 minutes, and then sutured at the reconstruction points with 2-0 Ethibond (DePuy Mitek, Inc. Co., NJ, USA).
Four-suture fixation (8 cases) A 1-mm Kirschner wire was used to make 4 holes on the patella surface towards the articular surface. The distance between the first hole and the medial edge of the patellar was 5 mm, and each hole spacing was 6 mm equally. When every single 2-0 Ethibond suture passed through the drilled hole, the medial hamstring tendon after pre-tension was sutured at the recon- struction points. Then the sutures were tied and fixed (Fig. 2A).
Anchors-single suture fixation (8 cases) Bone anchors (FASTIN RC, DePuy Mitek, Inc. Co.) were inserted into the reconstruction points of the medial edge of the patella. The anchors were placed at the distance of 2 cm. The medial hamstring tendon after pre-tension was tied and fixed at the anchors with a single suture (Fig. 2B).
Anchors-double suture fixation (8 cases) Bone anchors were inserted as above. The medial hamstring tendon after pre-tension was tied and fixed at the anchors with double sutures.
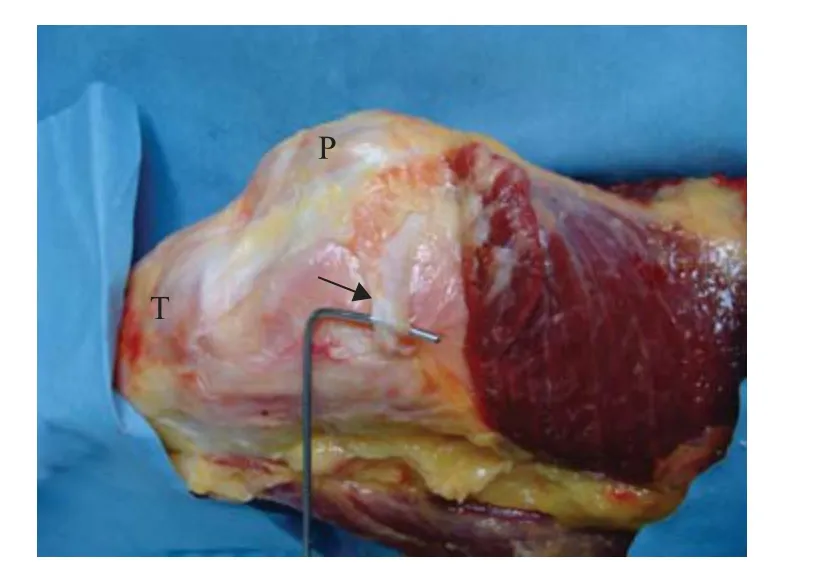
Figure 1. Normal structure of MPFL (arrow). MPFL: medial patellofemoral ligament; P: patella; T: tibia.
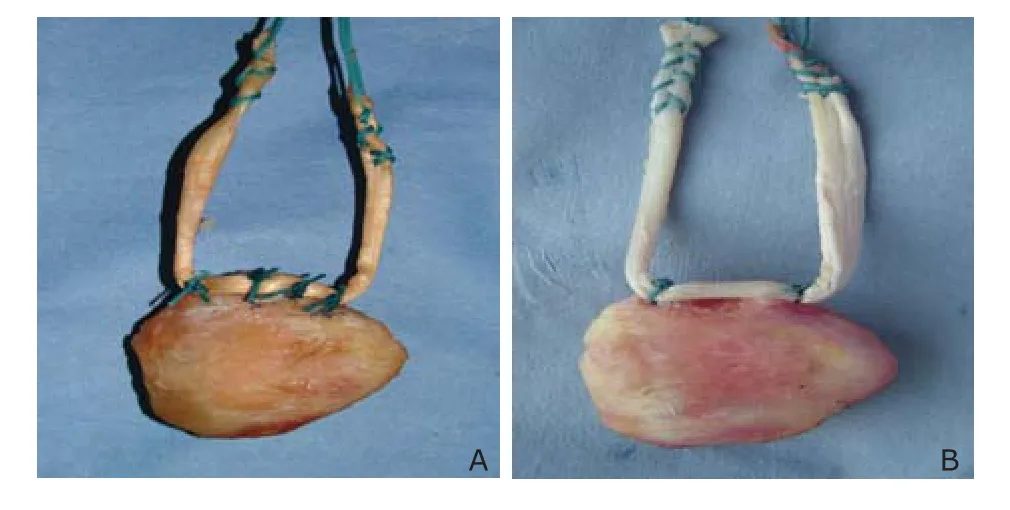
Figure 2. Hamstring tendon graft on the patella with four-suture fixation (A) and anchors-single suture fixation (B).
Tensile test
A MTS 858 Mini Bionix Ⅱ machine (MTS Systems Co., MN, USA) was used to measure the tensile strength of the normal MPFL and the tendon grafts in this study.
Tensile strength of the normal MPFL (8 cases) The femoral section of the knee joint was fixed horizontally on the bed of the testing machine. The femoral condyle was rotated internally 37° and placed directly under the traction fixture. When the patella was pulled vertically upward and clamped with the traction fixture, the MPFL was tangential to the femoral entocondyle (Fig. 3). The ligament was preconditioned by using 20 N for 10 times in order to eliminate its viscoelasticity, and then extended at the speed of 10 mm/min until rupture. The rupture mode, the maximum load and the elongation were recorded.
Tensile strength of the normal MPFL patellar side (8 cases) The part of the patella, embedded in the denture powder, was fixed on the bed of the testing machine. The other MPFL ending which was located 2 cm away from the medial margin of patella was pulled vertically upward and clamped with the traction fixture. The parameters of pre-tension and the tensile strength were used as above, until the fixation failed.
Tensile strength of the hamstring tendon graft models The part of the patella, embedded in the denture powder, was fixed on the bed of the testing machine. Both ends of the hamstring tendon grafts which were located 5 cm away from the medial margin of patella were pulled vertically upward and clamped with the traction fixture (Fig. 4). The parameters of pre-tension and the tensile strength were used as above, until the fixation failed.
Statistical analysis
Statistical analysis was performed by using SPSS 15.0 software. All data were expressed as means±standard deviation. A comparison between the two groups was performed using Student's t-test. P <0.05 was considered statistically significance.
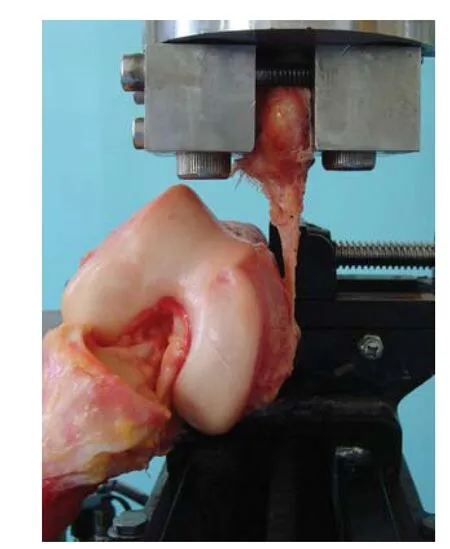
Figure 3. The femoral section was fixed horizontally. The femoral condyle was rotated internally 37°, and then the patella was pulled vertically upward with MPFL at the tangential position of the femoral entocondyle.

Figure 4. The part of the patella was embedded in the denture powder, and the hamstring tendon graft was marked 5 cm away from the medial margin of patella.
RESULTS
The rupture or failure modes were as follows. The normal MPFL group (n=8): 4 cases of avulsion of the femoral attachment and 4 cases of tear of the middle of the ligament. The normal MPFL patellar side group (n=8): 4 cases of tear of the patella attachment combined with avulsion fracture of the patellar medial edge and 4 cases of tear of the ligament fixation point. The four-suture fixation group (n=8): 6 cases of the suture cutting bone tunnel or the suture breaking and 2 cases of the medial patella fracture. The anchors-single suture fixation group (n=8): 8 cases of the suture breaking. The anchors-double suture fixation group (n=8): 6 cases of the suture breaking and 2 cases of the anchors being pulled out.
The tensile strength showed no significantly difference between the normal MPFL group and the anchors-single suture fixation group (P>0.05). There was also no significant difference among the four-suture fixation group and the normal MPFL patellar side group (all P>0.05). The tensile strength of the four-suture fixation group was significantly higher than that of the normal MPFL group (P=0.0014) and the anchors-single suture group (P= 0.0077), while lower than that of the anchors-double suture group (P=0.0052) (Table 1).
The elongation of the hamstring tendon in the four-suture fixation group had significant difference with that of the normal MPFL group (P=0.0000) and the anchors-single suture group (P=0.0016) and no difference with that of the anchors-double suture group (Table 1).
DISCUSSION
At present there are different opinions on the treatment of knee dislocation.7,8Habitual dislocation of the patella can cause a series of complications. Clinical studies have demonstrated that the MPFL-based treatment will enhance the patellofemoral stability with the purpose of the good prognosis.
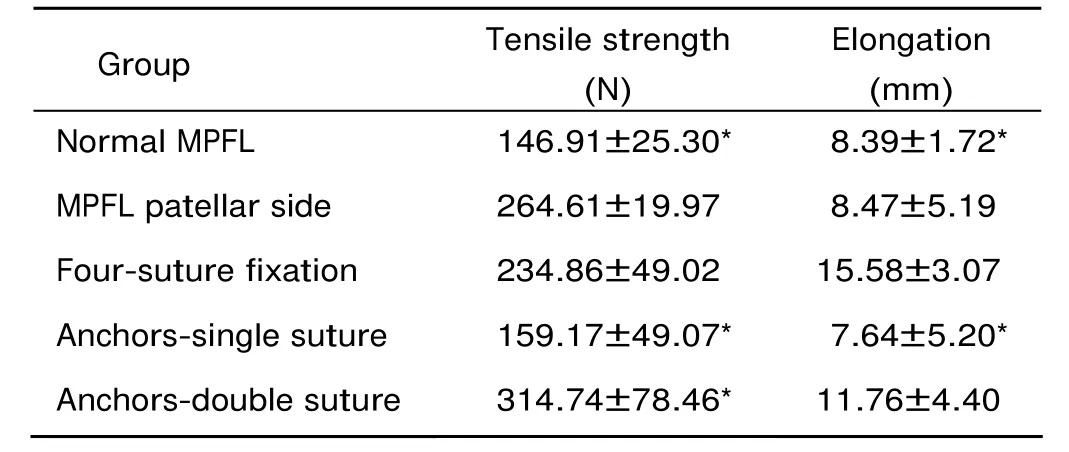
Table 1. Comparions of the tensile strength and the elongation in the five groups§ (n=8)
The anatomy of the MPFL has been described by some authors.9They defined that the MPFL originates from the adductor tubercle of the femur, immediately superior to the femoral attachment of the medial collateral ligament. The middle fibre inserts into the undersurface of the vastus medialis obliquus at the upper of the the medial margin of patella. The lower fibre extends anteriorly at the superior aspect of the medial margin of patella. The fibre in the adductor tubercle is thin and narrow, gradually becoming wider and thicker, and the thickest point is located at the medial margin of the patella attachment. Several studies10-13have shown that the MPFL is the major soft tissue restraint to lateral displacement of the patellar, providing about 50%-60% of the total medial restraining force in the range of 0° to 30° of knee flexion. The patellar dislocation and lateral displacement will occur when the MPFL is injured. Mountney et al14measured that the MPFL failed at a mean tension of 208±90 N, at 26±7 mm of elongation, which is similar to the result reported by Burks et al.15Our data is lower than it, which may be related to the ethnic difference or the loaded type. Mountney et al14reported that the MPFL was preconditioned by a series of ten cycles from 0 to 30 N, and then extended at 200 mm/min until failure. This condition is quite different from our parameter.
In our study, the tensile strength of the four-suture group was between the suture-single anchor group and the suture-double anchor group, and was close to the normal MPFL patellar side group. The elongation of the four-suture group was relatively large, which may be related to the suture sliding of the hamstring tendon graft fixation. Therefore, maintaining proper tension when the hamstring tendon was bound and fixed will reduce the elongation of the hamstring tendon graft after the reconstruction.
In various surgical procedures of MPFL reconstruction of hamstring tendon graft, there are many ways of the patellar side fixation, but the ways of the femoral side fixation are relatively unified, which are often fixed by the interfacial screw. In the biomechanical tests on different reconstruction ways, Mountney et al14demonstrated that all the failure modes were the hamstring tendon graft sliding from the interfacial screw. According to the "cask effect", the capacity of a cask is determined by its shortest wooden board, not the longest. In this study, all of the average tensile strength of three ways of the patellar side fixation were higher than or equal to the femoral side fixation measured by Mountney. Moreover, "the patella—the hamstring tendon graft—the femur" as a whole, the overall strength depends on the femoral side weakest point. Therefore, the biomechanical properties of these three ways by the patellar side fixation we have chosen are relatively reliable.
There are many controversies about which of the MPFL reconstruction techniques have better clinical effects. Recently, the hamstring tendon graft reconstruction has been reported frequently. The advantage of this method is an arthroscopic-assist surgery, so the motion trajectories of the patella can be observed and the lateral patellofemoral retinaculum get relaxation simultaneously. Among the hamstring tendon graft reconstruction techniques, the double-tunnel patellar side reconstruction has the stronger fixation strength, but the surgical trauma is relatively large, moreover, the patella of Chinese people is small, which may lead to the iatrogenic patellar fracture. The suture- anchor fixation is a minimally invasive surgery with the reliable effect, but the implant material is expensive and the body remaining may be concerned. The four-suture fixation, described in our previous study,16is characterized by small trauma, perfect fixation strength, low cost, especially no implants and easy to accept, therefore it is worth recommending. However, drilling the patellar may hurt the patellar articular surface which can contact the femoral articular surface only when the knee joint is in excess flexion. It needs further clinical observation to identify whether this damage of articular surface causes the clinical symptom or not. We suggest that the drilling angle tilted to the lateral can avoid the articular surface injury during the surgery.
In conclusion, this study demonstrates the superior stability of the four-suture fixation method for the MPFL reconstruction. Compared to the anchors-suture fixation method, it is simple, economical, and efficient. The biomechanical tests provide reference data for the clinical application.
ACKNOWLEDGEMENTS
The authors thank Zhong-li Li and Zhi-gang Wang for editing the manuscript discussion.
1. Ostermeier S, Holst M, Bohnsack M, et al. In vitro measurement of patellar kinematics following reconstruction of the medial patellofemoral ligament. Knee Surg Sports Traumatol Arthrosc 2007; 15: 276-85.
2. Deie M, Ochi M, Sumen Y, et al. A long-term follow-up study after medial patellofemoral ligament reconstruction using the transferred semitendinosus tendon for patellar dislocation. Knee Surg Sports Traumatol Arthrosc 2005; 13: 522-8.
3. Steensen RN, Dopirak RM, Maurus PB. A simple technique for reconstruction of the medial patellofemoral ligament using a quadriceps tendon graft. Arthroscopy 2005; 21: 365-70.
4. Nomura E, Inoue M, Osada N. Augmented repair of avulsion-tear type medial patellofemoral ligament injury in acute patellar dislocation. Knee Surg Sports Traumatol Arthrosc 2005; 13: 346-51.
5. Schöttle PB, Fucentese SF, Romero J. Clinical and radiological outcome of medial patellofemoral ligament reconstruction with a semitendinosus autograft for patella instability. Knee Surg Sports Traumatol Arthrosc 2005; 13: 516-21.
6. Schottle PB, Romero J, Schmeling A, et al. Technical note: Anatomical reconstruction of the medial patellofemoral ligament using a free gracilis autograft. Arch Orthop Trauma Surg 2008; 128: 479-84.
7. Cofield RH, Bryan RS. Acute dislocation of the patella: Results of conservative treatment. J Trauma 1977; 17: 526-31.
8. Davis DK, Fithian DC. Techniques of medial retinacular repair and reconstruction. Clin Orthop 2002; 402: 38-52.
9. Yu CS, Xuan Y, Li KC, et al. Anatomic study of the medial patellar retinaculum and its clinical implication. Chin J Clin Anat 2004; 22: 263-5.
10. Panagiotopoulos E, Strzelczyk P, Herrmann M, et al. Cadaveric study on static medial patellar stabilizers: The dynamizing role of the vastus medialis obliquus on medial patellofemoral ligament. Knee Surg Sports Traumatol Arthrosc 2006; 14: 7-12.
11. Hautamaa PV, Fithian DC, Kaufman KR, et al. Medial soft tissue restraints in lateral patellar instability and repair. Clin Orthop 1998; 349: 174-82.
12. Conlan T, Garth WP Jr, Lemons JE. Evaluation of the medial soft-tissue restraints of the extensor mechanism of the knee. J Bone Joint Surg Am 1993; 75: 682-93.
13. Desio SM, Burks RT, Bachus KN. Soft tissue restraints to lateral patellar translations in the human knee. Am J Sports Med 1998; 26: 59-65.
14. Mountney J, Senavongse W, Amis AA, et al. Tensile strength of the medial patellofemoral ligament before and after repair or reconstruction. J Bone Joint Surg Br 2005; 87: 36-40.
15. Burks RT, Desio SM, Bachus KN, et al. Biomechanical evaluation of lateral patellar dislocations. Am J Knee Surg 1998; 11: 24-31.
16. Wang N, Liu YJ, Yang YM, et al. Hamstring tendon autograft treatment of recurrent patellar dislocation. Junyi Jinxiu Xueyuan Xuebao 2009; 30: 603-5.
杂志排行
Chinese Medical Sciences Journal的其它文章
- What Moved into the Lung? An Unusual Case of Foreign Body Migration
- Recurrent Seizures Manifestations in a Case of Congenital Hypoparathyroidism:a Case Report
- Mechanical Stimulus Inhibits the Growth of a Bone Tissue Model Cultured In Vitro△
- CORRECTION
- Coronary Artery Perforation Complicated With Acute Aortic Valve Regurgitation During Percutaneous Coronary Intervention:Report of Two Cases
- Primary Endodermal Sinus Tumor in the Posterior Cranial Fossa:Clinical Analysis of 7 Cases
