Effect of Combining Tuina with Balance Training on Balance Functions of Stroke Patients
2013-07-18WuJiCuiXiaoWangJunShiJunchaoYeWencheng
Wu Ji, Cui Xiao, Wang Jun, Shi Jun-chao, Ye Wen-cheng
Department of Rehabilitation Medicine, Tianshan Hospital of Traditional Chinese Medicine of Changning District, Shanghai, Shanghai 200051, China
Effect of Combining Tuina with Balance Training on Balance Functions of Stroke Patients
Wu Ji, Cui Xiao, Wang Jun, Shi Jun-chao, Ye Wen-cheng
Department of Rehabilitation Medicine, Tianshan Hospital of Traditional Chinese Medicine of Changning District, Shanghai, Shanghai 200051, China
Objective: To observe the effect of combining tuina with balance training on balance functions of stroke patients.
Methods: A total of 120 cases who met the inclusion criteria were randomly allocated into an observation group and a control group. In addition to routine medical and rehabilitation treatment in both groups, balance training was used in the control group, versus combining tuina with balance training in the observation group. The therapeutic efficacies in two groups were evaluated using the Balance Subscale of the Fugl-Meyer Test (FM-B) before and after treatment.
Results: After 3 courses of treatment, the FM-B scores were significantly improved in both groups (P<0.01); and there was statistical difference in FM-B scores between the two groups (P<0.05).
Conclusion: Tuina manipulation of regulating the Governor Vessel can improve the balance function of stroke patients and benefit the patients’self-care abilities.
Tuina; Massage; Governor Vessel; Stroke; Complications; Hemiplegia; Postural Balance
Approximately 50%-80% apoplexy survivors may experience functional disturbances, especially balance problems[1]. Balance functions of human body involve sitting, standing and walking functions (i.e., static stability and motion coordination) as well as anti-interference ability in three stances. Balance reaction and spontaneous protective posture are the foundation of voluntary movement[2]. A normal balance function is the precondition and guaranty of body adaptation and daily living performance. Damaged balance function may result in disturbed motor functions. Apoplexy is a major cause of balance problems. As a traditional noninvasive traditional Chinese medicine (TCM) therapy, tuina can be easily accepted by patients. The action and effect of tuina on post-apoplectic rehabilitation have been extensively confirmed by studies from both home and abroad[3-6]. However, there is little research regarding tuina effect on balance function following stroke. This study aims to observe the effect of combining tuina with balance training on balance functions of hemiplegic patients following stroke.
1 Clinical Material
1.1 Diagnostic criteria
This is based on the Key Diagnostic Points for Cerebrovascular Diseases issued in the 4th National Academic Conference for Cerebrovascular Diseases(1995)[5]and relevant literature[6]. All cases were confirmed as cerebral infarction or hemorrhage by head CT or MRI scan.
1.2 Inclusion criteria
Those who met the above diagnostic criteria; FM-B scores <6; stable vital signs; both genders aged between 40 and 79 years old; willing to sign the informed consent.
1.3 Exclusion criteria
Active liver disease, kidney insufficiency, congestive heart failure, respiratory failure, water-electrolyte imbalance and severe malnutrition; malignant cancer; complications of apraxia of the affected limb, agnosia, hemianopsia and unilateral spatial neglect; disturbances of consciousness, psyche and intelligence; not suitable for tuina therapy.
1.4 Dropout criteria
Failed to stick to tuina therapy; failed to complete the treatment protocol due to relevant treatment events.
1.5 Statistical method
The SPSS 13.0 version software was used for data processing, () for measurement data expression, t-test for statistical analysis, and Chi-square test for numeration data. P<0.05 indicates a statistical significance.
1.6 General data
A total of 120 stroke patients treated between May 2011 and April 2012 in the Rehabilitation Department of our hospital were included in this study. They were 41 to 79 years old. These patients were randomly allocated into an observation group and a control group by a random digits table, 60 cases in each group. There were no between-group statistical differences (P>0.05) in gender, age and apoplectic nature and therefore the two groups were comparable (table 1).
The clinical managements of the two groups are shown in Fig.1.
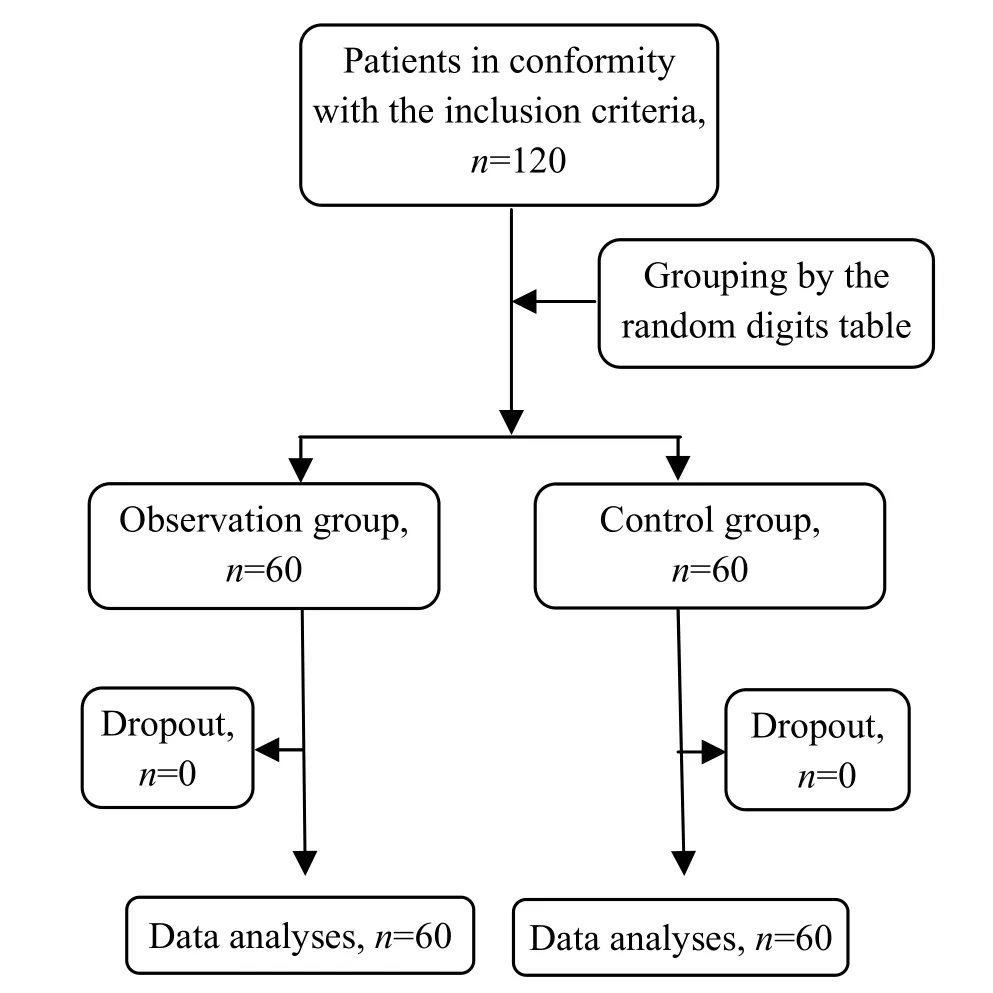
Fig.1 Clinical management flow chart
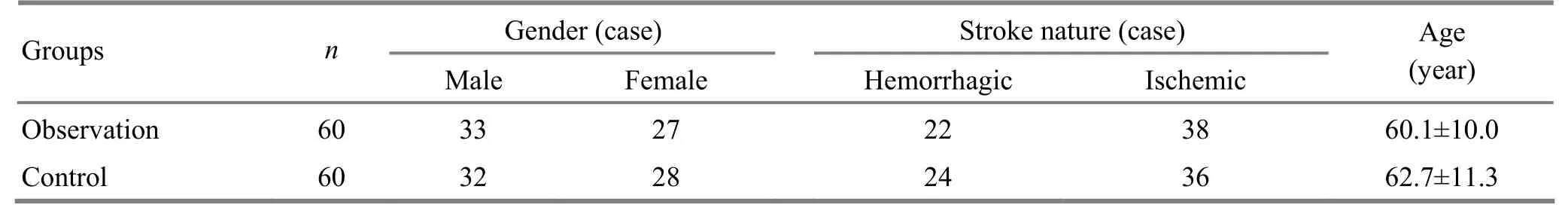
Table 1. Between-group comparison of general materials
2 Treatment Methods
2.1 Observation group
2.1.1 Tuina treatment
Treatment areas: From Dazhui (GV 14) to Changqiang (GV 1) along the pathway of the Governor Vessel, the Bladder Meridian on the back and Jiaji (EX-B 2) points.
Tuina manipulation: Gun-Rolling, An-Pressing, Ca-Rubbing, Rou-Kneading and Tanbo-Plucking.
Procedure of treatment: Ask the patient to take a prone position. First, relax the back muscles using Gun-Rolling manipulation 2-3 times from top to bottom (Fig.2). Next, An-Press and Rou-Knead the acupoints from Dazhui (GV 14) to Changqiang (GV 1) along the Governor Vessel using the thumb or thenar eminence 3-5 times till a warm sensation occurs. Then, apply Gun-Rolling and An-Pressing manipulations to the Bladder Meridian on the back 5-6 times from top to bottom. After this, Tanbo-Pluck the sacrospinous muscles on both sides using soft but penetrating manipulation (Fig.3). Follow this with heavy An-Pressing and Rou-Kneading Jiaji (EX-B 2) points. Finally, Ca-Rub the Governor Vessel and Bladder Meridian (Fig.4) till a warm sensation appears.
Time of treatment: Thirty minutes for each treatment, one treatment every day and 10 times constitute a course of treatment.

Fig.2 Gun-Rolling manipulation

Fig.3 Tanbo-Plucking manipulation

Fig.4 Ca-Rubbing manipulation
2.1.2 Balance training
The balance training shall be done step by step.
Training method: First, experience the feeling of standing with the help of a standing bed and correct the standing posture in front of a mirror (Fig.5). Next, exercise standing with and without support of the standing bed. Regarding weight-bearing exercise of the legs, first stand with help (by controlling the key areas in the knee and low back) or stand against a wall; try gradually to stand without help and exercise standing with separated legs, standing by placing two legs together and standing in a straight line (Fig.6); and then shift from standing with weight-bearing of both legs to standing on the affected leg (Fig.7). Ask the patient to lift arm and reach different objects in a standing posture. Exercise of back, front, left and right shift of the body weight in a balance trainer can improve the affected leg’s weight-bearing and standing balance ability. After this, the patient can continue with head, upper limb, torso and lower limb movements in a standing posture and exercise standing in a balance board.
Time of training: Twenty minutes for each training, and 10 times constitute a course of treatment.

Fig.5 Standing in front of a mirror

Fig.6 Standing with both legs
2.2 Control group
Rehabilitative balance training alone was conducted in the control group. The method and time of training were same as those of the observation group.

Fig.7 Standing with one leg
3 Treatment Results
3.1 Observation indexes
The patient’s balance ability was evaluated using FM-B. The FM-B contains 7 three-point (0-2) items, namely, sitting without support, parachute reaction (both sides), standing with support, standing without support, unilateral stance (both sides). The total score ranges from 0 to 14. A higher score indicates a better balance ability. The balance functions of patients in both groups were evaluated respectively before and after 3-course treatment by a therapist who was not involved in the study.
3.2 Results
There were no dropout cases in both groups during treatment. After 3 courses of treatment, the FM-B scores in both groups were significantly increased (P<0.01); and there was statistical difference in FM-B score between the two groups (P<0.05), indicating that the balance function was improved more significantly in the observation group than that in the control group (table 2).
Table 2. Between-group FM-B score comparison before and after treatment (, point)
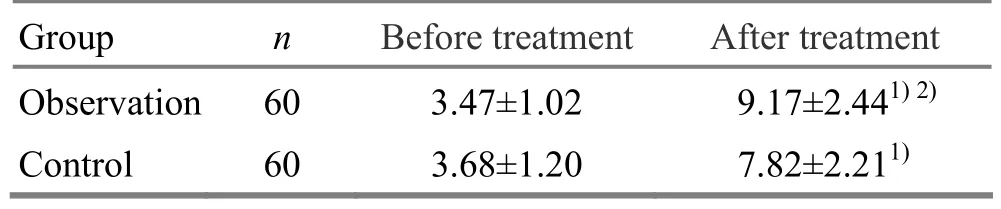
Table 2. Between-group FM-B score comparison before and after treatment (, point)
Note: Compared with the intra-group results before treatment, 1) P<0.01; compared with the control group, 2) P<0.05
Group n Before treatment After treatment Observation 60 3.47±1.02 9.17±2.441)2)Control 60 3.68±1.20 7.82±2.211)
4 Discussion
Apoplexy is a major cause of balance problems. Apoplexy patients frequently present increased postural sway, longer preparation of postural muscles, lower motion speed, prolonged latent period of postural adjustment and decreased autonomic response[7]. Quantitative analysis of static equilibrium has shown a significant static stability decrease in stroke patients[8]. In addition, apoplexy above the cerebral cortex, basal ganglia, thalamus and pons can all result in crossed cerebellar diaschisis[9]. The static and dynamic standing balance is the precondition of recovering walking ability after stroke[10]. Normal independent walking ability has high positive correlations with the torso control ability and standing balance[11], and the somatic balance control function in early hemiplegic state is of important prognosis value for long-term functional rehabilitation[12]. Numerous studies have suggested that balance function could facilitate the improvement of limb movement and daily living[13-15]. Consequently, it is essential to restore the balance function of stroke patients.
In Chinese medicine, qi disorder and yin-yang imbalance account for the balance disturbance following stroke. The principle of treatment is therefore to coordinate yin and yang of the body.
The Governor Vessel governs yang-qi of the entire body and is dubbed as the ‘sea of yang meridians’. Since it runs along the spine and enters the brain, the Governor Vessel is closely associated with the brain and spinal cord[16-17]. Tuina manipulation on the Governor Vessel can activate yang-qi, regulate meridians and refresh the brain. Also, the Governor Vessel connects with the Conception Vessel (the sea of yin meridians), so that tuina manipulation can regulate functions of all Zang-fu organs. By stimulating the Governor Vessel with An-Pressing, Rou-Kneading and Gun-Rolling manipulations, multiple meridians can be regulated as well. This can in turn activate yang qi, balance yin and yang and benefit qi activities. An-Pressing and Rou-Kneading Jiaji (EX-B 2) points (locate between the Governor Vessel and the Bladder Meridian) can further facilitate the regulation on the Governor Vessel.
This study has indicated that tuina manipulations of regulating the Governor Vessel can regulate qi activity, rebalance yin and yang, and thus improve balance function of stroke patients.
[1] Chen SZ, Zhang BF, Zhao JL, Chen ZH, Huang DF. The role of cognition function in balance control of patients post-stroke. Zhongguo Kangfu Yixue Zazhi, 2010, 25(2): 139-144.
[2] Wang MB. Modern Evaluation and Treatment for Hemiplegia. Beijing: Huaxia Publishing House, 1990: 67.
[3] Zhou GH. Effects of tuina treatment and facilitation technique on motor functions in apoplexy patients: a comparative study. Anmo Yu Daoyin, 2002, 18 (6): 17-18.
[4] Lin P, Li L, Xu HW, Bao XQ. Segmental tuina and post-apoplectic limb function improvement. Zhongguo Linchuang Kangfu, 2003, 7(10): 1610-1611.
[5] Chinese Neuroscience Society, Chinese Neurosurgical Society. Key diagnostic points for cerebrovascular diseases. Zhonghua Shenjing Waike Zazhi, 1997, 13 (1): 3-4.
[6] Chu HL, Zhan HS, Hou Q, Wang J, Cai XY, Ruan JY. Clinical study on tuina for early ischemic cerebral infarction in middle-aged and elder population. Zhejiang Zhongyi Xueyuan Xuebao, 2002, 26(3): 62-63.
[7] Zhou SX, Liu M. The clinical analysis of rehabilitation effects on stroke hemiparalysis. Qinghai Yixueyuan Xuebao, 2002, 23(3): 56-57.
[8] Yan TB. Balance test and balancing response-postapoplectic ability changes. Guowai Yixue: Wuli Yixue Yu Kangfu Xue Fence, 1991, (2): 72-74.
[9] Yang PJ, Chen JN, Zhang Q, Chen KM, Jiang B, Shao J, Cai HO, Wang MF, Zhang WM. Clinical application of balance function test with homemade computerized balance instrument. Zhongguo Kangfu Yixue Zazhi, 1998, 13(4): 153-156.
[10] Lang SY, Zhu K. Clinical significance of crossed cerebellar diaschisis. Guowai Yixue: Nao Xueguan Fence, 1995, 3(1): 39-41.
[11] Sun J, Tan DS. Walking function reconstruction of postapoplectic hemiplegia patients. Xiandai Kangfu, 2001, 5(9): 59.
[12] Ni CM, Fu J, Gao XP, Han R, Liu CY, Ge JP, Chen HM. Prediction for the ability of independent walking in acute stroke patients. Zhonghua Wuli Yixue Yu Kangfu Zazhi, 1999, 21(4): 196-198.
[13] Guo YQ, Chen LY, Li WX, Zhen ZC. Effect of combining acupuncture on Back-Shu points with functional bed exercise on torso control of apoplexy patients. Xiandai Kangfu, 2001, 5(2): 31-32.
[14] Huang LP, Wei GR, Song LX, Huang MW. Balance training for the aged with stroke. Zhongguo Kangfu Yixue Zazhi, 1996, 11(2): 56-58.
[15] Ni CM, Fu J, Liu CY, Gao XP, Ge JP, Han R, Chen HM. Standing balance and motor control of apoplexy patients. Xiandai Kangfu, 1997, 1(5): 358-359.
[16] Wei GR, Song LX, Huang MW, Huang LP, Qu L. Effects of selective trunk activities training on the recovery of hemiplegic patients. Zhongguo Kangfu Yixue Zazhi, 1998, 13(3): 108-110.
[17] Yu XX, Han L, Yin ZH. Therapeutic efficacy observation on puncturing the Governor Vessel acupoints for 50 stroke patients. Zhenjiu Linchuang Zazhi, 1999, 15(3): 11-12.
Translator: Han Chou-ping
Received Date: January 8, 2013
R246.1
A
both groups
medical and rehabilitative treatment to control high risk factors including blood pressure, blood sugar, blood fat, and blood viscosity.
Author: Wu Ji, bachelor, attending physician.
E-mail: wuji1022@hotmail.com
杂志排行
Journal of Acupuncture and Tuina Science的其它文章
- Therapeutic Efficacy Observation on Integrative Acupuncture Therapy for Chronic Urticaria
- Research Progress of Acupuncture-moxibustion for Insomnia: An Analysis of Literature in Recent 5 Years
- Treatment Frequency and Long-term Efficacy Observation on Electric Pudendal Nerve Stimulation for Stress Urinary Incontinence
- Clinical Observation on Treatment of Insomnia with Puncturing Back-Shu Acupoints
- Therapeutic Efficacy Observation on Acupuncture for Postmenopausal Osteoporosis
- Clinical Observation on Acupuncture for Perimenopausal Syndrome