Treatment Frequency and Long-term Efficacy Observation on Electric Pudendal Nerve Stimulation for Stress Urinary Incontinence
2013-07-18ZhaoLinWangSiyou
Zhao Lin, Wang Si-you
1 Nephrology Department, Longhua Hospital Affiliated to Shanghai University of Traditional Chinese Medicine, Shanghai 200032, China
2 Shanghai Research Institute of Acupuncture and Meridian, Shanghai 200030, China
Treatment Frequency and Long-term Efficacy Observation on Electric Pudendal Nerve Stimulation for Stress Urinary Incontinence
Zhao Lin1, Wang Si-you2
1 Nephrology Department, Longhua Hospital Affiliated to Shanghai University of Traditional Chinese Medicine, Shanghai 200032, China
2 Shanghai Research Institute of Acupuncture and Meridian, Shanghai 200030, China
Objective: To observe the effect of different treatment frequency of electric pudendal nerve stimulation (EPNS) on stress urinary incontinence (SUI).
Methods: A total of 60 female SUI cases were randomly allocated into group A and group B, 30 in each group. Cases in both groups were treated with EPNS, 3 times a week for group A, versus twice a week for group B. Then clinical symptoms, stress urinary incontinence and quality of life (QOL) were assessed respectively before treatment and after 12 times of treatment by using questionnaire. In addition, for 99 cases whose clinical symptom scores were reduced by more than 50% after EPNS treatment, a telephone interview follow-up was conducted.
Results: The cases in the treatment group were better than those in the control group in the enhancement of clinical effects, the decline of VAS scores and the improvement of clinical symptoms and sign integrals, with statistical significance (P<0.01 or P<0.05).
Conclusion: EPNS has positive effect for female SUI; different treatment frequencies have certain impact on clinical effect: the effect achieved by 3 times a week was better than that by twice a week; and this therapy has stable long-term effect.
Acupuncture Therapy; Electroacupuncture; Urinary Incontinence, Stress
Stress urinary incontinence (SUI) is the involuntary leakage of urine with increased abdominal pressure (such as coughing, sneezing, laughing, running or exercise) in the absence of a detrusor contraction[1]. This study aimed to further study the treatment frequency and long-term effect of managing female SUI with electric pudendal nerve stimulation (EPNS).
1 Clinical Material
1.1 Diagnostic criteria
The SUI diagnostic criteria in this study are based on Campbell’s Urology[2], the Guidance to Diagnosis and Treatment of Modern Urology[3]and the Modern Urology[4].
Female SUI patients shall meet the first three items and one of the last three items: ① SUI symptoms or a history of SUI; ① positive stress test (leakage of urine upon coughing or exertion-induced increase in abdominal pressure); ③positive Marshall-Marchetti test (finger pressure test); ④ uninhibited contraction with normal bladder volume and sensation by urodynamic testing;⑤ immediate postvoid residual <50 mL; ⑥ the urinary incontinence score in the diagnosis of female SUI[5]>12.
1.2 Inclusion criteria
Aged from 18 to 80 years; meeting the first 5 items, or the first 3 items and the 6th item in the diagnostic criteria; willing to sign the informed consent.
1.3 Exclusion criteria
Urge incontinence; neurogenic bladder.
1.4 General data
A total of 60 female SUI patients treated from May 2009 to December 2010 were divided into two groups. Thirty cases in group A were treated in Shanghai Research Institute of Acupuncture and Meridian, whereas 30 cases in group B were treated in Yueyang Hospital of Integrated Chinese and Western Medicine Affiliated to Shanghai University of Traditional Chinese Medicine.
Statistical management showed that there were no significant differences in age, duration, menopausal time and initial female SUI urinary incontinence score between the two groups (P>0.05). The two groups were therefore comparable (table 1).
Table 1. Between-group comparison of general data ()
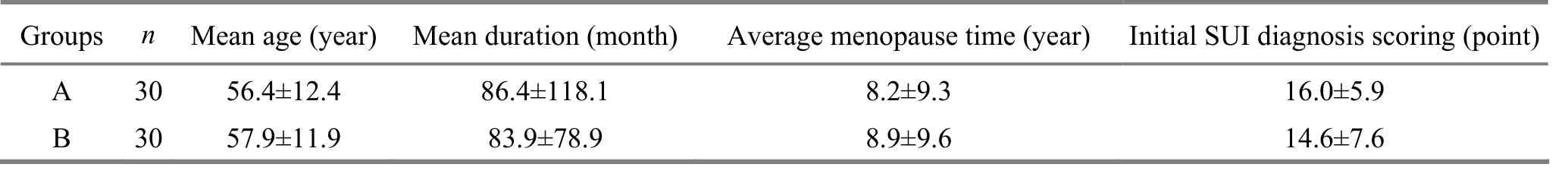
Table 1. Between-group comparison of general data ()
A 30 56.4±12.4 86.4±118.1 8.2±9.3 16.0±5.9 Initial SUI diagnosis scoring (point) B 30 57.9±11.9 83.9±78.9 8.9±9.6 14.6±7.6
2 Treatment Methods
2.1 Points
Ask the patient to take a prone position and select bilateral upper and lower points according to the pathway of pudendal nerve (Fig.1).
Upper point: Lateral to the sacrum border, at the same level of the 4th posterior sacral foramen.
Lower point: 0.5 cun lateral to the coccyx.

Fig.1 Acupuncture points
2.2 Method
After routine disinfection, puncture the upper points to a depth of 75-90 mm using long needles of 0.4 mm in diameter and 100 mm in length, enabling the needling sensation to reach the urethra or anus. Puncture the lower points obliquely to a depth of 90-110 mm using long needles of 0.4 mm in diameter and 100 or 125 mm in length, enabling the needling sensation to reach the urethra[6-7]. Then connect the two electrodes of G6805-II electroacupuncture apparatus (manufactured by Shanghai High Technology Medical Equipment Company) with the ipsolateral upper and lower needles (upper needle connecting with positive electrode and lower needle with negative electrode) for 60 min, using continuous wave, 2.5 Hz frequency and tolerable intensity. It is important to induce an upward rhythmic contraction of the patient’s pelvic floor muscles (centered on the urethra) during electric stimulation.
2.3 Time of treatment
Cases in both groups were treated with same EPNS by the same operator. Cases in group A were treated 3 times a week, whereas cases in group B were treated twice a week, 12 times in total for both groups.
3 Treatment Results
3.1 Observation indexes
The following indexes were observed before and after 12 times of treatment. The SUI symptom severity and quality of life (QOL) scoring were based on modified SUI symptom and QOL questionnaire[8](table 2). In addition, the symptom and QOL were scored respectively before and after 12 times of treatment.
3.2 Criteria for therapeutic efficacy[8]
Recovery: Complete absence of clinical symptoms, the symptom scores 0 or is reduced by 100%.
Marked effectiveness: Clinical symptom scores are reduced by 75% or more.
Improvement: The symptom scores are reduced by 50% or more but less than 75%.
Failure: The symptom scores are reduced less than 50%.
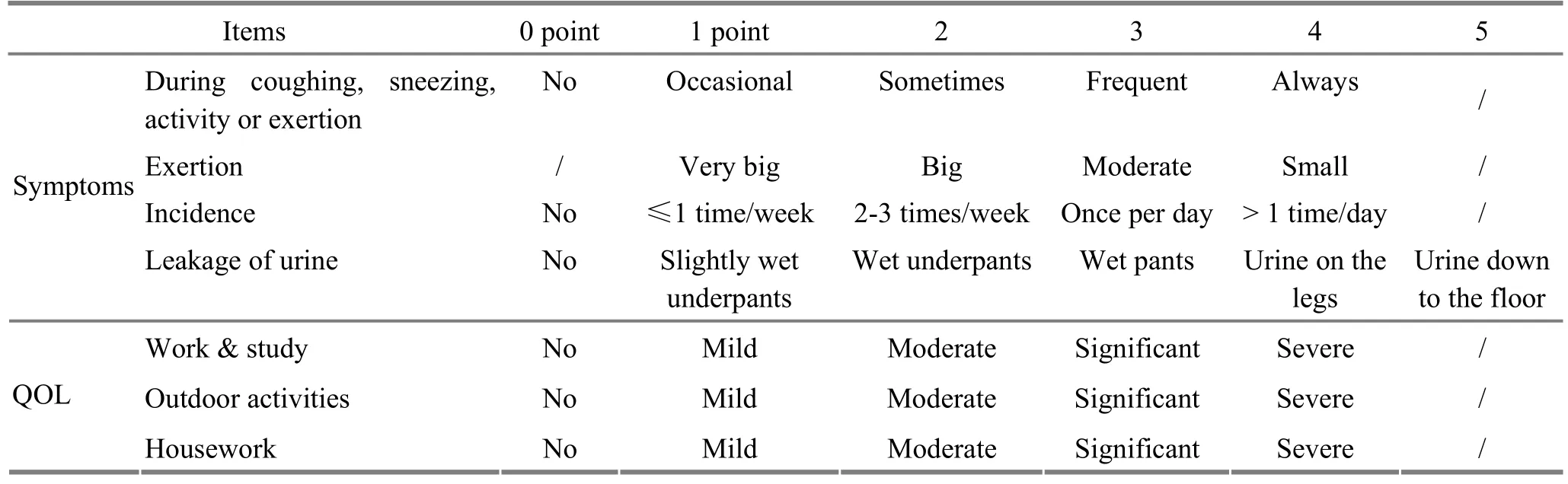
Table 2. SUI patients’ symptom and QOL scoring
3.3 Statistical method
The SPSS 18.0 version software was used for data processing, () for expression of normal distribution of measurement data, M (QL, QU) for expression of abnormal distribution, t-test for normal data distribution, Wilcoxon signed rank sum test for abnormal data distribution, analysis of variance for normal betweengroup data distribution comparison and Mann-Whitney U test for abnormal between-group data distribution comparison.
3.4 Treatment outcome
3.4.1 Between-group comparison of symptom and QOL scores
The clinical symptoms in both groups were significantly improved after treatment (P<0.01), and there were between-group statistical differences (P<0.01), (table 3).
3.4.2 Between-group comparison of clinical effects
The Mann-Whitney U test showed a statistical significance in therapeutic effect between the two groups (P<0.05). The therapeutic effect in group A was better than that in group B (table 4).
4 Long-term Follow-up
4.1 Follow-up subjects
A total of 120 female SUI cases were treated in Shanghai Research Institute of Acupuncture and Meridian between March 2004 and April 2011. A follow-up study was conducted in 99 cases whose clinical symptom score was reduced by 50% or more. Cases following 24 months or longer follow-up study were selected as our long-term observation subjects.
4.2 Follow-up method
A telephone interview was made to evaluate the long-term effect according to the therapeutic efficacy criteria.
4.3 Follow-up results
4.3.1 Comparison of long-term clinical symptom scores
The results showed a statistical significance between the follow-up and pre-treatment scores (P<0.01); however, there was no statistical significance between follow-up and post-treatment scores (table 5).
4.3.2 Comparison of long-term clinical effects
There was no statistical significance between followup and post-treatment effects (P>0.05), (table 6).
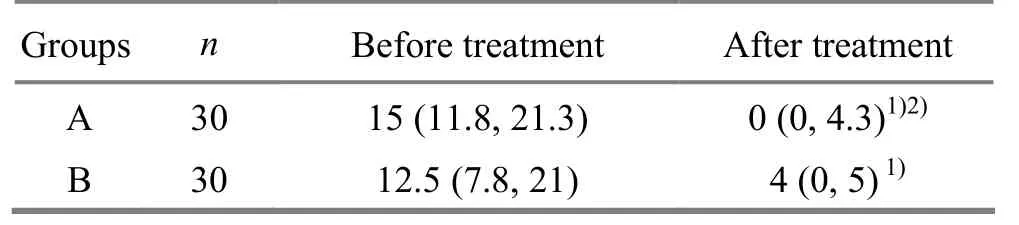
Table 3. Between-group comparison of symptoms and QOL scores before and after treatment [M (QL, QU)]
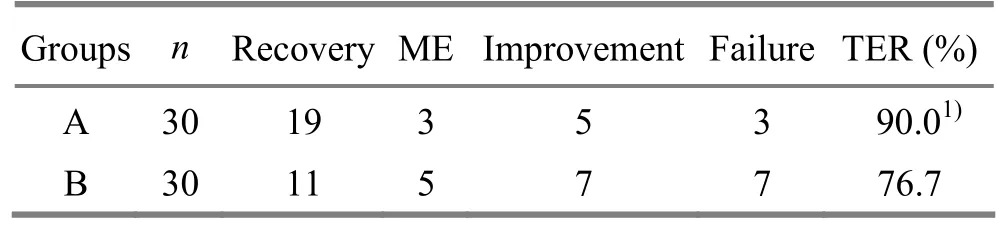
Table 4. Between-group comparison of clinical effects (case)
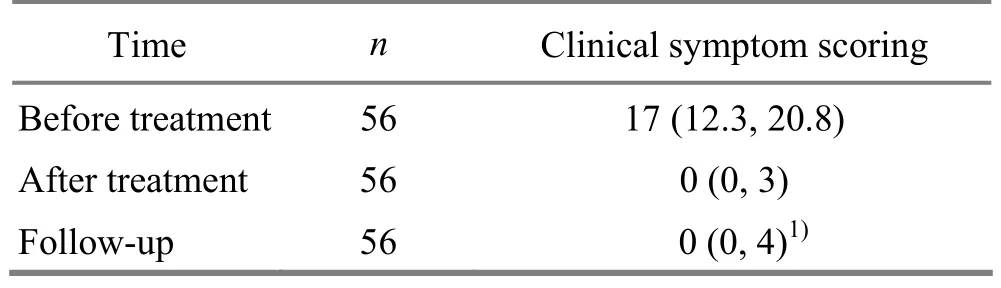
Table 5. Between-group comparison of long-term symptoms score [M (QL, QU)]
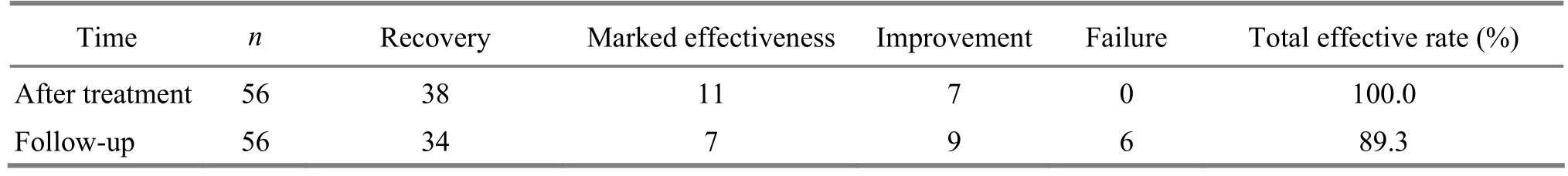
Table 6. Comparison between post-treatment and follow-up clinical efficacy (case)
5 Discussion and Conclusion
EPNS[9]synthesized the strong points of pelvic floor exercises[10], electrical nerve stimulation therapy[11-12]and deep acupuncture using long needles. By directly activating the pudendal nerve, this method can induce rhythmic contraction of the pelvic floor muscles and thus strengthen these muscles to hold urine and control urination. Unlike active pelvic floor exercises, EPNS is a passive exercise method, which can directly induce passive contraction of the pelvic floor muscles (without patients’ voluntary muscle contraction exercise) and therefore enhance patients’ compliance[13].
This clinical trial has indicated that EPNS is positively effective for female SUI. In terms of treatment frequencies, patients who were treated 3 times a week obtained better effects than those who were treated twice a week. Within a certain time frame, an increased frequency means more pelvic floor exercises, which can in turn strengthen the contraction of the pelvic floor muscles and improve the clinical effect. These findings are consistent with other relevant report[14].
The follow-up results have proved positive long-term effect. The follow-up telephone interviews 2 years after treatment have preliminarily confirmed stable long-term effect of EPNS on female SUI. There were no statistical significances in long-term effects between posttreatment and follow-up results.
In summary, EPNS has positive effect for female SUI. Compared with treatment frequency of twice a week, patients who were treated 3 times a week obtained better effects. Additionally, this method can achieve stable long-term effects.
[1] Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U, Van Kerrebroeck P, Victor A, Wein A.The standardisation of terminology in lower urinary tract function: report from the standardisation sub-committee of the International Continence Society. Urology, 2003, 61(1): 37-49.
[2] Walsh PC, Retik AB. Campbell’s Urology. 7th Edition (photocopied English version). Beijing: Science Press, 2001: 1007-1029.
[3] Wu JP. Urology Surgery. Jinan: Shandong Science & Technology Press, 1993: 780-791.
[4] Ma TX. Modern Urology Surgery. Tianjin: Tianjin Science and Technology Press, 2000: 925-946.
[5] Ishiko O, Hirai K, Sumi T, Nishimura S, Ogita S. The urinary incontinence score in the diagnosis of female urinary incontinence. Int J Gynaecol Obstet, 2000, 68(2): 131-137.
[6] Wang SY. Electroacupuncture pudendal nerve stimulation and its application. J Acupunct Tuina Sci, 2013, 11(2): 117-121.
[7] Wang SY, Yan JJ, Chen GM, Xu MY. Simultaneous perineal ultrasound and vaginal pressure measurement proves electroacupuncture pudendal nerve stimulation. J Acupunct Tuina Sci, 2009, 7(1): 41-46.
[8] Kulseng-Hanssen S, Borstad E. The development of a questionnaire to measure the severity of symptoms and the quality of life before and after surgery for stress incontinence. BJOG, 2003, 110(11): 983-988.
[9] Wang SY, Zhang SJ. Simultaneous perineal ultrasound and vaginal pressure measurement prove the action of electrical pudendal nerve stimulation in treating female stress incontinence. BJU Int, 2012, 110(9): 1338-1343.
[10] Truijen G, Wyndaele JJ, Weyler J. Conservative treatment of stress urinary incontinence in women: who will benefit? Int Urogynecol J Pelvic Floor Dysfunct, 2001, 12(6): 386-390.
[11] Jeyaseelan SM, Haslam EJ, Winstanley J, Roe BH, Oldham JA. An evaluation of a new pattern of electrical stimulation as a treatment for urinary stress incontinence: a randomized, double-blind, controlled trial. Clin Rehabil, 2000, 14(6): 631-640.
[12] Smith AL, Moy ML. Modern management of women with stress urinary incontinence. Ostomy Wound Manage, 2004, 50(12): 32-41.
[13] Wang SY, Chen GM, Li LH. “Needling 4 sacrum points”for stress incontinence in women. Shanghai Zhenjiu Zazhi, 2006, 25(5): 15-17.
[14] E JS. Needling Shenque (CV 8) for stress urinary incontinence in women. Shanghai Zhenjiu Zazhi, 1998, 17(6): 7.
Translator: Han Chou-ping
Received Date: February 20, 2013
R246.3
A
es, 56
24 months or longer follow-up: 24-90 months (47.8±20.8 months on average). These patients aged from 35 to 78 years (mean age: 55.4±9.0 years) and their conditions lasted from 1 to 240 months (mean duration: 60.7±50.0 months).
Author: Zhao Lin, doctoral student
Wang Si-you, chief physician, researcher.
E-mail: wangsiyou1234@163.com
杂志排行
Journal of Acupuncture and Tuina Science的其它文章
- Therapeutic Efficacy Observation on Integrative Acupuncture Therapy for Chronic Urticaria
- Research Progress of Acupuncture-moxibustion for Insomnia: An Analysis of Literature in Recent 5 Years
- Clinical Observation on Treatment of Insomnia with Puncturing Back-Shu Acupoints
- Therapeutic Efficacy Observation on Acupuncture for Postmenopausal Osteoporosis
- Clinical Observation on Acupuncture for Perimenopausal Syndrome
- Clinical Observation on Deep Acupuncture at Huantiao (GB 30) for Patients with Chronic Prostatitis