Therapeutic Efficacy Observation on Acupuncture for Postmenopausal Osteoporosis
2013-07-18DuGeshu
Du Ge-shu
Acupuncture Department, Changsha Hospital of Traditional Chinese Medicine, Hunan 410100, China
Therapeutic Efficacy Observation on Acupuncture for Postmenopausal Osteoporosis
Du Ge-shu
Acupuncture Department, Changsha Hospital of Traditional Chinese Medicine, Hunan 410100, China
Objective: To observe the clinical efficacy of acupuncture for postmenopausal osteoporosis (PMOP).
Methods: A total of 64 PMOP cases were randomized into an observation group and a control group, 32 cases in each group. Acupuncture was employed in the observation group, versus oral Osteoform capsule in the control group. After 3-month treatment, the Bone Density (BD) and Estradiol (E2) were measured respectively before and after treatment, followed by statistical analysis on clinical efficacies in the two groups.
Results: The total effective rate of the observation group was 81.3%, showing a statistical difference compared with the control group (P<0.05). After treatment, the BD measurements in all body regions of the observation group were significantly elevated (P<0.05), showing a statistical difference compared with the control group (P<0.05). Also, the E2levels in both groups were significantly increased (P<0.01), showing no between-group statistical significance (P>0.05).
Conclusion: Acupuncture has exact efficacy for PMOP and is therefore effective for the prevention and treatment of PMOP.
Acupuncture Therapy; Osteoporosis, Postmenopausal; Bone Density; Estradiol
Postmenopausal osteoporosis (PMOP) is frequently seen in women after menopause. It is associated with the reduction of estrogen level. PMOP can greatly affect these women’s qualify of life, since it causes pain, fracture, a stooped posture, reduction of height and even declined respiratory function. Acupuncture has great potential in the prevention and treatment of PMOP with its safety, efficacy and absence of adverse reactions. We treated 32 PMOP cases with acupuncture and then compared with oral medication Osteoform capsule. The report is now summarized as follows.
1 Clinical Materials
1.1 Diagnostic criteria
This is based on the diagnostic criteria for osteoporosis stipulated in the Guiding Principles for Clinical Study of New Chinese Medicines[1]. Its major symptoms include general weakness and progressively aggravated lumbar and back pain; fracture can occur upon mild trauma; deformed posterior process of the vertebral column; osteopenia confirmed by X-ray, particularly seen in the spine, pelvis and superior part of the femur, possible presence of a double-concave shape resembling a fish tail and widened intervertebral space;and positive sign by bone density (BD) measurement.
1.2 Inclusion criteria
Those who met the above diagnostic criteria; postmenopausal women; and those who signed the informed consent.
1.3 General data
A total of 64 outpatients from the Acupuncture Department of our hospital who met the inclusion criteria were randomly allocated into an observation group and a control group by their visit sequences. The ages of 32 cases in the observation group ranged from 56 to 73 years, with an average age of (64±8), versus 59 to 75 years in the control group, with an average age of (66±9). The disease duration of 32 cases in the observation group lasted from 3 to 10 years, with an average duration of (5.7±2.3) years, versus 2-12 years in the control group, with an average duration of (5.6±3.3) years. There were no between-group statistical significances in age, duration and disease condition (P>0.05), and thus the two groups are comparable.
The clinical managements of the two groups are shown in Fig.1.
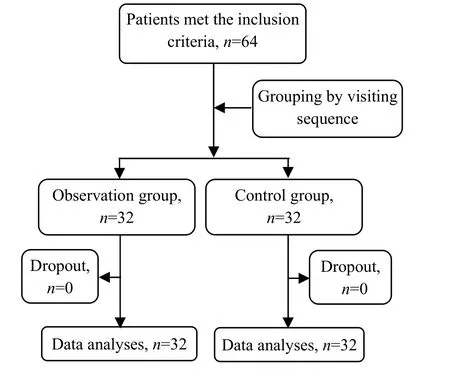
Fig.1 Clinical management flow chart
2 Treatment Methods
2.1 Observation group
Acupoints: Bilateral Qimen (LR 14), Ganshu (BL18), Pishu (BL 20), Shenshu (BL 23), Zusanli (ST 36), Yanglingquan (GB 34), Xuanzhong (GB 39), Sanyinjiao (SP 6), Taixi (KI 3) and Taichong (LR 3).
Methods: Ask the patient to take a sitting position and disinfect the local area with 75% alcohol. Using disposable filiform needles of 0.30 mm in diameter and 25-50 mm in length, puncture Qimen (LR 14) 0.5-0.8 cun obliquely outward, puncture Ganshu (BL 18) 0.5-0.8 cun obliquely inward, puncture Pishu (BL 20), Shenshu (BL 23) and Taixi (KI 3) perpendicularly, puncture Xuanzhong (GB 39) 0.5-0.8 cun perpendicularly, puncture Taichong (LR 3) 0.5-0.8 cun perpendicularly, puncture Yanglingquan (GB 34) and Sanyinjiao (SP 6) 1-1.5 cun perpendicularly and puncture Zusanli (ST 36) 1-2 cun perpendicularly. Upon arrival of qi sensation, apply reducing manipulation by lifting and thrusting to Taichong (LR 3), reinforcing manipulation by twirling to Ganshu (BL 18), Pishu (BL 20), Shenshu (BL 23), Zusanli (ST 36), Sanyinjiao (SP 6) and Taixi (KI 3) and even reinforcing-reducing manipulation to Qimen (LR 14), Yanglingquan (GB 34) and Xuanzhong (GB 39). Retain the needles for 30 min, and manipulate once every 10 min. The treatment was conducted once every other day for 3 months (45 times of treatment in total).
2.2 Control group
Cases in the control group were given oral Osteoform capsule (each capsule contains 778.6 mg of calcium and 3 200 IU of vitamin D), 1 capsule for each dose, one dose a day, for 3 months in total.
3 Therapeutic Efficacy Observation
3.1 Observation indexes
BD: It was measured using a bone densitometer.
Locations: L2-4, Ward’s triangle, greater trochanter (GT) and neck regions of the left femur.
Estradiol (E2): The E2was measured using the chemiluminescence immunoassay.
The above indexes were measured once before and after treatment respectively by professionals from the Clinical Laboratory Department of Changsha Hospital of Traditional Chinese Medicine.
3.2 Therapeutic efficacy criteria
This is based on the therapeutic efficacy criteria for osteoporosis stipulated in the Guiding Principles for Clinical Study of New Chinese Medicines[1].
Marked effectiveness: Complete absence of pain, coupled with increased BD through a bone densitometer.
Improvement: Significant relief of pain, coupled with absent reduction of BD through a bone densitometer.
Failure: No changes at all after treatment.
3.3 Statistical method
The SPSS 16.0 version software was used for data processing, Wilcoxon rank sum test for ranked data, t-test for measurement data and Chi-square test for numeration data.
3.4 Treatment results
3.4.1 Comparison of the clinical effect between the two groups
The total effective rate of the observation group was 81.3%, there was a statistical difference between the two groups (P<0.05), (table 1).
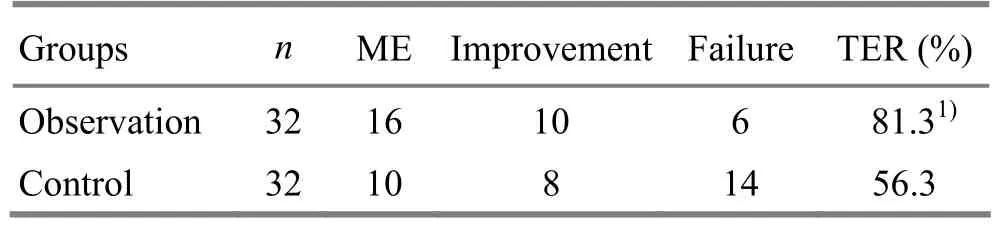
Table 1. Comparison of the clinical effect between the two groups (case)
3.4.2 Comparison of the BD between the two groups before and after treatment
After treatment, the bone densities in L2-4, left femur neck, Ward’s and GT regions in the observation group were significantly increased (P<0.05), showing a statistical significance between the two groups (P<0.05), (table 2).
Table 2. Comparison of the BD between the two groups (, g/cm2)
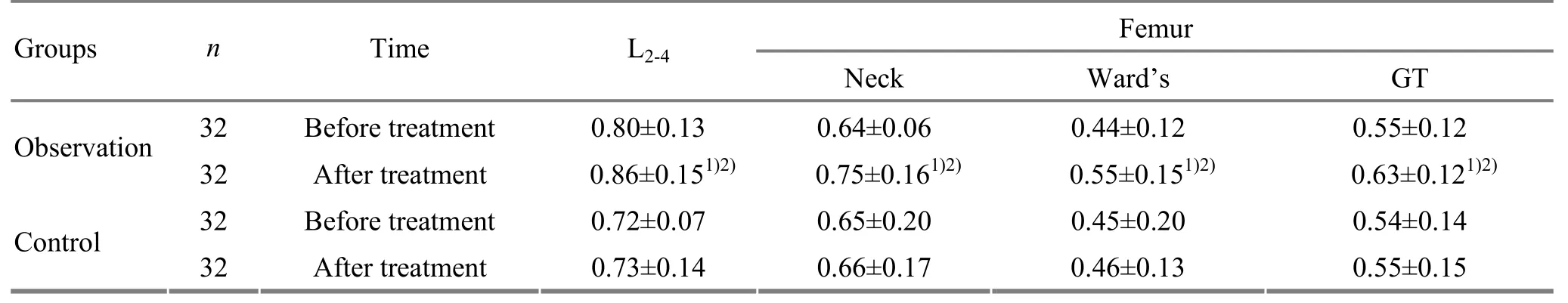
Table 2. Comparison of the BD between the two groups (, g/cm2)
Note: Compared with the intra-group results before treatment, 1) P<0.05; compared with the control group, 2) P<0.05
32 Before treatment 0.80±0.13 0.64±0.06 0.44±0.12 0.55±0.12 Observation 32 After treatment 0.86±0.151)2)0.75±0.161)2)0.55±0.151)2)0.63±0.121)2)32 Before treatment 0.72±0.07 0.65±0.20 0.45±0.20 0.54±0.14 Control 32 After treatment 0.73±0.14 0.66±0.17 0.46±0.13 0.55±0.15
3.4.3 Comparison of the blood serum E2between the two groups
After treatment, the E2levels in both groups were significantly elevated (P<0.01), showing no statistical significance.
Table 3. Between-group blood serum E2comparison before and after treatment (, pg/mL)
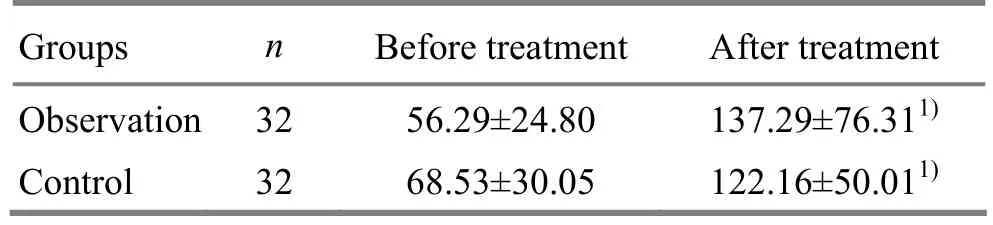
Table 3. Between-group blood serum E2comparison before and after treatment (, pg/mL)
Note: Compared with the intra-group results before treatment, 1) P<0.01
Groups n Before treatment After treatment Observation 32 56.29±24.80 137.29±76.311)Control 32 68.53±30.05 122.16±50.011)
4 Discussion
Osteoporosis is a systemic metabolic bone disease characterized by reduced bone mineral density (BMD), low extracellular matrix, microarchitectural deterioration and loss of trabecular bone that predisposes patients to increased bone fragility and fracture. Postmenopausal osteoporosis generally develops when estrogen levels drop precipitously, leading to abnormal bone metabolism, excessive bone resorption (breakdown), enhanced functional compensation of osteoblasts. This can further result in bone resorption (breakdown) outpacing the building of new bone, loss of bone mass and osteoporosis[2].
Considering from its clinical manifestations, PMOP falls under the category of ‘bone flaccidity’ or ‘bone Bi-Impediment’. According to traditional Chinese medicine, PMOP is closely associated with the liver, spleen and kidney. Since the liver stores blood and dominates sinews, insufficient liver-blood after menopause fails to nourish the sinews and vessels, leading to inflexible joint movement and fatigue. The liver and kidney share the same source, blood and essence can mutually transform, and liver-blood insufficiency can cause kidney essence insufficiency. Since the kidney stores essence, dominates bones and generates marrow, kidney essence insufficiency can result in skeletal malnourishment. In addition, since the liver also maintains free flow of qi and blood, obstructed flow of essence and blood may also cause malnourishment of the sinews, vessels and bones. The spleen is known as the acquired base (source) of qi and blood; as a result, spleen qi deficiency may also cause malnourishment of sinews and bones. What’s more, kidney qi has the functions of promoting and transforming qi of other Zang-fu organs, kidney deficiency may affect the liver and spleen. Consequently, the treatment principle for PMOP is to soothe the liver, tonify the spleen and kidney.
Acupuncture can obtain some effects for PMOP[3-6]. Laboratory studies have indicated that acupuncture could increase the BMD contents, BD and E2level in postmenopausal model rats[7-9]. Of acupoints employed in this study, Ganshu (BL 18), Pishu (BL 20) and Shenshu (BL 23), the Back-Shu acupoints of the liver, spleen and kidney, can activate essential qi of the three organs[10-11]. Recognized as a key acupoint for disease prevention and treatment, Zusanli (ST 36) regulates the spleen and stomach, nourishes qi and blood, supplements healthy qi and supports yang. Zusanli (36) and Pishu (BL 20) in combination can tonify qi and blood to supplement the congenital kidney qi. As a crossing acupoint of the Liver, Spleen and Kidney Meridians, Sanyinjiao (SP 6) regulates functions of the above three organs. Yanglingquan (GB 34), the Influential Acupoint of the sinews, benefits the sinews.Xuanzhong (GB 39), the influential acupoint of the marrow, is indicated for marrow-related problems. Taixi (KI 3), the Shu-Stream and Yuan-Primary acupoint of the Kidney Meridian, nourishes kidney yin and warms kidney yang. Taixi (KI 3) and Shenshu (BL 23) in combination supplement kidney essence. Taichong (LR 3), the Shu-Stream and Yuan-Primary acupoint of the Liver Meridian, soothes liver qi. Qimen (LR 14), the Front-Mu acupoint of the liver, when used in combination with Ganshu (BL 18), can soothe, nourish the liver and regulate qi activity. Apparently, the above acupoints can soothe the liver, tonify the spleen and reinforce the kidney, thus benefiting PMOP patients.
According to the findings of this study, after acupuncture treatment, the BD in the observation group was significantly elevated (P<0.05), showing a statistical significance between the two groups (P<0.05) and thus indicating a better effect of acupuncture for BD elevation. The E2levels in both groups were increased after treatment (P<0.01), showing no statistical significance between the two groups (P>0.05) and indicating that acupuncture and oral calcium tablets containing vitamin D can both increase the E2level. Previous studies have also proven that supplementing vitamin D in ovary tissue culture in vitro could stimulate the secretion of estrogen; however, further study is needed for the effect of supplementing vitamin D on human E2level[12].
In summary, the action mechanism of acupuncture for PMOP might be associated with its effects in elevating E2level, inhibiting hyperactive bone remodeling, thus restoring normal bone metabolism, increasing the BD and relieving clinical symptoms. Unlike estrogen-replacement therapy that may cause adverse reactions after long-term use, acupuncture can be an effective non-drug therapy for the prevention and treatment of senile osteoporosis.
[1] Ministry of Health of the People’s Republic of China. Guiding Principles for Clinical Study of New Chinese Medicines. Beijing: China Medico-Pharmaceutical Science & Technology Publishing House, 2002: 357-360.
[2] Zhao LH, Nong ZN, Zhong X, Pang Y, Liang JS, Su XD, Ye FW. Effects of warm needle moxibustion on bone mass density and biochemical indexes of bone metabolism in patients of postmenopausal osteoporosis. Zhongguo Zhenjiu, 2008, 28(12): 897-900.
[3] Ji F, Li P. Clinical application and consideration of acupuncture in postmenopausal osteoporosis. Zhongguo Minjian Liaofa, 2005, 13(6): 64-65.
[4] Pang Y, Zhao LH, Nong ZN, Ye FW, Liang JS, Su XD, Zhong X, Zhang JZ, Feng Z. Clinical study of acupuncturemoxibustion treatment for primary osteoporosis. Shanghai Zhenjiu Zazhi, 2008, 27(12): 15-16.
[5] Zhou ZH, Wang NQ, Pan FF, Wu ZH, Dai XY. Clinical observation on combined acupuncture and medication for osteoporosis in postmenopausal women. J Acupunct Tuina Sci, 2011, 9(6): 370-375.
[6] Wang XY, Zhang Y, Guo F. The influences of electroacupuncture plus estrogen on bone quantity and insulin-like growth factor in ovariectomized rats. Shanghai Zhenjiu Zazhi, 2006, 25(11): 33-35.
[7] Wang H, Bao SY, Zhou XL. Influence of “doublereinforcing and one-unblocking” acupuncture on the mineral content and the density of bone and estradiol in a rat model of postmenopausal osteoporosis. Shanghai Zhenjiu Zazhi, 2005, 24(10): 39-41.
[8] Liu XX, Wu MX, Wu BH, Zhang ZA, Lin W, Zheng LP, Lin JM. Studies on effects of acupuncture and moxibustion on fracture healing in experimental osteoporotic models produced in rats. Zhongguo Gushang, 2001, 14(2): 81-82.
[9] Pan FF, Zhou ZH, Wang YP, Wang XY, Zhao LX, Chen HD. Effect of combined use of acupuncture and medicine on serum E2and bone mineral density in postmenopausal osteoporosis rats. Shanghai Zhenjiu Zazhi, 2012, 31(6): 444-446.
[10] Li CX, Zhang W. Treatment of 22 cases of chronic fatigue syndrome by puncturing Back-Shu points. J Acupunct Tuina Sci, 2010, 8(6): 368-370.
[11] Xu DK, Guo L. Therapeutic observation on the treatment of Sjogren’s syndrome by majorly needling Back-Shu points. Shanghai Zhenjiu Zazhi, 2013, 32(1): 28-29.
[12] Zhu JL, Zhang WC, Li H, Huang YJ. Effect of vitamin D3on sex hormone secretion of rat’s chipped ovaries. Zhongguo Gonggong Weisheng, 2007, 23(10): 1163-1164.
Translator: Han Chou-ping
R246.3
A
Date: March 20, 2013
Author: Du Ge-shu, associate chief physician.
E-mail: csszxyy@126.com
杂志排行
Journal of Acupuncture and Tuina Science的其它文章
- Therapeutic Efficacy Observation on Integrative Acupuncture Therapy for Chronic Urticaria
- Research Progress of Acupuncture-moxibustion for Insomnia: An Analysis of Literature in Recent 5 Years
- Treatment Frequency and Long-term Efficacy Observation on Electric Pudendal Nerve Stimulation for Stress Urinary Incontinence
- Clinical Observation on Treatment of Insomnia with Puncturing Back-Shu Acupoints
- Clinical Observation on Acupuncture for Perimenopausal Syndrome
- Clinical Observation on Deep Acupuncture at Huantiao (GB 30) for Patients with Chronic Prostatitis