Clinical Observation on Acupuncture for Perimenopausal Syndrome
2013-07-18ZhengLifangJinYabei
Zheng Li-fang, Jin Ya-bei
1 Zhejiang University of Traditional Chinese Medicine, Hangzhou 310053, China
2 Acupuncture Department, Hangzhou Red Cross Hospital, Hangzhou 310003, China
Clinical Observation on Acupuncture for Perimenopausal Syndrome
Zheng Li-fang1, Jin Ya-bei2
1 Zhejiang University of Traditional Chinese Medicine, Hangzhou 310053, China
2 Acupuncture Department, Hangzhou Red Cross Hospital, Hangzhou 310003, China
Objective: To observe the clinical efficacy of acupuncture for perimenopausal syndrome.
Methods: A total of 40 perimenopausal syndrome cases who met the inclusion criteria were randomized into an observation group and a control group, 20 in each group. Acupuncture combining with ginger-partitioned moxibustion was used in the observation group, whereas acupuncture was used in the control group. Modified Kupperman Index (KI) was evaluated respectively before and after treatment. In addition, the clinical efficacies in the two groups were compared.
Results: The total effective rate in the observation group was higher than that in the control group (P<0.05). After treatment, KI in both groups were significantly reduced (P<0.01) and there was a statistical difference between the two groups (P<0.01).
Conclusion: Acupuncture combining with ginger-partitioned moxibustion could obtain a higher total effective rate for perimenopausal syndrome than acupuncture alone. Furthermore, it was also superior to acupuncture alone in improving hot flushes, insomnia, melancholia and arthralgia or myalgia.
Acupuncture Therapy; Acupuncture-moxibustion Therapy; Indirect Moxibustion; Perimenopausal Syndrome; Menopausal Syndrome; Gingerpartitioned Moxibustion
Perimenopausal syndrome is mainly characterized by endocrine disorder and vegetative nerve functional disturbance. We treated 40 cases with perimenopausal syndrome with combining acupuncture with gingerpartitioned moxibustion between July 2009 and December 2010 and then compared its clinical efficacy with acupuncture alone. The results are now reported as follows.
1 Clinical Materials
1.1 Diagnostic criteria
This is based on the diagnostic criteria for menopausal syndrome stipulated in the Guiding Principles for Clinical Study of New Chinese Medicines[1].
Women aged from 45 to 55 presenting with (other than irregular menstruation) hot flush and associated symptoms such as restlessness, irritability, palpitations, insomnia, chest stuffiness, headache, mood swings, poor memory, fluctuating blood pressure and low back/leg pain; reduced estrodiol (E2) level and increased follicle stimulating hormone (FSH) and luteinizing hormone (LH).
1.2 Inclusion criteria
Those who met the above diagnostic criteria and were willing to sign the informed consent.
1.3 Exclusion criteria
Those who took sleep pills for a long period of time; those with complications of hyperthyroidism, neurosis, psychic disease, severe skin conditions or coagulation disorder; those with other systemic disease or organic reproductive system conditions.
1.4 General data
A total of 40 cases were randomly allocated into an observation group and a control group according to their visit sequences, 20 in each group. The mean age and duration of cases in the observation group were (48±6) years and (9.52±5.44) months respectively, versus (47±5) years and (8.86±5.67) months in the control group. There were no between-group statistical differences in age and duration (P>0.05). Therefore, the two groups are comparable.
The clinical managements of the two groups are shown in Fig.1.
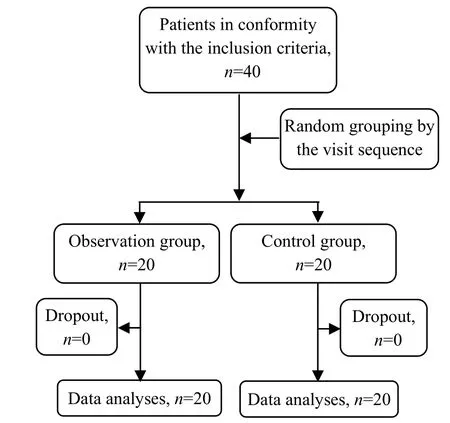
Fig.1 Clinical management flow chart
2 Treatment Methods
2.1 Observation group
Cases in the observation group were treated with combining acupuncture with ginger-partitioned moxibustion.
Acupoints: Zhongwan (CV 12), Xiawan (CV 10), Qihai (CV 6), Guanyuan (CV 4), Qixue (KI 13), Siman (KI 14), Taixi (KI 3), Taichong (LR 3), Sanyinjiao (SP 6) and Shenque (CV 8).
Methods: After routine disinfection, puncture all acupoints except for Shenque (CV 8) perpendicularly using filiform needles of 0.25 mm in diameter and 40 mm in length. Upon arrival of qi, apply 1-minute even twirling (twirling speed: 60 r/min; twirling amplitude: 360°) and retain the needles for 30 min. Regarding ginger-partitioned moxibustion, place fresh ginger slice of 5 cm in diameter and 2 cm in thickness over Shenque (CV 8), then place a moxa cone of 3 cm in diameter and 3 cm in height on the fresh ginger slice and ignite the moxa cone. When one cone was burnt out (1 cone), remove the ash and replace another one (2 cones in total). The treatment was conducted once every day, 5 times a week and 20 times made up one course of treatment.
2.2 Control group
The cases in the control group were treated with acupuncture alone using the same acupoints, method and course of treatment as the observation group.
3 Treatment Results
3.1 Therapeutic efficacy criteria
The therapeutic efficacy was evaluated using the modified Kupperman scoring standard[2]. Kupperman Index (KI) is a numerical index that scores menopausal symptoms.
KI ratio=Post-treatment KI/Pre-treatment KI×100%.
Marked effectiveness: MI ratio <25%.
Improvement: MI ratio≥25% but ≤80%.
Failure: MI ratio>80%.
3.2 Statistical method
The SPSS 11.5 version statistical software was used for statistical management. The t-test for measurement data (expressed with) and Chi-square test for numeration data.
3.3 Treatment outcomes
3.3.1 Between-group clinical efficacy comparison
There was a between-group statistical difference in total effective rate (P<0.05), indicating that combining acupuncture with ginger-partitioned moxibustion could obtain better overall response rate than acupuncture alone (table 1).
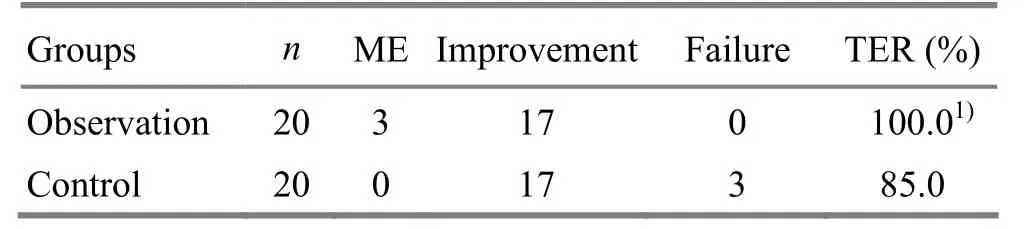
Table 1. Between-group clinical efficacy comparison (case)
3.3.2 Between-group KI comparison before and after treatment
After treatment, KI in both groups were significantly reduced (P<0.01) and there was statistical difference between the two groups (P<0.01), (table 2).
3.3.3 Between-group symptom scoring comparison before and after treatment
After treatment, cases in the observation group showed significant improvement in hot flushes, insomnia, nervousness, melancholia, arthralgia or myalgia, vertigo, weakness and palpitations (P<0.01 or P<0.05); cases in the control group showed significant improvement in hot flushes, insomnia, nervousness, melancholia and arthralgia or myalgia (P<0.01 or P<0.05); and there were between-group statistical differences in hot flushes, insomnia, melancholia and arthralgia or myalgia (P<0.05), (table 3).
Table 2. Between-group KI comparison before and after treatment (, point)
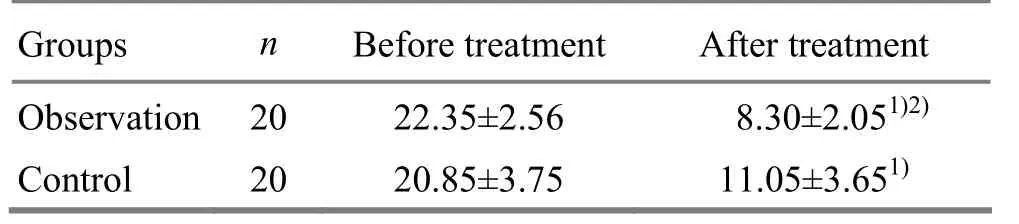
Table 2. Between-group KI comparison before and after treatment (, point)
Note: Compared with the intra-group results before treatment, 1) P<0.01; compared with the control group, 2) P<0.01
Observation 2022.35±2.56 8.30±2.051)2)Control 2020.85±3.75 11.05±3.651)
Table 3. Between-group symptom scoring comparison before and after treatment (, point)
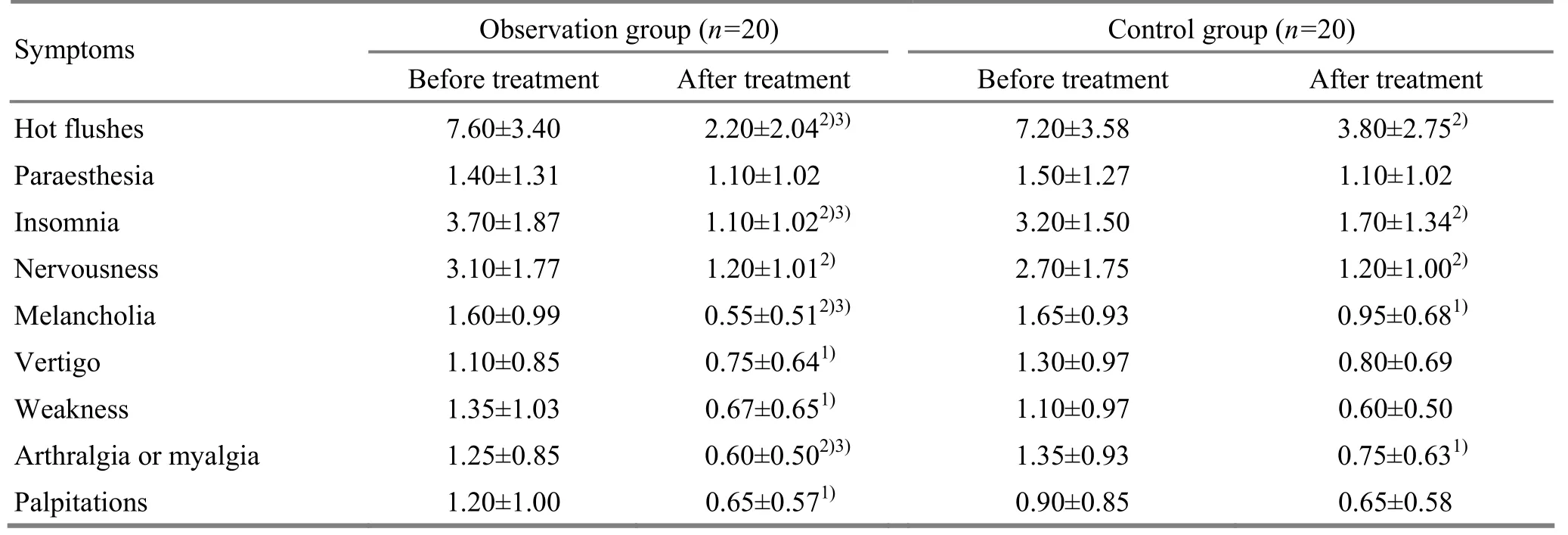
Table 3. Between-group symptom scoring comparison before and after treatment (, point)
Note: Compared with the intra-group results before treatment, 1) P<0.05, 2) P<0.01; compared with the control group, 3) P<0.05
Symptoms Observation group (n=20) Control group (n=20) Before treatment After treatment Before treatment After treatment Hot flushes 7.60±3.40 2.20±2.042)3)7.20±3.58 3.80±2.752)Paraesthesia 1.40±1.31 1.10±1.02 1.50±1.27 1.10±1.02 Insomnia 3.70±1.87 1.10±1.022)3)3.20±1.50 1.70±1.342)Nervousness 3.10±1.77 1.20±1.012)2.70±1.75 1.20±1.002)Melancholia 1.60±0.99 0.55±0.512)3)1.65±0.93 0.95±0.681)Vertigo 1.10±0.85 0.75±0.641)1.30±0.97 0.80±0.69 Weakness 1.35±1.03 0.67±0.651)1.10±0.97 0.60±0.50 Arthralgia or myalgia 1.25±0.85 0.60±0.502)3)1.35±0.93 0.75±0.631)Palpitations 1.20±1.00 0.65±0.571)0.90±0.85 0.65±0.58
4 Discussion
In Chinese medicine, perimenopausal syndrome develops with gradual declining of kidney qi, almost exhaustion of Tiangui (congenital kidney essence), deficiency of the Thoroughfare and Conception Vessels, loss of reproductive function, dysfunctions of the Zang-fu organs and disordered qi, blood, yin and yang[3]. As a result, the important principle of treatment is to balance kidney yin and yang. Sanyinjiao (SP 6) benefits the liver, spleen and kidney, regulates qi, circulates blood, nourishes the Thoroughfare and Conception Vessels and restores yin-yang balance. Zhongwan (CV 12) and Xiawan (CV 10) regulate qi ascending and descending of the spleen and stomach. Qihai (CV 6) and Guanyuan (CV 4) tonify qi and consolidate the congenital base. The four acupoints in combination can warm and nourish the Thoroughfare and Conception Vessels, supplement essence-blood, harmonize qi and blood and balance yin and yang. Qixue (KI 13), Taixi (KI 3) and Taichong (LR 3)tonify the kidney and soothe liver qi. Pungent and warm in nature and flavor, fresh ginger circulates qi and blood and relieves the exterior. Ginger-partitioned moxibustion on Shenque (CV 8) warms and tonifies the spleen and kidney and regulates the Thoroughfare and Conception Vessels.
According to our study findings, cases in both groups got significant relief in hot flushes, insomnia and nervousness; however, combining acupuncture with ginger-partitioned moxibustion was superior to acupuncture alone in improving symptoms such as hot flushes, insomnia, melancholia and arthralgia or myalgia, indicating that ginger-partitioned moxibustion is associated with the between-group therapeutic efficacy difference. Ineffectiveness of both groups in paraesthesia might be related to selection of acupoints and course of acupuncture treatment. Since combining acupuncture with ginger-partitioned moxibustion can markedly reduce the KI in patients with menopausal syndrome, it is an effective therapy for perimenopausal syndrome (100% overall response rate). Previous clinical and laboratory studies have proven that acupuncture can stimulate and promote the remaining sinusoid ovarian follicle function and enhance the synthesis of estrogen[4-6]. As a result, acupuncture can effectively regulate the functions of the hypothalamicpituitary-ovarian axis, increase the hormonal stability and significantly improve menopausal symptoms[7-8]. By means of the heat effect and osmosis, ginger-partitioned moxibustion can reach all meridians, benefit the kidney, further activate meridian qi, regulate Zang-fu organs and harmonize yin and yang via the path of acupoints-meridians-Zang-fu organs[9-10], and thus relieve perimenopausal syndrome symptoms.
[1] Ministry of Health of the People’s Republic of China. Guiding Principles for Clinical Study of New Chinese Medicines. Beijing: China Medico-Pharmaceutical Science & Technology Publishing House, 1997: 98, 151.
[2] Wang SY. Practical Diagnosis and Treatment Standard for Gynecology and Obstetrics. Nanjing: Jiangsu Phoenix Science Press, 2002:120.
[3] Zhang YZ. Chinese Gynecology and Obstetrics. Beijing: China Press of Traditional Chinese Medicine, 2002: 169.
[4] Li Y, Xia Y, Liu SM, Ju ZY, Shi XL, Chen MG, He JS. Effect of electroacupuncture on Kupperman index scores in patients with perimenopausal syndrome. Shanghai Zhenjiu Zazhi, 2009, 28(10): 559-561.
[5] Zhou Q, Wang JX. Clinical observation on acupuncture for perimenopausal melancholia. J Acupunct Tuina Sci, 2009, 7(4): 200-202.
[6] Li Y, Ju ZY, Xia Y, Liu SM, Shi XL, He JS. Study of the effect of electroacupuncture in a rat model of perimenopausal melancholia. Shanghai Zhenjiu Zazhi, 2010, 29(10): 670-673.
[7] Li Y, Xia Y, Liu SM, Ju ZY, Shi XL, Chen MG, Cheng L, He JS. Clinical study on electroacupuncture for perimenopause syndrome. J Acupunct Tuina Sci, 2011, 9(5): 278-282.
[8] Che P, Zhao H, Chen BY. Ectopic expression of GnRH during natural compensation of HPOA function and the effect of electroacupuncture on it in ovariectomized rats. Shanghai Zhenjiu Zazhi, 2007, 26(11): 39-42.
[9] Zhou YL, Li J. Survey on clinical and basic study on perimenopausal syndrome treated by moxibustion. J Acupunct Tuina Sci, 2009, 7(5): 315-320.
[10] Qian XL, Bao CL, Hou WG, Zhou YL, Li J. Effect of cake-partitioned moxibustion on integral of climacteric syndrome patients. Jiangsu Zhongyiyao, 2010, 42(9): 47-48.
Translator: Han Chou-ping
R246.3
A
Date: March 15, 2013
Author: Zheng Li-fang, M.M.
E-mail: hhrsk303@163.com
杂志排行
Journal of Acupuncture and Tuina Science的其它文章
- Therapeutic Efficacy Observation on Integrative Acupuncture Therapy for Chronic Urticaria
- Research Progress of Acupuncture-moxibustion for Insomnia: An Analysis of Literature in Recent 5 Years
- Treatment Frequency and Long-term Efficacy Observation on Electric Pudendal Nerve Stimulation for Stress Urinary Incontinence
- Clinical Observation on Treatment of Insomnia with Puncturing Back-Shu Acupoints
- Therapeutic Efficacy Observation on Acupuncture for Postmenopausal Osteoporosis
- Clinical Observation on Deep Acupuncture at Huantiao (GB 30) for Patients with Chronic Prostatitis