Therapeutic Efficacy Observation on Integrative Acupuncture Therapy for Chronic Urticaria
2013-07-18ZhangFuqingLiZhiyuanJiJun
Zhang Fu-qing, Li Zhi-yuan, Ji Jun
1 Shanghai Research Institute of Acupuncture and Meridian, Shanghai 200030, China
2 Fulintang Clinic of Traditional Chinese Medicine, Haicang District, Xiamen, Fujian 361026, China
Therapeutic Efficacy Observation on Integrative Acupuncture Therapy for Chronic Urticaria
Zhang Fu-qing1, Li Zhi-yuan2, Ji Jun1
1 Shanghai Research Institute of Acupuncture and Meridian, Shanghai 200030, China
2 Fulintang Clinic of Traditional Chinese Medicine, Haicang District, Xiamen, Fujian 361026, China
Objective: To observe the clinical effect of comprehensive acupuncture therapy for chronic urticaria.
Methods: A total of 70 patients with chronic urticaria were treated with acupuncture, bloodletting after pricking and cupping [on Shenque (CV 8)]. The changes of signs and symptoms were observed before and after treatment. The therapeutic efficacy was then assessed according to the change rate of clinical symptoms scoring.
Results: After treatment, 11 of the 70 cases got basic recovery, 21 cases got marked effectiveness, 27 cases got improvement and 11 cases got no effect. The total effective rate was 84.3%. There was statistical significance in symptoms score between before and after treatment (P<0.01).
Conclusion: Combining acupuncture, bloodletting after pricking and cupping on Shenque (CV 8) is effective for chronic urticaria.
Acupuncture-moxibustion Therapy; Urticaria; Pricking Blood Therapy; Cupping Therapy
According to epidemiologic studies, urticaria affects about 20 percent of people at some time during their lifetime[1]. Due to localized edema resulting from increased osmosis and dilation of small vessels in the skin or mucosa, urticaria often starts as transient itchy wheals in various sizes that can come and go. This condition can be defined as acute or chronic depending on how long it lasts. Approximately 10% of the acute urticaria patients may develop into chronic urticaria after more than six weeks[2-4]. With its complex pathogenesis and protracted duration, chronic urticaria can greatly affect the patients’ daily living and mental state. We have treated 70 cases with acupuncture combining with cupping and bloodletting therapy, and now report the result as follows.
1 Clinical Materials
1.1 Diagnostic criteria
This is based on the diagnostic criteria stipulated in the Clinical Pathway for Urticaria [WBYZF (2010) No. 190] by the Ministry of Health of the People’s Republic of China.
Wheals (skin rashes) in various sizes and shapes that suddenly appear and disappear; single skin lesion lasts no more than 24 h and leaves no trace after disappearance; skin rashes tend to migrate, coupled with itching (mild, moderate or severe) or irritation; accompanied symptoms may include chest stuffiness, difficulty breathing, nausea, vomiting, abdominal pain, diarrhea and fever; the condition lasts more than 6 weeks.
1.2 Inclusion criteria
Those who met the above diagnostic criteria; aged from 18 to 65 years old; willing to complete the treatment, accept telephone follow-up and sign the informed consent.
1.3 Exclusion criteria
Those who failed to meet the above diagnostic or inclusion criteria; patients with acute urticaria, cholinergic urticaria, cold urticaria, and solar urticaria; those fainted from needling or refused to accept acupuncture treatment; women during pregnancy or lactation; those with a history of mental disorders; those with complications of other major diseases; and those who used corticosteroid hormone over the past 1 month.
1.4 General materials
Of 70 outpatients treated in Shanghai Research Institute of Acupuncture and Meridian between January 2010 and October 2012, there were 32 males and 38 females. They aged from 27 to 48 years old (mean age: 37.5) and their disease lasted from 8 months to 11 years (mean duration: 6.6 years).
2 Treatment Methods
2.1 Acupuncture
Major acupoints: Quchi (LI 11), Waiguan (TE 5), Hegu (LI 4), Xuehai (SP 10), Zusanli (ST 36) and Sanyinjiao (SP 6)
Adjunct acupoints: Neiguan (PC 6) was added for chest stuffiness; Zhongwan (CV 12) and Tianshu (ST 25) were added for abdominal pain and diarrhea.
Method: Ask the patient to take a supine position and disinfect the local area, and then puncture the above acupoints using filiform needles of 0.25 mm in diameter and 25-40 mm in length. Even reinforcingreducing manipulations are applied after arrival of needling sensation (qi). Retain the needles for 30 min and manipulate them every 10 min.
2.2 Cupping
Apply cupping to Shenque (CV 8) and retain the cup for 5 min.
2.3 Bloodletting after pricking using a plum-blossom needle
Disinfect the surrounding area of Geshu (BL 17) on both sides, tap the local area using a plum-blossom needle (gradually increased force) until the skin slightly bleed. Then apply cupping to the bilateral acupoints and retain the cups for 10 min.
The above combined therapy was conducted 3 times a week. Improvements of clinical symptoms were observed after 6-week treatments. A follow-up was conducted 6 months after treatment to track the relapse rate.
3 Treatment Results
3.1 Scoring rating scale of signs and symptoms
This is based on the rating scale of signs and symptoms used in the Clinical Trial on Fexofenadine Hydrochloride Capsules for Chronic Idiopathic Urticaria and Allergic Rhinitis (phase III drug trial). The main observation indexes and scoring are shown in table 1.

Table 1. Clinical observation indexes and scoring
3.2 Criteria for therapeutic efficacy
This is also based on the scoring criteria for therapeutic efficacy in the Clinical Trial on Fexofenadine Hydrochloride Capsules for Chronic Idiopathic Urticaria and Allergic Rhinitis (phase III drug trial). The therapeutic efficacy was then assessed according to the improvement degree of the total scores of signs and symptoms after treatment.
Basic recovery: The score of clinical symptoms was reduced by over 90%.
Marked effectiveness: The score of clinical symptoms was reduced by 60% or more but less than 90%.
Improvement: The score of clinical symptoms was reduced by 20% or more but less than 60%.
Failure: The score of clinical symptoms was reduced by less than 20%.
3.3 Statistical method
The paired sample t-test was used for measurement data, Chi-square test for numeration data and P<0.05indicated a statistical significance.
3.4 Treatment outcome
3.4.1 Observation on symptoms scores before and after treatment
After treatment, both clinical signs and symptoms were significantly improved, showing a statistical significance (P<0.01), (table 2).
3.4.2 Therapeutic efficacy
Of the 70 cases, 11 got basic recovery, 21 got marked effectiveness, 27 got improvement and 11 got no effect. The total effective rate was 84.3%.
3.4.3 Follow-up results
Telephone follow-up was conducted on cases with basic recovery and marked effectiveness 6 months after treatment to observe the relapse rates. The results showed that 4 cases experienced one mild relapse that did not appear after disappearance and had no interference with daily living; and 1 case experienced moderate tolerable relapse that did not appear after disappearance. The relapse rate was 15.6%.
Table 2. Comparison of signs & symptoms scoring before and after treatment (, point)
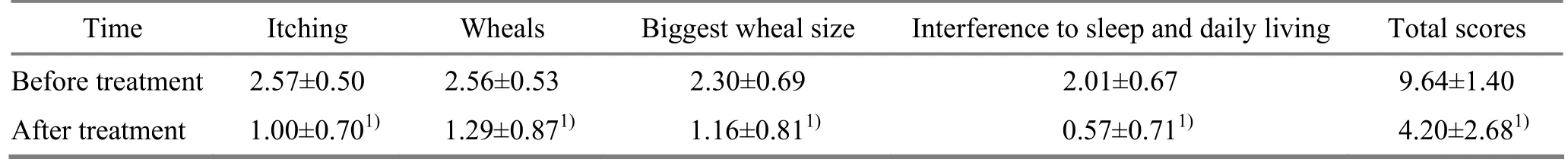
Table 2. Comparison of signs & symptoms scoring before and after treatment (, point)
Note: Compared with the pre-treatment results, 1) P<0.01
Time Itching Wheals Biggest wheal size Interference to sleep and daily living Total scores Before treatment 2.57±0.50 2.56±0.53 2.30±0.69 2.01±0.67 9.64±1.40 After treatment 1.00±0.701)1.29±0.871)1.16±0.811)0.57±0.711)4.20±2.681)
4 Discussion
In modern medicine, urticaria is caused by functional disorder of immune or non-immune mechanism and subsequent excessive release of histamine and other mediators of inflammation, followed by itching wheals (or hives). As the first-line therapy for patients with chronic urticaria, histamine H1receptor antagonists are extensively used for their accurate efficacies. However, these antagonists may cause adverse reactions such as a dry mouth, somnolence, drug resistance over time and relapse after drug discontinuance. As a result, the research priority is to find a safe and effective treatment protocol that can minimize adverse reactions and relapses[5-8].
There were no recorded documents of chronic urticaria in Chinese medicine, however, according to description of ‘migratory itching wheals that come and go’, it falls under the category of ‘hidden rashes’ and‘wind rashes or itching sores’ in ancient Chinese medical literature. Considering from its protraction and relapses, chronic urticaria can be diagnosed as mixed deficiency (the root cause) and excess (symptoms)[3-4]. Deficiency of healthy qi and dysfunctions of the Zang-fu organs are root cause of this condition, six external pathogenic factors and improper diet can be the inducing factors. Numerous studies have proven that acupuncture can regulate the Zang-fu functions, supplement qi, strengthen the spleen (the acquired base), circulate blood, remove wind and thus alleviate itching. On the basis of ancient literature regarding acupuncture for ‘hidden rashes’ and publications regarding acupuncture for chronic urticaria between 2000 and 2010 as well as ‘with sufficient healthy qi inside the body, pathogenic factors will have no way to invade the body’ and ‘treating from the blood to dispel wind, wind stops spontaneously after blood circulates normally’ in Chinese medical theory, acupoints in this trial are selected according to syndrome, symptoms and experience[4]. For example, Hegu (LI 4), Zusanli (ST 36) and Sanyinjiao (SP 6) regulate dysfunctions of the spleen and stomach; Geshu (BL 17) (bloodletting and cupping), Quchi (LI 11), Waiguan (TE 5) and Xuehai (SP 10) circulate blood, dispel wind, consolidate the exterior and relieve itching wheals; Neiguan (PC 6) alleviates chest tightness and difficulty breathing; and cupping on Shenque (CV 8) facilitates the effect of dispelling wind to relieve itching[9-10]. Consequently, the combined acupoints obtained a satisfactory effect.
[1] Zhao B. Clinical Dermatology. 3rd Edition. Nanjing: Jiangsu Science & Technology Press, 2006: 613.
[2] Wang XS, Liao KH, Yang GL. Dermatology. Shanghai: Science and Technical Literature Press, 2005: 406.
[3] Geng P, Tian YH, Lin ZJ, Wang GF, Wang SY. Therapeutic effect observations on treatment of urticaria with acupuncture plus garlic-partitioned moxibustion. J AcupunctTuina Sci, 2004, 2(1): 44-45.
[4] Li ZY, Ji J, Xu J. Analysis and prospect on acupuncture for chronic urticaria. Shanghai Zhenjiu Zazhi, 2012, 31(5): 360-364.
[5] Chow SK. Management of chronic urticaria in Asia: 2010 AADV consensus guidelines. Asia Pac Allergy, 2012, 2(2): 149-160.
[6] Zuberbier T. Chronic urticaria. Curr Allergy Asthma Rep, 2012, 12(4): 267-272.
[7] Ferrer M, Sastre J, Jáuregui I, Dávila I, Montoro J, del Curvillo A, Mullol J, Bartra J, Valero A. Effect of antihistamine up-dosing in chronic urticaria. J Investiq Allergol Clin Immunol, 2011, 21(Suppl): 34-39.
[8] Ue AP, Souza PK, Rotta O, Furlani Wde J, Lima AR, Sabbag DS. Quality of life assessment in patients with chronic urticaria. An Bras Dermatol, 2011, 86(5): 897-904.
[9] Liao XQ, Xiao P. Therapeutic efficacy observation on bloodletting Quchi (LI 11) for chronic urticaria. Shanghai Zhenjiu Zazhi, 2012, 31(2): 119-121.
[10] Wang YJ, Chai WH, Wang HR, Wu ZQ. Clinical observation on thunder-fire moxibustion for chronic urticaria. Shanghai Zhenjiu Zazhi, 2012, 31(2): 107-109.
Translator: Han Chou-ping
R246.7
A
Date: February 26, 2013
Author: Zhang Fu-qing, M.M., research assistant
Ji Jun, M.D., associate researcher.
E-mail: jijunmm@126.com
杂志排行
Journal of Acupuncture and Tuina Science的其它文章
- Research Progress of Acupuncture-moxibustion for Insomnia: An Analysis of Literature in Recent 5 Years
- Treatment Frequency and Long-term Efficacy Observation on Electric Pudendal Nerve Stimulation for Stress Urinary Incontinence
- Clinical Observation on Treatment of Insomnia with Puncturing Back-Shu Acupoints
- Therapeutic Efficacy Observation on Acupuncture for Postmenopausal Osteoporosis
- Clinical Observation on Acupuncture for Perimenopausal Syndrome
- Clinical Observation on Deep Acupuncture at Huantiao (GB 30) for Patients with Chronic Prostatitis