Prognostic criteria for postoperative mortality in 170 patients undergoing major right hepatectomy
2012-06-11
Bologna,Italy
Introduction
Recent studies[1-7]have focused on identifying criteria that lead to the early detection of patients suffering from hepatic failure in order to modify the therapeutic regimen and possibly improve the recovery rate and prognosis.Postoperative hepatic failure is a dreadful complication after major hepatectomy and carries high morbidity and mortality.[4,8-10]Balzan et al[8]found that prothrombin time <50% [international normalized ratio (INR)>1.7] and a serum total bilirubin concentration >50 μmol/L (>3.0 mg/dL) on postoperative day 5 are associated with a mortality rate of 70%.[11]Mullen et al[10]identified a total bilirubin concentration>7 mg/dL in the postoperative period as an accurate predictor of death from hepatic failure.
Right hepatectomy is linked to a poor outcome with a high morbidity or mortality,[12]typically ranging from 6% to 8%.[9]As a primary endpoint of this study,we assessed the 50/50 and Mullen criteria for their ability to predict death from hepatic failure in patients undergoing right hepatectomy only.As a secondary endpoint,we aimed at identifying prognostic factors linked to intra-hospital morbidity and mortality as well as death from hepatic failure in these patients.
Methods
Demographics of patients
The charts of the patients undergoing right hepatectomy,right hepatectomy with caudate lobe resection and right extended hepatectomy from 2000 to 2008 were retrospectively reviewed at the Department of General Surgery and Organ Transplantation of the University of Bologna.One hundred and seventy consecutive patients were identified for analysis.All patients had abdominal CT scans with IV contrast preoperatively for diagnostic purposes.
Study design and endpoints
For each patient,the following were analysed:age,gender,body mass index (BMI),diagnosis at presentation,presence of cirrhosis,HBV and HCV titers,days of hospital stay,intraoperative complications,postoperative complications,positivity for either the 50/50 or Mullen criteria,[10,11]portal vein embolization,type of procedures,associated procedures,need for packed red blood cells and fresh frozen plasma transfusions as well as quantity transfused,length of procedures,need for portal triad clamping,times of triad clamping,and surgical resection margins.Moreover,INR,creatinine,bilirubin,ALT and AST before and after operation on days 1,3,5 and 10 were recorded and analysed (Fig.1).Also recorded were adjunct comorbidities at the time of surgery,including diabetes mellitus,chronic pulmonary disorders,and cardiac disease (categorized as NYHA I-IV).Cirrhosis was defined as the presence offibrosis,disruption of hepatic parenchymal structure,and presence of parenchymal microscopic or macroscopic nodules on histological examination.Categorical variables were either defined empirically or through a receiving operating characteristic (ROC) curve,in order to determine cutoffs with the highest sensitivity and specificity.These variables were subjected to univariate and multivariate analyses.
Surgical procedures
Major right hepatectomy was defined as every right hepatectomy (Couinaud's segments 5-6-7-8),every right extended hepatectomy (Couinaud's segments 5-6-7-8+4),and every right hepatectomy with caudate lobe resection(Couinaud's segments 5-6-7-8+1),as defined by the International Hepato-Pancreato-Biliary Association(Brisbane 2000).Twenty-four (14.1%) patients underwent right hepatectomy with caudate lobe resection,80 (47.1%)underwent right hepatectomy alone,and 66 (38.8%)underwent extended right hepatectomy.
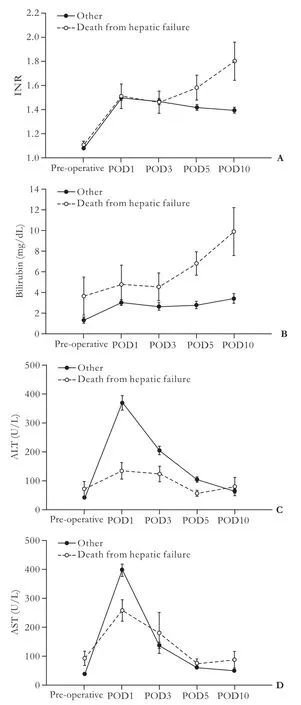
Fig.1.Pre- and post-operative INR (A),bilirubin (B),ALT (C) and AST (D) levels.POD:post-operative day.
Postoperative complications and hepatic failure
Postoperative complication was defined as any adverse event related to the surgical procedure and/or manifested within 30 days after the operation.The complication included ascites,biliaryfistulas,jaundice,hemoperitoneum or any condition requiring reoperation,renal failure,and respiratory,urinary and surgical infections.Renal failure was defined as a creatinine level >1.3 mg/dL.In patients suffering from hepatic failure that expired,the diagnosis of death from hepatic failure was based on laboratory values (INR,ammonia levels,and bilirubin) and clinical findings(encephalopathy,jaundice,and ascites).[13-19]Ascites was defined as >300 mL of abdominal fluid[20]and biliaryfistula as an abdominal fluid leak that persisted >7 days with a bilirubin concentration >5 mg/dL.[21]
Statistical analysis
Statistical analysis was conducted using SPSS 15.0(Chicago,IL.,USA).Data were expressed as percentages and mean±SD.Significance was assessed through the Chi-square test and Student's t test for univariate analysis and through logistic regression for multivariate analysis.A P value <0.05 was considered statistically significant.
Results
The demographic characteristics and intraoperative outcomes of the 170 patients included in this study are summarized in Table 1.The most common histological diagnoses were colorectal metastases,hepatocellular carcinoma and cholangiocarcinoma (Table 2).The mean hospital stay was 11.8±9.2 days,and 73 (42.9%) patients developed postoperative complications (Fig.2).Of these patients,15 (8.8%) had to undergo reoperation.Intrahospital mortality was 6.5% (11 patients),with 6 deaths due to terminal hepatic failure,1 to sepsis following ischemic necrosis of the biliary tree,1 to hemorrhage secondary to the rupture of the hepatic artery,2 to massive pulmonary embolism,and 1 to sudden death of unknown etiology.There were 4 (5.0%) deaths in patients undergoing right hepatectomy,4 (6.1%) in those undergoing extended right hepatectomy,and 3 (12.4%)in those undergoing right hepatectomy with caudate lobe resection.Nineteen patients (11.2%) were diagnosed with cirrhosis.Of these,16 were Child-Pugh class A and 3 were B,for an average Child-Pugh score of 5.6.Two of the cirrhotic patients had radiographic evidence of portal hypertension,and neither of them died postoperatively.
Of the 6 patients who died from hepatic failure,one was positive for the 50/50 criteria,and all the 6 patients were positive for the Mullen criteria (Table 3).Furthermore,5 of the 6 patients had ALT levels <188 U/L on postoperative day 1.Among the patients who did not die from hepatic failure,3 were positive for the 50/50 criteria and 22 for the Mullen criteria.When the Mullen criteria was used in cirrhotic patients on subgroup analysis,all 3 cirrhotic patients who died from hepatic failure had a bilirubin peak >7 mg/dL in the postoperative period (P<0.05).Age >65 years was also an independent predictor of intra-hospital mortality.Further,male gender was associated with an increased death rate for hepatic failure.The MELD score was not associated with intra-hospital mortality (P=0.117) nor death from hepatic failure (P=0.119) (data not shown).
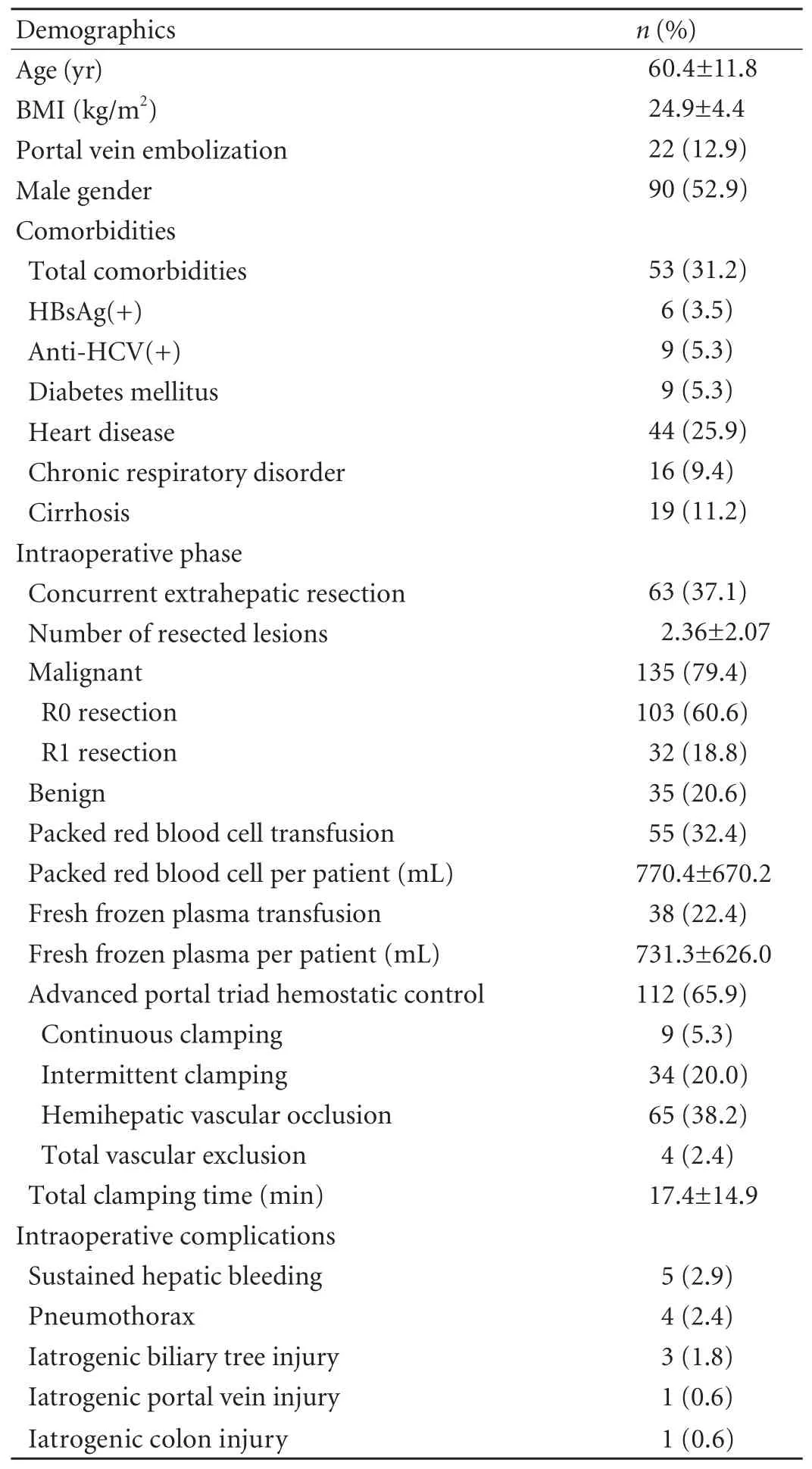
Table 1.Demographics and intraoperative results of patients
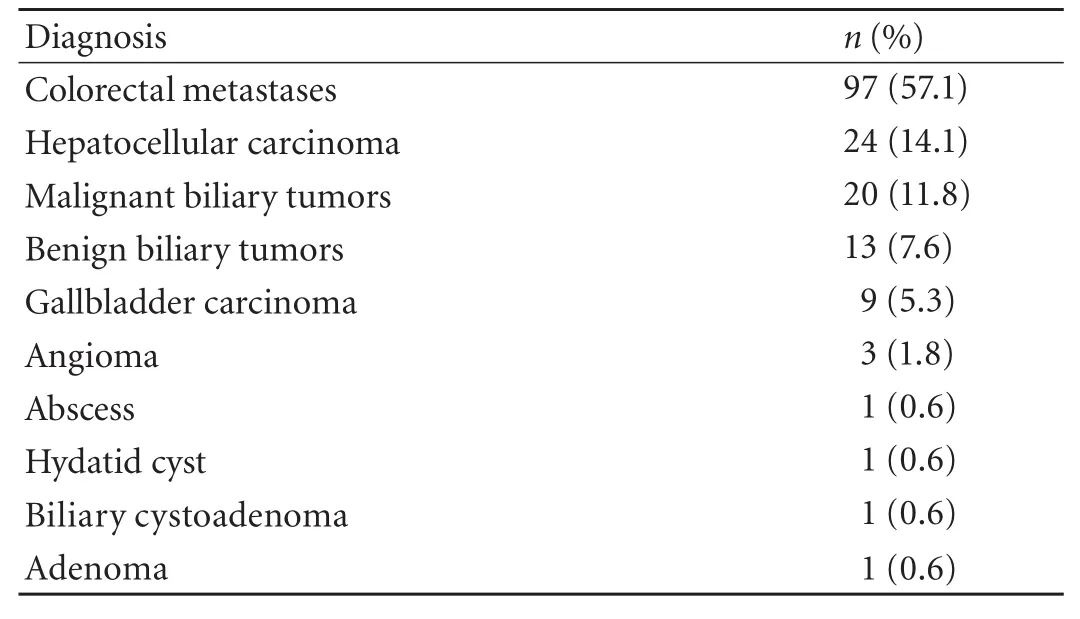
Table 2.Diagnosis of patients
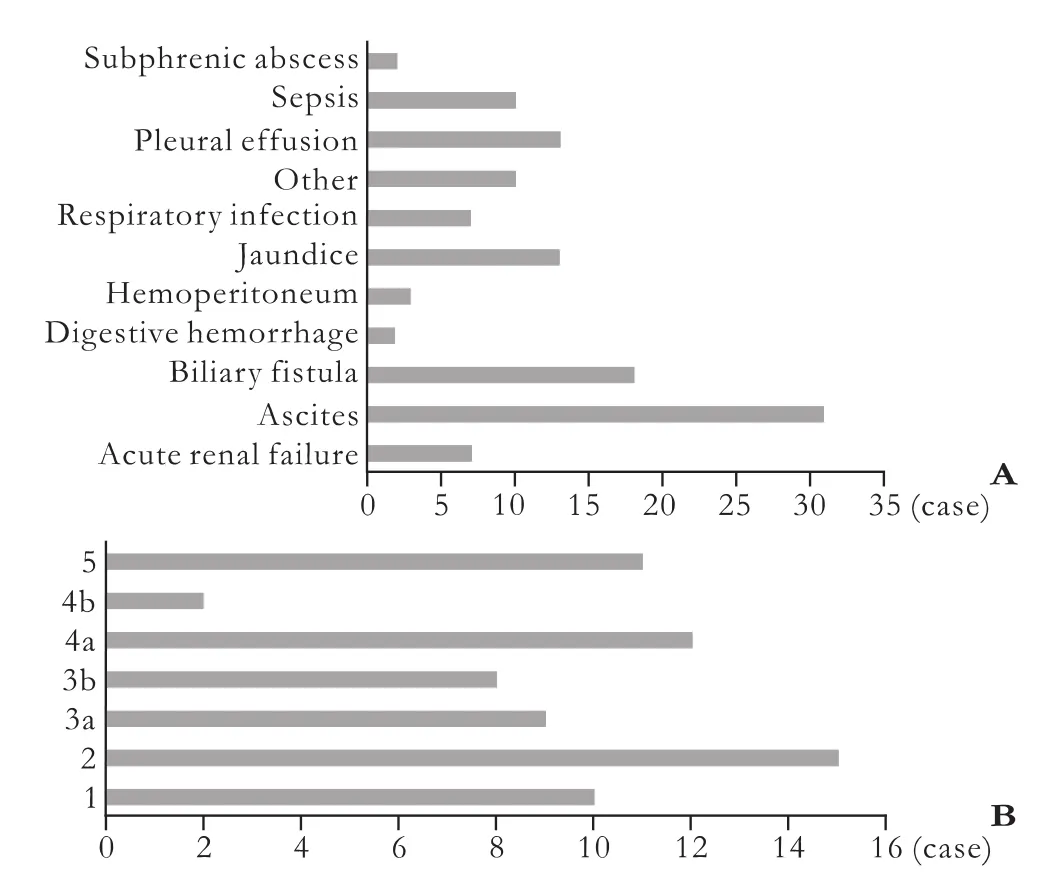
Fig.2.Postoperative complications.A:List of complications.B:Complications type according to Clavien/Dindo classification:1,2 (requiring pharmacologic treatment),3a (requiring surgical/endoscopic/radiologic intervention),3b (3a+general anesthesia),4a (single organ dysfunction+ICU admission),4b (multiple organ dysfunction+ICU admission),5 (death).
Male gender,cirrhosis,hepatitis C,hepatocellular carcinoma,development of complication,renal failure,jaundice,re-laparotomy,preoperative bilirubin level >1 mg/dL,bilirubin peak >7 mg/dL and ALT <188 U/L on postoperative day 1 were associated with death from hepatic failure on univariate analysis.Multivariate analysis showed that male gender,hepatitis C,hepatocellular carcinoma and ALT <188 U/L on postoperative day 1 were predictive of death from hepatic failure in the postoperative period.Hepatitis C,biliary and gallbladder tumors,re-laparotomy,packed red blood cell transfusion,a preoperative bilirubin >1 mg/dL,50/50 criteria and bilirubin peak >7 mg/dL were associated with morbidity on univariate analysis.Multivariateanalysis showed that bilirubin peak >7 mg/dL was a significant factor for the development of morbidity in patients undergoing right hepatectomy (Table 4).Uniand multivariate analyses for intra-hospital mortality were also assessed (data not shown).On multivariate analysis age >65 years,HCV(+),reoperation and renal failure remained as significant independent predictors of intra-hospital mortality (P<0.05).
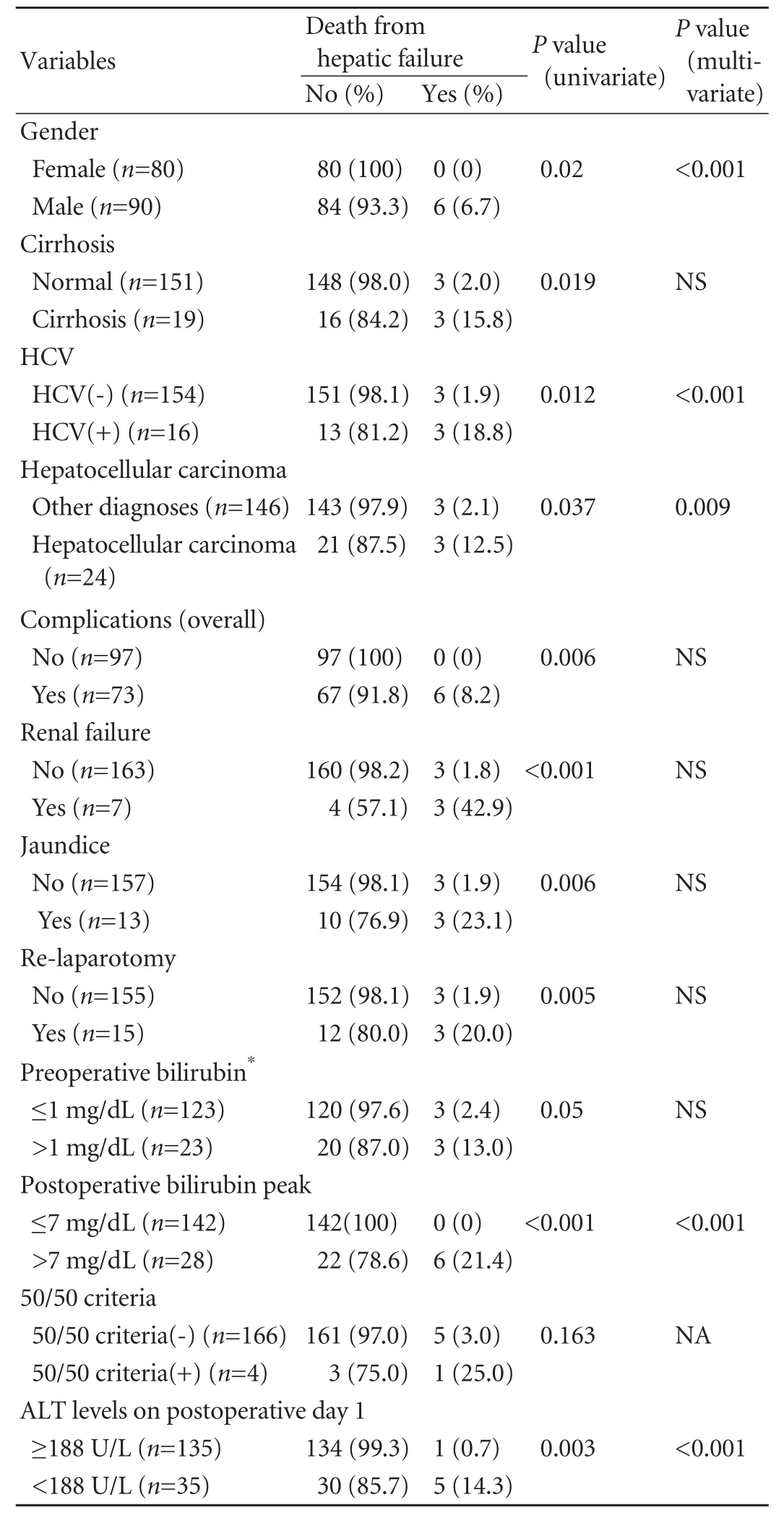
Table 3.Univariate and multivariate analysis of death from hepatic failure in 170 patients undergoing right hepatectomy

Table 4.Univariate and multivariate analyses of morbidity in 170 patients undergoing major right hepatectomy
Discussion
Hepatectomy is the standard of care for a large number of benign and malignant conditions of the liver.Efforts have been made to assess clinical parameters that could readily identify those patients at higher risk of developing hepatic failure after major hepatectomy.This phenomenon is characterized by jaundice,coagulopathy,fluid retention,encephalopathy,higher susceptibility to sepsis and ultimately death.Since patients undergoing right hepatectomy are prone to higher morbidity and mortality,[12]early identification of those who will develop terminal hepatic failure is crucial.
Balzan et al[11]found that prothrombin time <50%(INR>1.7) together with serum total bilirubin level>50 μmol/L (>3.0 mg/dL) on postoperative day 5 was associated with a mortality rate of 69.7% in patients undergoing hepatectomy.This finding was validated by a prospective review of 436 hepatectomies and it was found to be predictive for mortality on both postoperative days 3 and 5.[22]In our patient population who underwent major right hepatectomy,the 50/50 criteria were less successful since among the 6 patients who died from hepatic failure,only one was positive for the criteria.
A high yield for predicting postoperative death from hepatic failure has also been reported with the Mullen criteria (bilirubin peak >7.0 mg/dL in the postoperative period),with a sensitivity of 93% and a specificity of 94%.The result was derived through a ROC curve indicating bilirubin values and deaths from hepatic failure in 1059 non-cirrhotic patients undergoing right or left hepatectomy.[10]In our study,the Mullen criteria appeared to be reliable in predicting death from hepatic failure in patients underwent major right hepatectomy.Of the 6 patients who died from hepatic failure,all were positive for the Mullen criteria (100%).The se findings suggest that the Mullen criteria is superior to the 50/50 criteria for predicting death from hepatic failure in patients undergoing right hepatectomy.
Furthermore,our study confirmed that a bilirubin peak >7.0 mg/dL was an independent predictor of death from hepatic failure and intra-hospital morbidity.Interestingly,we found a strong association between a low ALT level on postoperative day 1 and death from hepatic failure.ROC analysis showed that ALT levels<188 U/L on postoperative day 1 were predictive of death from hepatic failure with a sensitivity of 79%,a specificity of 83% and a positive predictive value of 0.17.Patients with ALT levels <188 U/L on postoperative day 1 were more likely to die from hepatic failure as shown by multivariate analysis (P=0.003).However,it is hard to interpret the pathophysiological significance of this finding.Transaminase release is in fluenced by clamping time[23]and is significantly lower in patients suffering from liver cirrhosis.[24]In our patients,however,no significant differences were observed in clamping time between patients with ALT levels <188 U/L and those with ALT levels ≥188 U/L,nor our patient population contained a significantly higher number of cirrhotic patients.Possibly a smaller liver remnant after surgery released fewer enzymes into the systemic circulation.Unfortunately,we could not confirm this hypothesis since postoperative volumetric data on the patients with ALT levels <188 U/L were not available in our retrospective review.Although this finding is limited by the size of patients,ALT levels <188 U/L may be an early postoperative factor for predicting mortality in patients undergoing major hepatectomy.Hence,larger trials are needed to confirm the value of low ALT levels in the clinical setting.The major limitations of this study include retrospective nature,small sample size and inability to include a larger cohort of cirrhotic patients.
In summary,the Mullen criteria can accurately predict death from hepatic failure in patients undergoing major right hepatectomy.A bilirubin level >7 mg/dL in the postoperative period,HCV positivity,hepatocellular carcinoma and a ALT level <188 U/L on postoperative day 1 are associated with death from hepatic failure in such patients.
Acknowledgment:We thank Dr.Thomas J Fahey III and Dr.Rasa Zarnegar from Weill Cornell Medical College for help during the drafting of the manuscript.
Contributors:FF and GGL conceived the study and wrote the draft.FF,ZM and SF collected the data and performed the statistical analysis.All authors interpreted the data,gave critical inputs to the draft and revised the manuscript.FF is the guarantor.
Funding:None.
Ethical approval:Not needed.
Competing interest:No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
1 Child CG,Turcotte JG.Surgery and portal hypertension.Major Probl Clin Surg 1964;1:1-85.
2 Cucchetti A,Ercolani G,Vivarelli M,Cescon M,Ravaioli M,La Barba G,et al.Impact of model for end-stage liver disease (MELD) score on prognosis after hepatectomy for hepatocellular carcinoma on cirrhosis.Liver Transpl 2006;12:966-971.
3 Ercolani G,Grazi GL,Callivà R,Pierangeli F,Cescon M,Cavallari A,et al.The lidocaine (MEGX) test as an index of hepatic function:its clinical usefulness in liver surgery.Surgery 2000;127:464-471.
4 Kishi Y,Abdalla EK,Chun YS,Zorzi D,Madoff DC,Wallace MJ,et al.Three hundred and one consecutive extended right hepatectomies:evaluation of outcome based on systematic liver volumetry.Ann Surg 2009;250:540-548.
5 Malinchoc M,Kamath PS,Gordon FD,Peine CJ,Rank J,ter Borg PC.A model to predict poor survival in patients undergoing transjugular intrahepatic portosystemic shunts.Hepatology 2000;31:864-871.
6 Mullin EJ,Metcalfe MS,Maddern GJ.How much liver resection is too much? Am J Surg 2005;190:87-97.
7 Teh SH,Sheppard BC,Schwartz J,Orloff SL.Model for End-stage Liver Disease score fails to predict perioperative outcome after hepatic resection for hepatocellular carcinoma in patients without cirrhosis.Am J Surg 2008;195:697-701.
8 Balzan S,Belghiti J,Farges O,Ogata S,Sauvanet A,Delefosse D,et al.The "50-50 criteria" on postoperative day 5:an accurate predictor of liver failure and death after hepatectomy.Ann Surg 2005;242:824-829.
9 Jarnagin WR,Gonen M,Fong Y,DeMatteo RP,Ben-Porat L,Little S,et al.Improvement in perioperative outcome after hepatic resection:analysis of 1,803 consecutive cases over the past decade.Ann Surg 2002;236:397-407.
10 Mullen JT,Ribero D,Reddy SK,Donadon M,Zorzi D,Gautam S,et al.Hepatic insufficiency and mortality in 1059 noncirrhotic patients undergoing major hepatectomy.J Am Coll Surg 2007;204:854-864.
11 Balzan S,Nagarajan G,Farges O,Galleano CZ,Dokmak S,Paugam C,et al.Safety of liver resections in obese and overweight patients.World J Surg 2010;34:2960-2968.
12 Aloia TA,Fahy BN,Fischer CP,Jones SL,Duchini A,Galati J,et al.Predicting poor outcome following hepatectomy:analysis of 2313 hepatectomies in the NSQIP database.HPB(Oxford) 2009;11:510-515.
13 Parikh AA,Gentner B,Wu TT,Curley SA,Ellis LM,Vauthey JN.Perioperative complications in patients undergoing major liver resection with or without neoadjuvant chemotherapy.J Gastrointest Surg 2003;7:1082-1088.
14 Kimura F,Itoh H,Ambiru S,Shimizu H,Togawa A,Yoshidome H,et al.Circulating heat-shock protein 70 is associated with postoperative infection and organ dysfunction after liver resection.Am J Surg 2004;187:777-784.
15 Nagino M,Nishio H,Ebata T,Yokoyama Y,Igami T,Nimura Y.Intrahepatic cholangiojejunostomy following hepatobiliary resection.Br J Surg 2007;94:70-77.
16 Pawlik TM,Olino K,Gleisner AL,Torbenson M,Schulick R,Choti MA.Preoperative chemotherapy for colorectal liver metastases:impact on hepatic histology and postoperative outcome.J Gastrointest Surg 2007;11:860-868.
17 Reddy SK,Morse MA,Hurwitz HI,Bendell JC,Gan TJ,Hill SE,et al.Addition of bevacizumab to irinotecan- and oxaliplatin-based preoperative chemotherapy regimens does not increase morbidity after resection of colorectal liver metastases.J Am Coll Surg 2008;206:96-106.
18 Zorzi D,Chun YS,Madoff DC,Abdalla EK,Vauthey JN.Chemotherapy with bevacizumab does not affect liver regeneration after portal vein embolization in the treatment of colorectal liver metastases.Ann Surg Oncol 2008;15:2765-2772.
19 Rahbari NN,Garden OJ,Padbury R,Brooke-Smith M,Crawford M,Adam R,et al.Posthepatectomy liver failure:a definition and grading by the International Study Group of Liver Surgery (ISGLS).Surgery 2011;149:713-724.
20 Moore KP,Wong F,Gines P,Bernardi M,Ochs A,Salerno F,et al.The management of ascites in cirrhosis:report on the consensus conference of the International Ascites Club.Hepatology 2003;38:258-266.
21 Imamura H,Seyama Y,Kokudo N,Maema A,Sugawara Y,Sano K,et al.One thousandfifty-six hepatectomies without mortality in 8 years.Arch Surg 2003;138:1198-1206.
22 Paugam-Burtz C,Janny S,Delefosse D,Dahmani S,Dondero F,Mantz J,et al.Prospective validation of the "fifty-fifty"criteria as an early and accurate predictor of death after liver resection in intensive care unit patients.Ann Surg 2009;249:124-128.
23 Isozaki H,Adam R,Gigou M,Szekely AM,Shen M,Bismuth H.Experimental study of the protective effect of intermittent hepatic pedicle clamping in the rat.Br J Surg 1992;79:310-313.
24 Sugiyama Y,Ishizaki Y,Imamura H,Sugo H,Yoshimoto J,Kawasaki S.Effects of intermittent Pringle's manoeuvre on cirrhotic compared with normal liver.Br J Surg 2010;97:1062-1069.
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- High-intensity focused ultrasound ablation as a bridging therapy for hepatocellular carcinoma patients awaiting liver transplantation
- Effect of endogenous hypergastrinemia on gallbladder volume and ejection fraction in patients with autoimmune gastritis
- Expression of HBx protein in hepatitis B virusinfected intrahepatic cholangiocarcinoma
- Laparoscopic distal pancreatectomy with or without splenectomy:spleen-preservation does not increase morbidity
- Xanthogranulomatous cholecystitis mimicking gallbladder cancer and causing obstructive cholestasis
- Disease spectrum and use of cholecystolithotomy in gallstone ileus