Xanthogranulomatous cholecystitis mimicking gallbladder cancer and causing obstructive cholestasis
2012-06-11
Boston,USA
Introduction
Xanthogranulomatous cholecystitis (XGC) is a rare in flammatory disease of the gallbladder characterized by abnormal thickening of the wall,intense acute and chronic in flammation,severe proliferativefibrosis with formation of multiple yellowbrown intramural nodules and foamy histiocytes.[1,2]
XGC is found in 1%-6% of cholecystectomies,most of the time in association with gallstones (91%-100%),and it affects men and women equally.The etiology is not well-known.[1,2]Direct involvement of extra-gallbladder organs and structures is not common.In some cases of XGC,extended surgical resections need to be done because it cannot be differentiated from gallbladder or bile duct adenocarcinoma.[3-13]Fewer than 10 cases which showed extensive involvement of extra-gallbladder organs and required extended surgical resections have been reported in the literature so far.These procedures included bile duct resections,segmental resections of colon or duodenum,and pancreatoduodenectomies.[4,7]
Case report
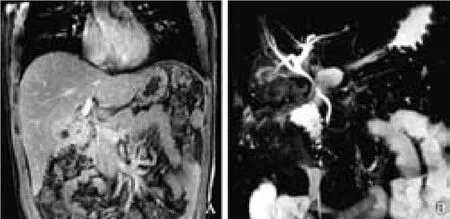
Fig.1.A:Abdominal MRI scan (cross-section coronal image)revealed an irregular thickening of the wall of the gallbladder and loss of the normal planes between the gallbladder,liver and other adjacent tissues.B:Projection image in the coronal plane 3D T2 weighted MRCP showed mild stenosis of the upper common bile duct.The cystic duct and gallbladder could not be visualized.There was no evidence of gallstones.

Fig.2.Liver specimen cut after trisegmentectomy.The gallbladder wall and surrounding liver had a hard consistency and yellow discoloration (arrows).The gallbladder mucosa was covered byfibrino-purulent exudate.
A 35-year-old Hispanic male complaining of right upper quadrant pain and jaundice for 2 months was admitted for evaluation.The pain was mild,continuous,not related to eating,and with no exacerbating or alleviating factors.He denied a history of fever,nausea/vomiting and weight loss.His medical history was relevant only for non-insulin dependent diabetes mellitus.He had no history of primary sclerosing cholangitis,no previous episodes of jaundice,and no previous operations.On physical examination,the patient was jaundiced,and all vital signs were within normal limits.The abdomen was mildly tender to deep palpation and there was no rebound tenderness.Laboratory examination revealed white blood count 8.1×109/L (neutrophils 62%,lymphocytes 20%,bands 0%),hemoglobin 12.5 g,glucose 261 mg/dL,creatinine 0.9 mg/dL,BUN 14,ALT 31 U/L,AST 14 U/L,alkaline phosphatase 314 U/L,total bilirubin 2.4 mg/dL(direct bilirubin 2.0),and albumin 3.6 g/dL.The hepatitis panel was negative.The international normalized ratio(INR) was 1.8,CA19-9 was slightly elevated 52 U/mL(normal limit up to 33 U/mL),and AFP and CEA were negative.
CT and MRI scans showed diffuse circumferential arterial enhancing gallbladder wall thickening with an indistinct border with the liver suggestive of gallbladder tumor.There was no intrahepatic biliary ductal dilatation and no abdominal lymphadenopathy.No gallstones were seen (Fig.1).
At laparotomy,the liver was not cirrhotic and the mass seemed to be infiltrating the duodenum and colon.No intra-abdominal collection or abscesses were seen.The common bile duct (CBD) was thickened and seemed to be infiltrated.Although the frozen section biopsies of the colon,duodenum,and cystic duct stump were negative for malignancy,the clinical history,CA19-9,imaging,and intraoperative findings were suggestive of malignancy,which led us to resect the mass.The CBD was divided at the level of the pancreas and the patient underwent left liver trisegmentectomy,periportal lymphadenectomy,and Roux-en-Y hepaticojejunostomy.We used intra-operative ultrasound to guide the resection,and the estimated remnant volume was 55%of the whole liver volume.Pathological examination of the surgical specimen (Fig.2) unexpectedly revealed XGC without malignancy (Fig.3).The post-operative course was uneventful and the patient was discharged home after 8 days.Six months after the operation the patient is asymptomatic.
Discussion
Our patient exhibited severe,destructive,tumor-like xanthogranulomatous in flammation,with adherence to adjacent organs (colon and duodenum),and in flammatory stenosis of the CBD.Because the patient had no increased white blood cell count and no history of gallstones,the CA19-9 was slightly elevated,and the CT scan and intra-operative findings were suggestive of malignancy,the most probable diagnosis was a locally advanced gallbladder cancer,despite his young age.Despite the fact that the intra-operative frozen-section biopsies were negative for malignancy,we performed an extensive hepatectomy and reconstruction of the biliary system because the diagnosis was unclear,the CBD was narrowed,and the patient had a low operative risk.
XGC is not frequently associated with obstructive cholestasis.Krishna et al[10]reported only 4 cases of in flammatory strictures of the extrahepatic biliary tract in a total of 620 cases of XGC.These patients were managed with resection of the CBD,pancreatoduodenectomy or hepatectomy.Kawana and colleagues[11]reported a case in which a child with XGC-associated stenosis of the CBD was treated by a cholecystectomy,resection of the choledochus,and hepaticojejunostomy.Cholestasis is usually associated with stenosis of the CBD caused by in flammatory extension from XGC[10-12]and can lead to Mirizzi syndrome.[13]
The differential diagnosis of XGC and gallbladder adenocarcinoma/cholangiocarcinoma is very difficult.[14]The clinical presentation can be similar,and in patients with XGC the CA19-9 can be normal or elevated.[14]Adachi et al[15]reported that serum CA19-9 is not reliable to differentiate XGC from adenocarcinoma because in both conditions this marker can be elevated.It is also difficult to differentiate these conditions with ultrasound,CT,and MRI imaging.[16]Even PET-CT,which has been shown to be useful in differentiating between benign and malignant lesions,can lead to falsepositive results in the presence of XGC.[5]
The role of frozen sections is also important and they should always be performed.However,in cases showing extensive invasion of extra-gallbladder organs,the surgical strategy should not be determined only by frozen section examination since it can give falsenegative results.[4,7,17]
In conclusion,advanced and pseudotumoral XGC constitutes a surgical dilemma.Preoperative and intraoperative differential diagnosis of XGC from gallbladder carcinoma remains a challenge when it is associated with in flammatory involvement of surrounding tissues.Since gallbladder carcinoma and XGC may coexist,[18-20]radical resection is justified when malignancy cannot be completely ruled out.Radical resection for a benign process and the associated morbidity should be balanced against leaving the patient with persistent biliary stricture or leaving behind an undiagnosed tumor.In this circumstance,a second operative approach in a liver hilum that has been previously manipulated is more difficult and associated with complications and a higher risk of tumor spread.
Contributors:MPN proposed the study,participated in the operation and care of the patient,and wrote the first draft.SP and FM participated in the care of the patient and reviewed the manuscript.MPN is the guarantor.
Funding:None.
Ethical approval:Not needed.
Competing interest:No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
1 Yang T,Zhang BH,Zhang J,Zhang YJ,Jiang XQ,Wu MC.Surgical treatment of xanthogranulomatous cholecystitis:experience in 33 cases.Hepatobiliary Pancreat Dis Int 2007;6:504-508.
2 Benbow EW.Xanthogranulomatous cholecystitis.Br J Surg 1990;77:255-256.
3 Sharma D,Babu R,Sood G,Kapoor G,Solanki RS,Thomas S.Xanthogranulomatous cholecystitis masquerading as malignancy with liver metastasis.ANZ J Surg 2009;79:946-947.
4 Spinelli A,Schumacher G,Pascher A,Lopez-Hanninen E,Al-Abadi H,Benckert C,et al.Extended surgical resection for xanthogranulomatous cholecystitis mimicking advanced gallbladder carcinoma:A case report and review of literature.World J Gastroenterol 2006;12:2293-2396.
5 Makino I,Yamaguchi T,Sato N,Yasui T,Kita I.Xanthogranulomatous cholecystitis mimicking gallbladder carcinoma with a false-positive result on fluorodeoxyglucose PET.World J Gastroenterol 2009;15:3691-3693.
6 Enomoto T,Todoroki T,Koike N,Kawamoto T,Matsumoto H.Xanthogranulomatous cholecystitis mimicking stage IV gallbladder cancer.Hepatogastroenterology 2003;50:1255-1258.
7 Rastogi A,Singh DK,Sakhuja P,Gondal R.Florid xanthogranulomatous cholecystitis masquerading as invasive gallbladder cancer leading to extensive surgical resection.Indian J Pathol Microbiol 2010;53:144-147.
8 Pinocy J,Lange A,König C,Kaiserling E,Becker HD,Kröber SM.Xanthogranulomatous cholecystitis resembling carcinoma with extensive tumorous infiltration of the liver and colon.Langenbecks Arch Surg 2003;388:48-51.
9 Maeda T,Shimada M,Matsumata T,Adachi E,Taketomi A,Tashiro Y,et al.Xanthogranulomatous cholecystitis masquerading as gallbladder carcinoma.Am J Gastroenterol 1994;89:628-630.
10 Krishna RP,Kumar A,Singh RK,Sikora S,Saxena R,Kapoor VK.Xanthogranulomatous in flammatory strictures of extrahepatic biliary tract:presentation and surgical management.J Gastrointest Surg 2008;12:836-841.
11 Kawana T,Suita S,Arima T,Hirayama Y,Ishii K,Minamishima I,et al.Xanthogranulomatous cholecystitis in an infant with obstructive jaundice.Eur J Pediatr 1990;149:765-767.
12 Kawate S,Ohwada S,Ikota H,Hamada K,Kashiwabara K,Morishita Y.Xanthogranulomatous cholangitis causing obstructive jaundice:a case report.World J Gastroenterol 2006;12:4428-4430.
13 Lee KC,Yamazaki O,Horii K,Hamba H,Higaki I,Hirata S,et al.Mirizzi syndrome caused by xanthogranulomatous cholecystitis:report of a case.Surg Today 1997;27:757-761.
14 Yoshida J,Chijiiwa K,Shimura H,Yamaguchi K,Kinukawa N,Honda H,et al.Xanthogranulomatous cholecystitis versus gallbladder cancer:clinical differentiating factors.Am Surg 1997;63:367-371.
15 Adachi Y,Iso Y,Moriyama M,Kasai T,Hashimoto H.Increased serum CA19-9 in patients with xanthogranulomatous cholecystitis.Hepatogastroenterology 1998;45:77-80.
16 Chun KA,Ha HK,Yu ES,Shinn KS,Kim KW,Lee DH,et al.Xanthogranulomatous cholecystitis:CT features with emphasis on differentiation from gallbladder carcinoma.Radiology 1997;203:93-97.
17 Aoki T,Tsuchida A,Kasuya K,Inoue K,Saito H,Koyanagi Y.Is frozen section effective for diagnosis of unsuspected gallbladder cancer during laparoscopic cholecystectomy?Surg Endosc 2002;16:197-200.
18 Kwon AH,Sakaida N.Simultaneous presence of xanthogranulomatous cholecystitis and gallbladder cancer.J Gastroenterol 2007;42:703-704.
19 Lopez JI,Elizalde JM,Calvo MA.Xanthogranulomatous cholecystitis associated with gallbladder adenocarcinoma.A clinicopathological study of 5 cases.Tumori 1991;77:358-360.
20 Benbow EW.Xanthogranulomatous cholecystitis associated with carcinoma of the gallbladder.Postgrad Med J 1989;65:528-531.
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- Disease spectrum and use of cholecystolithotomy in gallstone ileus
- Liver transplantation in Crigler-Najjar syndrome type I disease
- High-intensity focused ultrasound ablation as a bridging therapy for hepatocellular carcinoma patients awaiting liver transplantation
- Laparoscopic distal pancreatectomy with or without splenectomy:spleen-preservation does not increase morbidity
- Expression of HBx protein in hepatitis B virusinfected intrahepatic cholangiocarcinoma
- Effect of endogenous hypergastrinemia on gallbladder volume and ejection fraction in patients with autoimmune gastritis