Effect of endogenous hypergastrinemia on gallbladder volume and ejection fraction in patients with autoimmune gastritis
2012-06-11
Ankara,Turkey
Introduction
Autoimmune gastritis (AIG) is an organ-specific in flammatory autoimmune disease characterized by antibodies to gastric parietal cells.In the early stages of the disease,AIG is usually clinically silent and demonstrable only by specific serologic tests such as antibodies to gastric parietal cells or intrinsic factor,[1]and there is no specific symptom associated with this condition,thus diagnosis is limited to clinical suspicion.The clinical manifestations of AIG are extremely heterogeneous and they include symptoms such as epigastric and abdominal pain,abdominal bloating,and diarrhea.[2]AIG is also accompanied by raised serum levels of gastrin caused by hypochlorhydria or achlorhydria.The regulation of gallbladder motor activity depends on neural and hormonal factors.It is well known that cholecystokinin is an important gastrointestinal hormone that coordinates gallbladder motility.It mainly affects gallbladder motility in the postprandial phase through CCK-1 receptors.The gallbladder ejection fraction (GEF) is positively correlated with the CCK receptor density on gallbladder smooth muscle.[3]The molecular structure of gastrin is very close to CCK,and gastrin also stimulates gallbladder smooth muscle contraction.Gastrin has a cholecystokinetic action on gallbladder motility,and cholecystokinin and gastrin act directly on the smooth muscle of the gallbladder.[3-5]The motor activity of the gallbladder can be evaluated by ultrasonography.Gallbladder dysmotility is a relatively rare condition.Its main clinical presentation,right upper quadrant and epigastric pain,is not easily differentiated from other functional gastrointestinal disorders.Although most patients with gallbladder motility disorders present with right upper quadrant pain,some may have poorly-defined chronic abdominal pain,flatulence and abdominal bloating suggestive of other functional gastrointestinal disorders such as functional dyspepsia,gastroesophageal re flux disease and irritable bowel syndrome.[6]Our hypothesis was that,since AIG is an autoimmune disease characterized by hypergastrinemia and gastrin has a cholecystokinetic effect on gallbladder motility,chronic endogenous hypergastrinemia might play a role in the development of altered gallbladder motility.The aim of the present study was to assess whether chronic endogenous hypergastrinemia has any effect on the gallbladder volume and ejection fraction in a group of patients with AIG; moreover,the effect of chronic endogenous hypergastrinemia on gallbladder motility has not been investigated.
Methods
Patients
A total of 41 patients with AIG and 29 healthy individuals were enrolled in the study.The diagnosis of chronic AIG was based on the histopathological findings in gastric biopsy tissue and histopathological diagnosis was available for each patient.In addition,the presence of anti-parietal cell antibody,gastric juice pH,and serum gastrin levels were also determined in each patient as described by Vargas et al.[7]The healthy subjects were recruited from the check-up center of the hospital who agreed to enter the study.The demographic data of each patient including age,gender,smoking,and body mass index (BMI) were recorded.All patients were questioned for the presence of other concomitant autoimmune diseases.Exclusion criteria were as follows:patients with gallstone disease,cholecystectomy,diabetes mellitus,thyroid diseases,gastric surgery,anti-cholinergics,and other systemic and neurological diseases,and drugs that might affect gallbladder motility (e.g.anti-cholinergics).This study was approved by the Institutional Review Board of Ankara University Faculty of Medicine and all subjects signed informed consent before entering the study.
Laboratory examinations
Serum gastrin (Biosource Europe SA,Nivelles,Belgium,with radio-immunoassay according to the instructions of the supplier),serum vitamin B12 level,anti-parietal cell antibody (APA) (Euroimmun,Lübeck,Germany,with indirect immuno fluorescence test according to the instructions of the supplier) and gastric juice pH were also investigated in each patient.Helicobacter pylori status was determined by both histopathological evaluation and serologic testing [serum H.pylori IgG was measured by enzyme-linked immunoabsorbant assay (ELISA,Trinity Biotech,Jamestown,NY,USA)].
Fasting gallbladder volume (FGV),postprandial gallbladder volume (PPGV),and GEF
Gallbladder measurements were performed using an ultrasound machine with a 3.5 MHz convex probe(General Electric,Pro Series,Healthcare,Korea).The ultrasonographer was not aware of the diagnosis of the patients.Smoking,alcohol consumption,and the use of caffeine were prohibited 24 hours before ultrasonographic examination in order to avoid possible effects on gallbladder motility.The mean gallbladder volume was calculated using the ellipsoid method described by Dodds et al.[8]In brief,one longitudinal(D1) and two cross-sectional diameters (D2 and D3) and the volume were calculated using the ellipse formula(π/6×D1×D2×D3).The mean gallbladder volume was calculated from the measurements of three sequential gallbladder volumes.[9]Premenopausal women were examined in the first phase of the menstrual cycle,in order to avoid gallbladder motility changes during the cycle.[10]All patients and healthy subjects were investigated after 12 hours of fasting and 30 minutes after a meal consisting of 100 g milky chocolate of the same brand (54.1% carbohydrate,31.5% lipid,and 9.2%protein).[9]FGV and PPGV were substituted into the following formula in order to calculate the GEF:GEF(%)=(FGV-PPGV)/(FGV)×100.[11,12]
Statistical analysis
Statistical analysis was done with SPSS 16.0 for Windows (SPSS Inc,Chicago,IL).All values were expressed as mean±standard deviation (SD) unless otherwise stated.A two-tailed t test was used to compare quantitative variables.The Mann-Whitney U test and Fisher's exact test were used for statistical comparisons whenever appropriate.The risk factors were detected by logistic regression analysis.A P value <0.05 was considered statistically significant.
Results
In this comparative study,41 patients with AIG [29females (70.7%),12 males,mean age 46.00±12.53 years (range 24-78)] were enrolled.These results were compared with 29 control subjects [17 females (58.6%),12 males,mean age 44.82±10.66 years (range 34-87)].The levels of serum gastrin (P<0.001) and vitamin B12 level (P=0.012) were significantly higher in the AIG patients than in the control subjects (Table).Among the 41 AIG patients,35 (85.3%) were APA-positive and 6 (14.7%) APA-negative.Patients with AIG were stratified into three groups according to the main reason for investigation:abdominal/epigastric pain (n=9),abdominal bloating (n=14) and iron and/or vitamin B12 deficiency (n=13).There was no difference between the AIG patients and the control subjects in terms of mean FGV (30.38±12.85 vs 29.27±9.91 cm3,P=0.189) and mean PPGV (15.67±8.32 vs 13.44±7.69 cm3,P=0.258)(Fig.1).The GEF (%) of the AIG patients was lower than that of the control subjects (46.06±18.28% vs 55.03±14.67%,P=0.032) (Fig.2).As for the symptom groups,logistic regression analysis of baseline parameters revealed that "abdominal bloating" was a risk factor for low GEF (%) in AIG patients (P=0.045,F=4.40).In addition,logistic regression analysis of baseline parameters revealed that smoking (n=5,P=0.025,F=5.44) was a predictor of low GEF (%) for AIG patients.It was found that age,gender,APA positivity,H.pylori,BMI,gastrin,B12,iron,ferritin,folate,homocysteine,mean corpuscular volume,total cholesterol,high density lipoprotein,low density lipoprotein,very low density lipoprotein and triglyceride were not significant risk factors for low GEF (%).
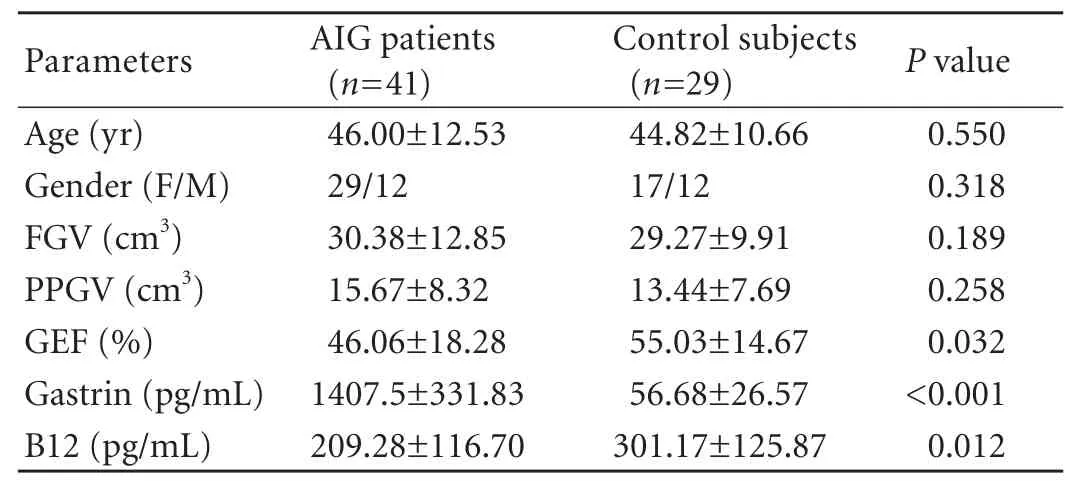
Table.Comparison of FGV,PPGV,and EF (%) of AIG patients and controls
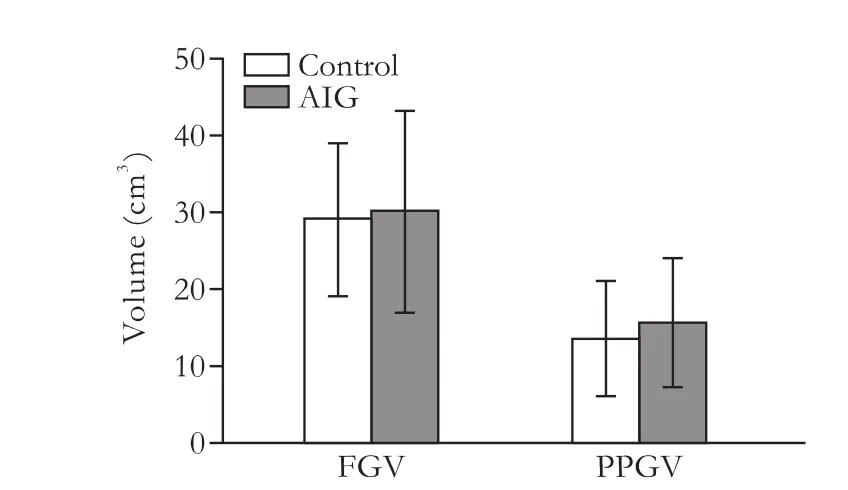
Fig.1.FGV and PPGV of patients with AIG compared with the control subjects.FGV:fasting gallbladder volume; PPGV:postprandial gallbladder volume.

Fig.2.Gallbladder ejection fraction of patients with autoimmune gastritis (AIG) compared with the control group.
Discussion
The results of this study showed that GEF was significantly lower in patients with AIG than in healthy controls,suggesting gallbladder dysmotility.There are no other studies addressing gallbladder problems in AIG.It is possible to evaluate gallbladder motility by using different imaging techniques.Although ultrasonography is operator-dependent,it is a readily available technique in daily practice.Ultrasonographic evaluation of gallbladder motility is an acceptable technique without radiation exposure and with its low cost in the work-up of patients in which gallbladder dysmotility is suspected.For these reasons,we preferred to use ultrasonography in the evaluation of gallbladder motility.[13]Lock et al[14]compared gallbladder motility in 20 patients with systemic sclerosis and healthy subjects.They found that motility in patients with sclerosis was not reduced when compared with controls and concluded that measurement of gallbladder emptying is not a helpful tool when looking for gastrointestinal involvement in systemic sclerosis.In a similar study,Posthuma et al[15]compared gallbladder motility in 10 patients with systemic sclerosis with 10 healthy subjects by ultrasonography.They found that motility in patients with sclerosis was preserved and suggested that such patients are not at increased risk for cholelithiasis because of gallbladder dysmotility.In a more detailed study,Di Ciaula et al[16]investigated 38 systemic scleroderma patients,60 healthy controls and 68 dyspeptic controls in terms of gastric and gallbladder motility.They found no difference between sclerosis patients versus dyspeptic and healthy controls for fasting volume and postprandial indices of gallbladder emptying.Kapicioglu et al[17]investigated the effect of omeprazole on gallbladder contraction in 20 healthy subjects using intravenous omeprazole and found no difference between subjects receiving omeprazole and placebo.Their hypothesis was that omeprazole causes hypergastrinemia because of the effects of prolonged suppression of acid secretion and the excitatory effects of omeprazole on gallbladder contraction.However,they did not report the gastrin levels achieved after omeprazole infusion.Zhang et al[18]investigated the levels of various gastrointestinal hormones in the plasma and gallbladder tissues of patients with gallbladder stones,gallbladder polyps and healthy subjects.They found that the level of plasma gastrin in patients with gallbladder stones was elevated compared to that in healthy subjects,and concluded that disturbance of gastrointestinal hormones may cause motor dysfunction of the gallbladder and bile stasis.In another study,Alagozlu et al[19]examined gallbladder motility in patients with achalasia and found that these patients had small gallbladders and lower GEF compared with healthy subjects.They speculated that this is congenital and/or the gallbladders of patients with achalasia have incomplete relaxation.There is no evidence that AIG is a congenital disorder.The autonomic nervous system and cholecystokinin play important roles in normal gallbladder function.Abnormalities have been found in autonomic nervous system function and cholecystokinin release in patients with irritable bowel syndrome.[20]In patients with irritable bowel syndrome,which is a common functional gastrointestinal disorder involving smooth muscle function in different systems of the body,Guliter et al[9]found no difference between irritable bowel syndrome patients and healthy subjects by means of FGVs.In contrast,the GEF of irritable bowel syndrome patients was found to be higher than that in the control group.However,we do not regard our findings as secondary to vagal nerve dysfunction,although we did not assess vagal nerve parameters in the current study.We found that the GEF was lower than in the healthy subjects.As for symptom groups,logistic regression analysis of baseline parameters revealed that"abdominal bloating" was a risk factor for low GEF (%)in AIG patients.We know that there are no specific clinical manifestations or symptoms that indicate AIG.Disturbances of gallbladder motility may be a cause of dyspeptic symptoms in patients with AIG.
In conclusion,we have demonstrated that AIG patients have a lower GEF than healthy subjects.Altered gallbladder motility may help to explain some of the upper gastrointestinal symptoms in patients with AIG,and that may be clinically helpful in managing patients with such symptoms.Therefore,further prospective,multicenter,well-designed studies which compare the symptoms of patients who have or have not had a cholecystectomy are needed to understand underlying mechanism(s) leading to gallbladder dysfunction,and alternatively,data on the histological evaluation of resected gallbladders from AIG patients may shed light on the pathophysiology of biliary disease in patients with AIG.
Contributors:SI proposed the study.YM and KO performed research and wrote the first draft.YM collected and analyzed the data.All authors contributed to the design and interpretation of the study and to further drafts.SI is the guarantor.
Funding:None.
Ethical approval:This study was approved by the Institutional Review Board of Ankara University,Faculty of Medicine.
Competing interest:No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
1 Toh BH,Chan J,Kyaw T,Alderuccio F.Cutting Edge Issues in Autoimmune Gastritis.Clin Rev Allergy Immunol 2010 Dec 22.
2 Kabacam G,Bektas M,Ustun Y,Yakut M,Toruner M,Cetinkaya H,et al.Clinical and laboratory features of patients with significantly elevated serum gastrin level.Gastroenterology 2009;136:A485.
3 Portincasa P,Di Ciaula A,Wang HH,Palasciano G,van Erpecum KJ,Moschetta A,et al.Coordinate regulation of gallbladder motor function in the gut-liver axis.Hepatology 2008;47:2112-2126.
4 Hildebrand P,Werth B,Beglinger C,Delco F,Jansen JB,Lamers CB,et al.Human gastrin-releasing peptide:biological potency in humans.Regul Pept 1991;36:423-433.
5 Cox MR,Padbury RT,Snelling TL,Schloithe AC,Harvey JR,Toouli J,et al.Gastrin-releasing peptide stimulates gallbladder motility but not sphincter of Oddi motility in Australian brush-tailed possum.Dig Dis Sci 1998;43:1275-1284.
6 Behar J,Corazziari E,Guelrudg M,Hogan W,Sherman S,Toouli J.Functional gallbladder and sphincter of Oddi disorders.In:Drossman DA ed.The functional gastrointestinal disorders,3rd ed.McLean,VA,USA:Degnon Associates,Inc.;2006:595-638.
7 Vargas JA,Alvarez-Mon M,Manzano L,Albillos A,Fernandez-Corugedo A,Albarrán F,et al.Functional defect of T cells in autoimmune gastritis.Gut 1995;36:171-175.
8 Dodds WJ,Groh WJ,Darweesh RM,Lawson TL,Kishk SM,Kern MK.Sonographic measurement of gallbladder volume.AJR Am J Roentgenol 1985;145:1009-1011.
9 Guliter S,Yilmaz S,Yakaryilmaz F,Keles H.Evaluation of gallbladder motility in patients with irritable bowel syndrome.Swiss Med Wkly 2005;135:407-411.
10 Nilsson S,Stattin S.Gallbladder emptying during the normal menstrual cycle.A cholecystographic study.Acta Chir Scand 1967;133:648-652.
11 Montet JC,Caroli-Bosc FX,Ferrari P,Piche T,Baize N,Anty R,et al.Gallbladder motility and gut hormone plasma levels in subjects with and without gallstones.Gastroenterol Clin Biol 2005;29:569-572.
12 Festi D,Frabboni R,Bazzoli F,Sangermano A,Ronchi M,Rossi L,et al.Gallbladder motility in cholesterol gallstone disease.Effect of ursodeoxycholic acid administration and gallstone dissolution.Gastroenterology 1990;99:1779-1785.
13 Portincasa P,Moschetta A,Colecchia A,Festi D,Palasciano G.Measurements of gallbladder motor function by ultrasonography:towards standardization.Dig Liver Dis 2003;35:S56-61.
14 Lock G,Zeuner M,Kammerl M,Lang B,Schölmerich J,Holstege A.Gallbladder motility in systemic sclerosis.Rheumatol Int 1996;16:61-65.
15 Posthuma WF,Ledeboer M,Masclee AA,Dijkmans BA,Westendorp RG,Jebbink MC,et al.Do patients with systemic sclerosis have abnormal gallbladder function? Eur J Gastroenterol Hepatol 1997;9:675-677.
16 Di Ciaula A,Covelli M,Berardino M,Wang DQ,Lapadula G,Palasciano G,et al.Gastrointestinal symptoms and motility disorders in patients with systemic scleroderma.BMC Gastroenterol 2008;8:7.
17 Kapicioglu S,Baki AH,Arslan M,Cetiner M,Cihanyurdu N.Effect of omeprazole on gallbladder contraction in humans.Hepatogastroenterology 2000;47:346-348.
18 Zhang ZH,Wu SD,Su Y,Jin JZ,Fan Y,Yu H,et al.Differences and significance of motilin,vasoactive intestinal peptide and gastrin in blood and gallbladder tissues of patients withgallstones.Hepatobiliary Pancreat Dis Int 2008;7:58-64.
19 Alagozlu H,Unal S,Karakan T,Cindoruk M,Ergun M.Small-volume gallbladders and decreased motility in patients with achalasia.J Clin Gastroenterol 2008;42:191-193.
20 Sood GK,Baijal SS,Lahoti D,Broor SL.Abnormal gallbladder function in patients with irritable bowel syndrome.Am J Gastroenterol 1993;88:1387-1390.
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- Disease spectrum and use of cholecystolithotomy in gallstone ileus
- Xanthogranulomatous cholecystitis mimicking gallbladder cancer and causing obstructive cholestasis
- Liver transplantation in Crigler-Najjar syndrome type I disease
- High-intensity focused ultrasound ablation as a bridging therapy for hepatocellular carcinoma patients awaiting liver transplantation
- Laparoscopic distal pancreatectomy with or without splenectomy:spleen-preservation does not increase morbidity
- Expression of HBx protein in hepatitis B virusinfected intrahepatic cholangiocarcinoma