Surgical treatment of Budd-Chiari syndrome: analysis of 221 cases
2011-07-05XiaoWeiDangPeiQinXuXiuXianMaDaQianXuYanJuZhuandYongShuaiZhang
Xiao-Wei Dang, Pei-Qin Xu, Xiu-Xian Ma, Da-Qian Xu, Yan-Ju Zhu and Yong-Shuai Zhang
Zhengzhou, China
Clinical Summary
Surgical treatment of Budd-Chiari syndrome: analysis of 221 cases
Xiao-Wei Dang, Pei-Qin Xu, Xiu-Xian Ma, Da-Qian Xu, Yan-Ju Zhu and Yong-Shuai Zhang
Zhengzhou, China
BACKGROUND:Budd-Chiari syndrome (B-CS) refers to post-hepatic portal hypertension and/or inferior vena cava hypertension caused by obstruction of blood flow at the portal cardinal hepatic vein. The treatments of B-CS include operations on pathological membrane lesions, shunting and combined operations. Studies have shown that China, Japan, India and South Africa have a high incidence of B-CS. In China, the Yellow River Basin in Henan, Shandong, Jiangsu and Anhui Provinces also have a high incidence, around 10 per 100 000.
METHODS:The clinical data of 221 B-CS patients were analyzed retrospectively. We focused on pathological types, surgical methods, effectiveness and complications of treatment, and follow-up.
RESULTS:Based on imaging findings such as color ultrasonography, angiography or magnetic resonance angiography, the 221 patients were divided into 3 types (five subtypes): type Ia (72 patients), type Ib (20), type II (72), type IIIa (33), and type IIIb (24). Surgical procedures included balloon membranotomy with or without stent (65 patients), improved splenopneumopexy (18), radical resection of membrane and thrombus (17), inferior vena cava bypass [29, with cavocaval transflow (13) and cavoatrial transflow (16)], mesocaval shunt (41), splenocaval shunt (25), splenoatrial shunt (12), splenojugular shunt (6), and combined methods (8). The complication rate was 9.05% (20/221) and the perioperative death rate was 2.26% (5/221). All of the patients were followed up from 6 months to 5 years. The success rate was 84.6% (187/221), and the recurrence rate was 8.9% (9/101) and 13.5% (13/96) after 1- and 5-year follow-up, respectively.
CONCLUSION:The rational choice of surgical treatment based on B-CS pathological typing may increase the success rate and decrease the recurrence.
(Hepatobiliary Pancreat Dis Int 2011; 10: 435-438)
Budd-Chiari syndrome; intervention; shunt; transflow
Introduction
Budd-Chiari syndrome (B-CS) is a severe benign disease with a complex presentation. The main clinical manifestations are symptoms of posthepatic portal hypertension and/or inferior vena cava hypertension, such as hepatomegaly, intractable ascites, upper gastrointestinal bleeding, splenomegaly, hypersplenism, varicose veins of the abdominal wall, and edema and/or pigmentation of the lower extremities.[1,2]The etiology of B-CS is still unclear,[1,3]and it is thought to be due to membrane formation and thrombosis.[3,4]Determination of lesion type in B-CS is important for the selection of treatment. The choice of treatment for such patients is often difficult, even for an experienced surgeon.[2]We treated 221 B-CS patients from January 2003 to June 2009 and report here their clinical outcomes.
Clinical summary
In the 221 B-CS patients, 124 were men and 97 women, with age ranging from 18 to 68 years, average 35.6±7.6. When symptoms appeared, the shortest duration was 2 months and the longest was 15 years. The patients were classified according to the report:[1]72 patients were of type Ia, 20 type Ib, 72 type II, 33 type IIIa, and 24 type IIIb. The patients in the type IIIb group presented with mainly symptoms and signs of portal hypertension and/or hypertension of the inferior vena cava (IVC). Of the 221 patients, 212 had hypodynamia symptoms, 201 had abdominal distension, 197 had anorexia, 77 had abdominal pain, 50 had jaundice, 177 had liver enlargement, 97 had splenomegaly, 146 had chest or abdominal wall varices, 96 had ascites, 126 had leg edema or pigmentation, 86 had upper gastrointestinal hemorrhage (hematemesis or melena), and 15 hadcritical conditions. In 96 patients preoperative or surgical liver biopsy showed sinusoidal expansion and shrinkage of liver cells near the center of the lobular liver cell necrosis and fibrosis. Examinations for diagnosis prior to treatment included color Doppler ultrasound (221 patients), angiography (112), and magnetic resonance angiography or 64-slice CT angiography (145).
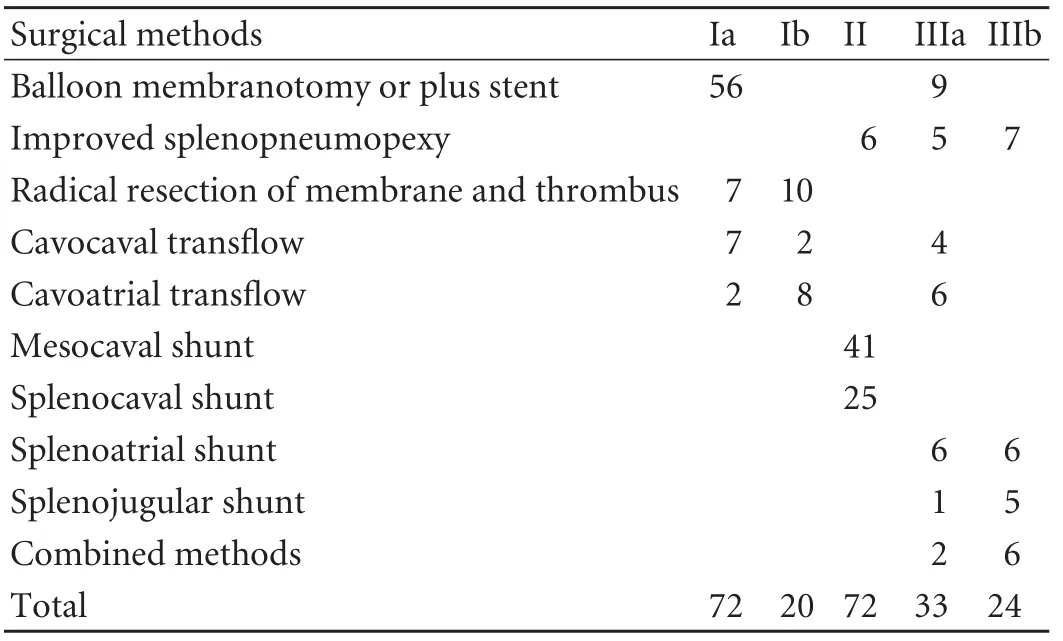
Table 1. Treatment methods of 221 B-CS patients
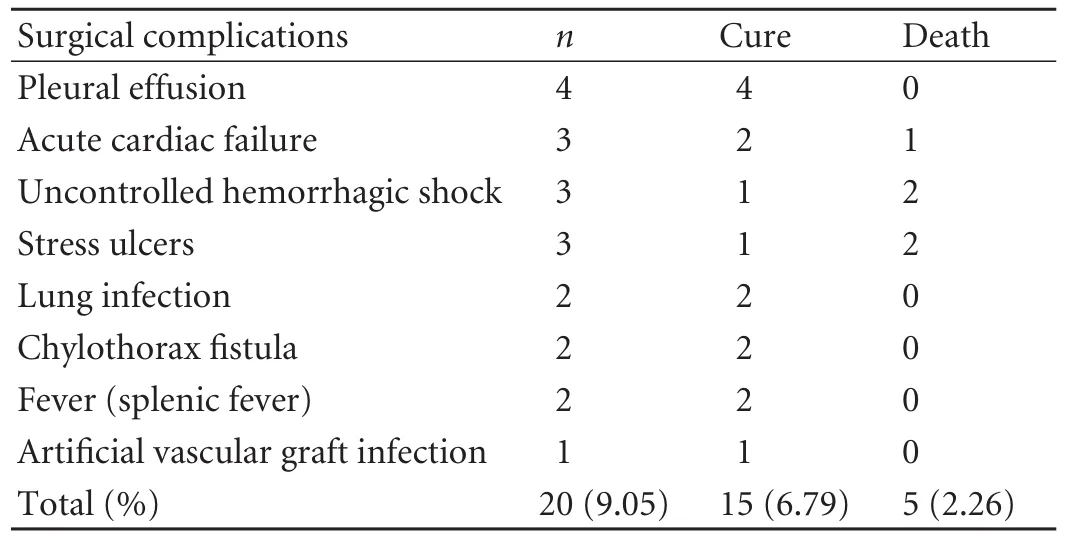
Table 2. Complications and treatment results of B-CS patients (n=20)
The methods of treatment are shown in Table 1. The patients in the combined methods group underwent both balloon membranotomy and mesocaval shunt simultaneously. The details and treatment results are shown in Table 2. The surgical complication rate was 9.05% (20/221), and the operative mortality rate was 2.26% (5/221). Postoperative follow-up of the 221 patients ranged from 6 months to 5 years and showed an overall success rate of 84.6% (187/221). The recurrence rates after 1 and 5 years after the operation were 8.9% (9/101) and 13.5% (13/96), respectively. The efficacy standard was based on a report.[1]
Discussion
Early definitions of B-CS narrowly refer to Chiari disease, namely, main hepatic vein (MHV) obstruction with thrombosis. In Asia, South Africa and other countries, the effect of membrane obstruction of the IVC is similar to that of Chiari disease, so generalized B-CS refers to post-hepatic portal vein hypertension and/or IVC hypertension syndrome caused by the obstruction of blood flow at the portal cardinal hepatic vein and/or the IVC.[1,4]By the end of 2008, more than 5000 cases were reported in China, suggesting that the disease has become a threat to public health. The highrisk countries include China, Japan, India, and South Africa. In China, the risk is high in areas of the Yellow River basin including Henan, Shandong, Jiangsu, and Anhui Provinces.[1]Blood clotting disorders, pregnancy, infection, oral contraceptives, trauma and tumors can cause B-CS.[1]
Clinical pathological type
The condition of B-CS is complicated and the clinical pathological types of the disease are various according to different standards. Investigators in China and overseas may use different classification methods for the disease. Xu et al[1,5]divided B-CS into type Ia: membranous obstruction of the IVC, and the MHV partly or unobstructed without thrombosis under the membrane; type Ib: membrane obstruction of the IVC, and the MHV partly or unobstructed with a mural thrombus under the membrane; type II: a segmental stenosis of the IVC, and an occlusion of the MHV; type IIIa: a short segmental occlusion of the IVC (<2 cm), and an obstruction of the MHV or at least one MHV was unobstructed or the hepatic right rear vein compensatorily expanded and unobstructed; type IIIb: a long segmental occlusion of the IVC (≥2 cm), and an obstruction of the MHV but without compensatory expansion of the vein in the third lobe of the liver. Xu et al[5]also put forward the concept and diagnostic criteria of severe B-CS. Any type of B-CS whether acute or chronic which has one of the following conditions on clinical or radiographic examination can be considered as severe B-CS: 1) recalcitrant ascites and intra-abdominal pressure >20 mmHg; 2) oliguria (urine <400 mL/day) or anuria (urine <100 mL/day); 3) prothrombin time extended more than 50%, serum bilirubin >34.2 mmol/L, the ratio of A (albumin)/G (globulin) inversion; 4) present or past hepatic encephalopathy; and 5) gastrointestinal hemorrhage.[6]
Treatment method and selection
There are dozens of surgical methods for B-CS, including those for diaphragm lesions (e.g. Kimura finger membranotomy, balloon membranotomy, radicalresection of membrane and thrombus), transflow (IVC bypass surgery), shunt (more specific methods), and combined surgery (intervention plus transflow or shunt plus shunt surgery). The main purposes of these methods are to remove the obstruction, restore the blood flow of the hepatic vein and/or IVC, relieve portal vein pressure, remit the congested state of the MHV and IVC, control or prevent upper gastrointestinal hemorrhage, alleviate the spleen, eliminate ascites, and protect hepatocytes.
Transjugular intrahepatic portosystemic shunt (TIPS) has also been performed to treat B-CS. The basic pathological change is obstruction of the outflow tract. TIPS flow is from the MHV or the retrohepatic segment of the IVC, hence if the MHV is obstructed, how can TIPS be accomplished? If puncture at the equivalent of the MHV outflow is chosen, because the "MHV" has been opened, how is the shunt "intrahepatic portosystemic"? Strictly speaking, "TIPS" surgery for B-CS should be called transjugular hepatic venoplasty/ veno-reconstruction shunt. Therefore the application of TIPS for B-CS is still questionable.[1,7,8]
Typei(IVC type)
The main pathological change of typeiis the appearance of a diaphragm lesion in the IVC. Based on whether there is thrombosis under the diaphragm, this type can be divided into Ia and Ib and its earliest treatment is finger membranotomy through the right atrium. This treatment has been replaced by minimally invasive techniques due to the development and maturation of intervention technology in recent years. Therefore the preferred treatment of type Ia is balloon membranotomy. The radical resection or transflow technique can be chosen if the patient has large and/or tough oblique and thick lesions. Successful intervention may complicate pulmonary embolism after expansion of the IVC balloon because type Ib has thrombus under the membrane.[9-11]For this reason we prefer to radical resection of the membrane and thrombus or shunt. We have studied this method by comparison of several treatments for 480 patients with membranous B-CS. We found in this study that the success rate of the treatment in the finger membranotomy group, the intervention group and the radical group was 61.4%, 91.7% and 90.4%, respectively, and the recurrence rate was 38.4%, 8.3% and 9.6%. Thus the long-term effects in the intervention group and the radical group were better than in the finger membranotomy group, and the recurrence rates were lower than in the finger membranotomy group. Therefore we think that even if B-CS patients can undergo the membrane-breaking surgery, balloon membranotomy should be chosen. Both radical resection and transflow can be chosen if the patient has large thrombosis, pathological lesions or tough oblique thickness lesions or if the disease relapses after interventional surgery. This type of the disease was found in 92 of our patients [balloon membranotomy (56), radical resection of membrane (17) and IVC bypass (19)]. One patient died of acute cardiac failure during surgery, and the remaining patients were cured.
Type II (MHV type)
The main clinical presentations of type II consist of the symptoms and signs of portal hypertension. The principal treatment is to reduce portal vein pressure. In our patients we tried to expand the occluded MHV through interventional methods, but the effect was poor or the symptoms relapsed in a short-term. Therefore we adopted different methods to transfer part of or all of the portal vein blood to the systemic circulation. This can alleviate the symptoms of portal hypertension, reducing portal vein pressure and/or controlling upper gastrointestinal hemorrhage. Shunts suitable for type II patients includes mesocaval shunt (M-CS) and splenocaval shunt (S-CS).[1,12,13]In our patients, 66 were treated by these procedures. Two patients died after shunts because of uncontrolled hemorrhagic shock caused by abdominal bleeding. In the patients who had stomach-esophagus varicosities or a history of upper gastrointestinal bleeding we performed transflow surgery combined with S-CS. With this method we treated 86 patients with portal hypertension, in whom portal vein pressure decreased to 6.6±1.2 cmH2O postoperatively. Their liver function before and after surgery did not change significantly. Postoperative follow-up of 56 patients for 3 months to 6 years showed a total success rate of 89.3% (50/56) except for 3 cases of recurrence and 3 deaths. The patency rate of artificial vascular graft was 95.7% (44/46). Thirty-six patients who had a history of preoperative gastrointestinal bleeding were subjected to a fiber-optic endoscopic examination showing disappearance of stomachesophagus varicosities. This examination also showed that S-CS combined with M-CS had been successful in reducing portal vein pressure and controlling upper gastrointestinal bleeding, and S-CS can eliminate hypersplenism. For the long-term effect, splenic-lung fixation also functions as a shunt. A total of 126 patients were treated by this method with a total success rate of 68.3% (86 patients). We think that patients with or without refractable ascites and cardiopulmonary functional disorders can be treated by improved splenopneumopexy operation if they are in poor economic conditions.[14,15]
Type III (mixed type)
Type III lesion is complex because it involves both the MHV and IVC. According to the pathological changes of the IVC and the presence or absence of obstruction in the MHV and its compensation, type III can be divided into IIIa and IIIb. Patients with type IIIa can undergo balloon membranotomy plus stenting and transflow surgery. If there is a thrombus in the IVC, shunt can also be performed to reduce portal vein pressure. Transflow uses the artificial vasculature at the IVC above and below the pathological lesions or cavoatrial transflow through bypass to restore the IVC blood flow, including cavocaval transflow and cavoatrial transflow. The cavocaval transflow proposed by Xu et al[1]compared with the cavoatrial transflow has some merits such as a reduced length of artificial vasculature, a minimized chance of thrombosis, no occurrence of tamponade, and a lowered incidence of pericarditis. In 33 patients with type IIIa, 9 underwent balloon membranotomy (including stenting in 4), 10 underwent transflow surgery and 7 underwent shunt. The symptoms of these patients improved significantly after surgery and the results were satisfactory. Since the condition of type IIIb patients was more serious than type IIIa patients, perioperative management should be stressed. Hence we select from the possible procedure from splenojugular shunt, splenoatrial shunt or combined methods.[6,16,17]In this group, 8 type III patients were treated with balloon membranotomy plus mesocaval shunt. Intra-operatively, the pressure of the IVC and the portal vein dropped significantly with the recovery of normal conditions. All patients were followed up for nearly 4 years without recurrence of the disease.
In conclusion, B-CS treatment should be based on the different pathological types of the disease. The scope of surgery for the disease is important to reduce the mortality rate, reduce perioperative complications, improve the success rate, and decrease the recurrence rate.
Funding:None.
Ethical approval:Not needed.
Contributors:DXW and XPQ proposed the study. DXW wrote the first draft and analyzed the data. All authors contributed to the design and interpretation of the study and to further drafts. DXW is the guarantor.
Competing interest:No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
1 Xu PQ, Ma XX, Ye XX, Feng LS, Dang XW, Zhao YF, et al. Surgical treatment of 1360 cases of Budd-Chiari syndrome: 20-year experience. Hepatobiliary Pancreat Dis Int 2004;3: 391-394.
2 Orloff MJ, Daily PO, Orloff SL, Girard B, Orloff MS. A 27-year experience with surgical treatment of Budd-Chiari syndrome. Ann Surg 2000;232:340-352.
3 Okuda H, Yamagata H, Obata H, Iwata H, sasaki R, Imai F, et al. Epidemiological and clinical features of Budd-Chiari syndrome in Japan. J Hepatol 1995;22:1-9.
4 Okuda K. Obliterative hepatocavopathy-inferior vena cava thrombosis at its hepatic portion. Hepatobiliary Pancreat Dis Int 2002;1:499-509.
5 Xu PQ, Zhang SJ. The experience and taste of the surgical treatment of Budd-Chiari syndrome. Fu Bu Wai Ke 1996;9: 146-149.
6 Xu PQ, Dang XW. Diagnosis and management of severe Budd-Chiari syndrome. Hepatobiliary Pancreat Dis Int 2003; 2:525-528.
7 Molmenti EP, Segev DL, Arepally A, Hong J, Thuluvath PJ, Rai R, et al. The utility of TIPS in the management of Budd-Chiari syndrome. Ann Surg 2005;241:978-983.
8 Rossle M, Olschewski M, Siegerstetter V, Berger E, Kurz K, Grandt D. et al. The Budd-Chiari syndrome: outcome after treatment with the transjugular intrahepatic portosystemic shunt. Surgery 2004;135:394-403.
9 Xu PQ, Dang XW. Treatment of membranous Budd-Chiari syndrome: analysis of 480 cases. Hepatobiliary Pancreat Dis Int 2004;3:73-76.
10 Kew MC, Hodkinson HJ. Membranous obstruction of the inferior vena cava and its causal relation to hepatocellular carcinoma. Liver Int 2006;26:1-7.
11 Hirooka M, Kimura C. Membranous obstruction of the hepatic portion of the inferior vena cava. Surgical correction and etiological study. Arch Surg 1970;100:656-663.
12 Ilkgul O, Kilic M, Icoz G, Zeytunlu M, Demirpolat G, Akyildiz M, et al. Experience with mesocaval shunt with autologous jugular vein interposition in patients with Budd-Chiari syndrome. Hepatogastroenterology 2005;52:662-665.
13 Uskudar O, Akdogan M, Sasmaz N, Yilmaz S, Tola M, Sahin B. Etiology and portal vein thrombosis in Budd-Chiari syndrome. World J Gastroenterol 2008;14:2858-2862.
14 Dang XW, Ma XX, Xu PQ. Modified splenopneumopexy in the treatment of Budd-Chiari syndrome: a report of 126 cases. Zhongguo Pu Tong Wai Ke Za Zhi 2006;12:884-886.
15 Lee BB, Villavicencio L, Kim YW, Do YS, Koh KC, Lim HK, et al. Primary Budd-Chiari syndrome: outcome of endovascular management for suprahepatic venous obstruction. J Vasc Surg 2006;43:101-108.
16 Klein AS. Management of Budd-Chiari syndrome. Liver Transpl 2006;12:S23-28.
17 Slakey DP, Klein AS, Venbrux AC, Cameron JL. Budd-Chiari syndrome: current management options. Ann Surg 2001;233: 522-527.
Received April 10, 2010
Accepted after revision February 5, 2011
Author Affiliations: Division of Hepatobiliary and Pancreatic Surgery, First Affiliated Hospital, Zhengzhou University, Zhengzhou 450052, China (Dang XW, Xu PQ, Ma XX, Xu DQ, Zhu YJ and Zhang YS)
Xiao-Wei Dang, MD, Division of Hepatobiliary and Pancreatic Surgery, First Affiliated Hospital, Zhengzhou University, Zhengzhou 450052, China (Tel: 86-371-66862122; Email: dangxw1001@163.com)
© 2011, Hepatobiliary Pancreat Dis Int. All rights reserved.
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- Hepatitis C virus infection and biological falsepositive syphilis test: a single-center experience
- Hepatobiliary & Pancreatic Diseases International (HBPD INT)
- Success rate and complications of endoscopic extraction of common bile duct stones over 2 cm in diameter
- Donor liver natural killer cells alleviate liver allograft acute rejection in rats
- Enteral supplementation with glycyl-glutamine improves intestinal barrier function after liver transplantation in rats
- Noninvasive indocyanine green plasma disappearance rate predicts early complications, graft failure or death after liver transplantation