Health-related quality of life in living liver donors after transplantation
2011-07-05PeiXianChenandLuNanYan
Pei-Xian Chen and Lu-Nan Yan
Chengdu, China
Review Article
Health-related quality of life in living liver donors after transplantation
Pei-Xian Chen and Lu-Nan Yan
Chengdu, China
BACKGROUND:Living donor liver transplantation (LDLT) has recently emerged as an effective therapeutic alternative for patients with end-stage liver disease. In the meantime, the health-related quality of life (HRQoL) of the donors is becoming better appreciated. Here we aimed to review the current literature and summarize the effects of liver donation on the long-term HRQoL of living donors.
DATA SOURCES:A literature search of PubMed using "donors", "living donor liver transplantation", "health-related quality of life", and "donation" was performed, and all the information was collected.
RESULTS:The varied postoperative outcomes of liver donors are attributive to the different evaluation instruments used. On the whole, donors experienced good long-term physical and mental well-being with a few complaining of compromised quality of life due to mild symptoms or psychiatric problems. The psychosocial dimension has received increasing attention with the vocational, interpersonal and financial impact of liver donation on donors mostly studied.
CONCLUSIONS:Generally, donors have a good HRQoL after LDLT. Nevertheless, to achieve an ideal donor outcome, further work is necessary to minimize the negative effects as well as to incorporate recent progress in regenerative medicine.
(Hepatobiliary Pancreat Dis Int 2011; 10: 356-361)
living donor; liver transplantation; donation; health-related quality of life
Introduction
Due to the disequilibrium between organ shortage and the mounting demand, living donor liver transplantation (LDLT) has emerged as a lifesaving alternative for those with end-stage liver disease[1]and has been given the green light in many countries throughout the world. An estimated number of over 12 000 LDLTs have been performed worldwide.[2]While the major focus has been directed towards the health-related quality of life (HRQoL) of the recipients, concerns over that of the donors are increasingly being voiced. According to some studies, up to 67% of donors suffer postoperative complications[3-7]with an overall reported mortality of 0.2% and a median morbidity of 16%.[8]In Japan, 8.4% of those who had donated grafts by the end of 2006 developed donation-related complications.[9]After donation, some donors may have to confront potentially life-threatening morbidity or even death, some may struggle with psychiatric problems or chronic symptoms for a long time after operation, while others feel fine and are willing to donate again. A nine-center adult-to-adult LDLT cohort study (A2ALL) disclosed that 62% of donors did not experience complications while 2% had life-threatening complications and 0.8% had lethal ones.[10]To some extent, such outcome variance implies that LDLT plays a role in alteration of the HRQoL of living donors after partial hepatectomy. HRQoL is a multi-faceted construct reflecting the overall physical, psychiatric and psychosocial well-being of a person.[11-15]Thus we reviewed the current literature and summarized the effect of LDLT on the physical, mental and psychosocial health of donors in the long run.
HRQoL
Physical health
Considering the magnitude of LDLT surgery itself and the associated risks, some donors are likely to develop postoperative complications and persistent symptomslong after donation. Ran et al[16]reported that 14 out of 105 living donors had postoperative complications, with 11 undergoing invasive treatment or re-operation. Among these medical complications, biliary events appear to be pronounced. According to Adcock et al,[17]bile leak occurred in 3% of 202 donors surveyed. Moreover, a multicenter study[5]showed that 82 donors had biliary complications including cholestasis (7.3%), bile leakage (6.1%) and bile duct stricture (1.1%). Although most donors finally recover, some might unfortunately suffer from persistent symptoms possibly caused by surgical complications or the surgery itself. Ongoing symptoms such as abdominal discomfort, fatigue, chronic pain and scar itching,[18-21]albeit mild, might undermine donors' daily life. Irrespective of medical complications, most living liver donors remain in good physical condition postoperatively, if not as well as they were prior to surgery.[22-24]
Mental health
Regarding psychological health post-donation, psychiatric complications receive particular attention. Fukunishi et al[21]demonstrated that three cases without a psychiatric history exhibited paradoxical psychiatric syndrome post-donation. Trotter et al[3]also reported that 4.1% of 392 liver donors had one or multiple psychiatric complications. Other psychological problems such as low self-esteem,[25,26]enhanced stress and decreased confidence were also reported. These data remind us that the mental health of donors should not be neglected in long-term follow-up, which facilitates detecting and solving occult psychiatric problems before they get worse. However, only a small number of centers recognize the importance of prolonged post-donation monitoring and keep track of donor complications over time.[27]Equally as important as prolonged donor monitoring after operation, a well-designed pre-donation workup helps to identify those prone to compromised mental health after donation. Chan et al[28]published a workup scheme for donors undergoing urgent liver transplantation, which was shown to expedite initial evaluation, assure donor safety and allow timely operation. Regardless of psychiatric events, many donors claim that they have benefited from the process,[18-20]and even a great part of them are willing to donate again.[18,24,29-32]On the whole, living liver donors obtain improved mental well-being in the long-term follow-up period.[23,25,31,33]
Psychosocial health
The psychosocial aspect of the HRQoL of liver donors after operation is increasingly being recognized in addition to the physical and mental aspects, as recent evidence showed that some living liver donors experience psychosocial stress after donation.[34]Here, we concentrated on the interpersonal, vocational and financial impact.
Interpersonal impact
In LDLT, the relationship between the donor and the recipient is ethically mandated to be biological or legitimate in most countries. Therefore LDLT has a bearing on the intimacy between the donors and the recipients or between the donors and their families. Fortunately, a majority of donors reported an improved or stable relationship compared with the preoperative situation.[18,19,25,31,35]In contrast, those who feel coerced preoperatively either by medical teams, families, recipients or themselves might end up with unfavorable interpersonal outcomes. They may complain of suffering more than anticipated or having a worse relationship with the recipients and their families due to interference by voluntarism during the decision-making process. Fujita et al[36]established a five-stage decision-making model to help professionals to understand the donors' feelings and offer sufficient support. In this way, donors are more likely to face up to negative outcomes that might be generated.
Vocational impact
Due to the operation and postoperative recuperation, donor performance in school or workplace is inevitably affected. Some donors are able to return to pre-donation employment, and some may have to turn to lightduty jobs or are laid-off due to compromised physical and mental status, while others may have to resume working probably due to financial burdens. Although impaired ability may render donors unfit for their predonation occupation, Holtzman et al[37]showed that 96% of donors received encouragement from school or workplace for their decision, which implies that the donation experience promotes the donors' identity in their workplace or school and their intimacy with coworkers (Table 1).
Financial impact
LDLT is slightly more costly than cadaveric transplantation, presumably due to the higher incidence of complications with LDLT.[24,41]Though donationrelated expenses are covered by the recipients' insurance and inpatient costs are covered by a universal healthcare system, donors still have to pay most of the outpatient costs. In addition, it was pointed out that employers and insurance companies are reluctant to pay the incomethat employees lose due to donation.[42]As a result, the costs of transportation, loss of work hours, medications, babysitters and phone calls are usually not reimbursed. In this case, donors, especially those in poor economic condition or without insurance, might end up living on a budget or finding it hard to make ends meet (Table 2).
Evaluation tools
Multiple studies have examined the physical, mental and psychosocial HRQoL in living liver donors using a wide variety of surveys, which are generally categorized into generic and disease-specific measurements (Table 3). One of the advantages of applying generic instrumentssuch as 36-item short-form survery (SF-36) is that they make comparison among different diseases possible and monitor overall health conditions. In contrast, disease-specific instruments such as the chronic liver disease questionnaire can identify disease-specific changes that might be overlooked by generic tools.[48]Jay et al[49]concluded that the development of targeted instruments improves HRQoL assessment in recipients and helps identify factors that influence their wellbeing. Therefore, we need an integrated instrument or an appropriate combination of both generic and liver transplant-specific characteristics to improve the accuracy of long-term evaluation of donor HRQoL.
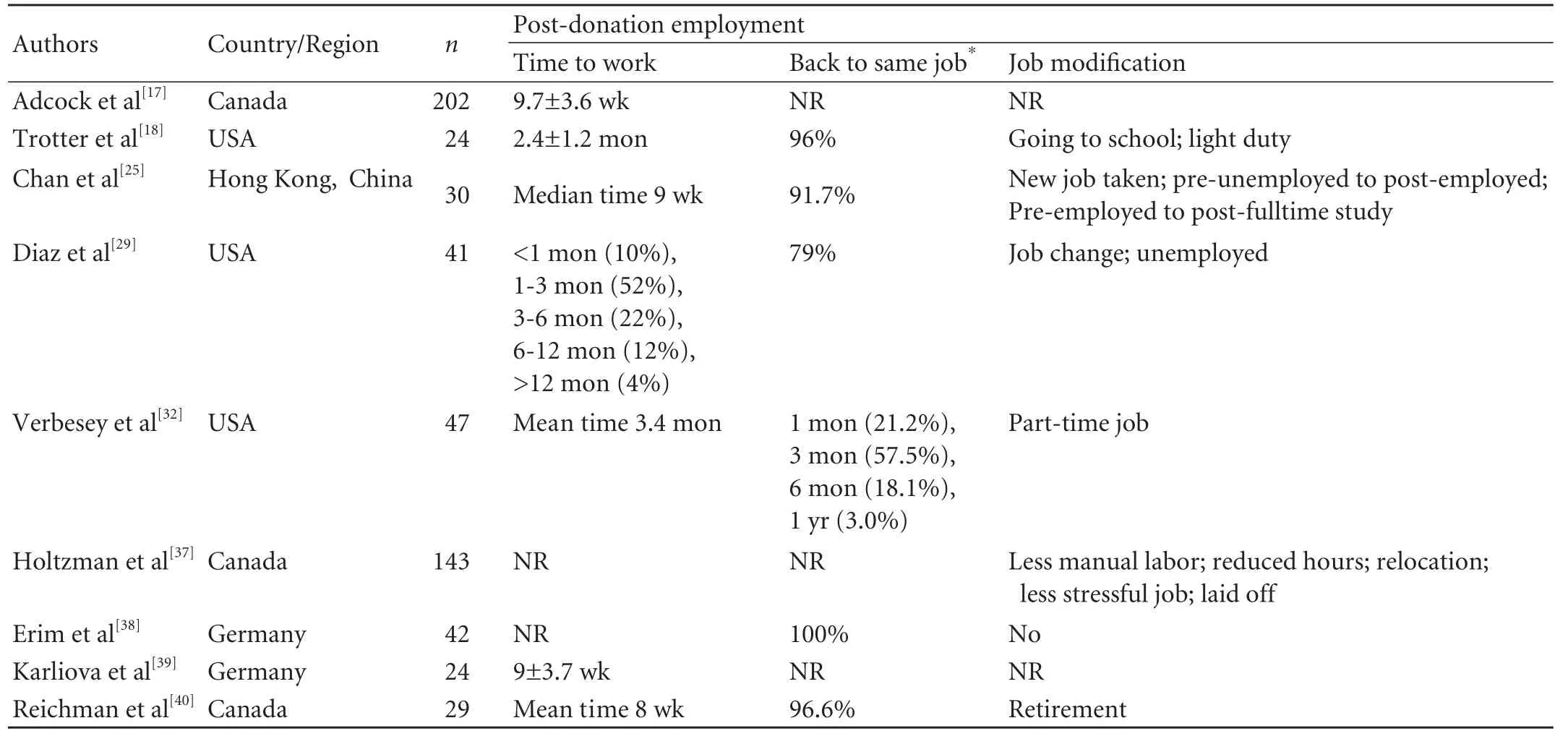
Table 1. Post-donation employment among living liver donors
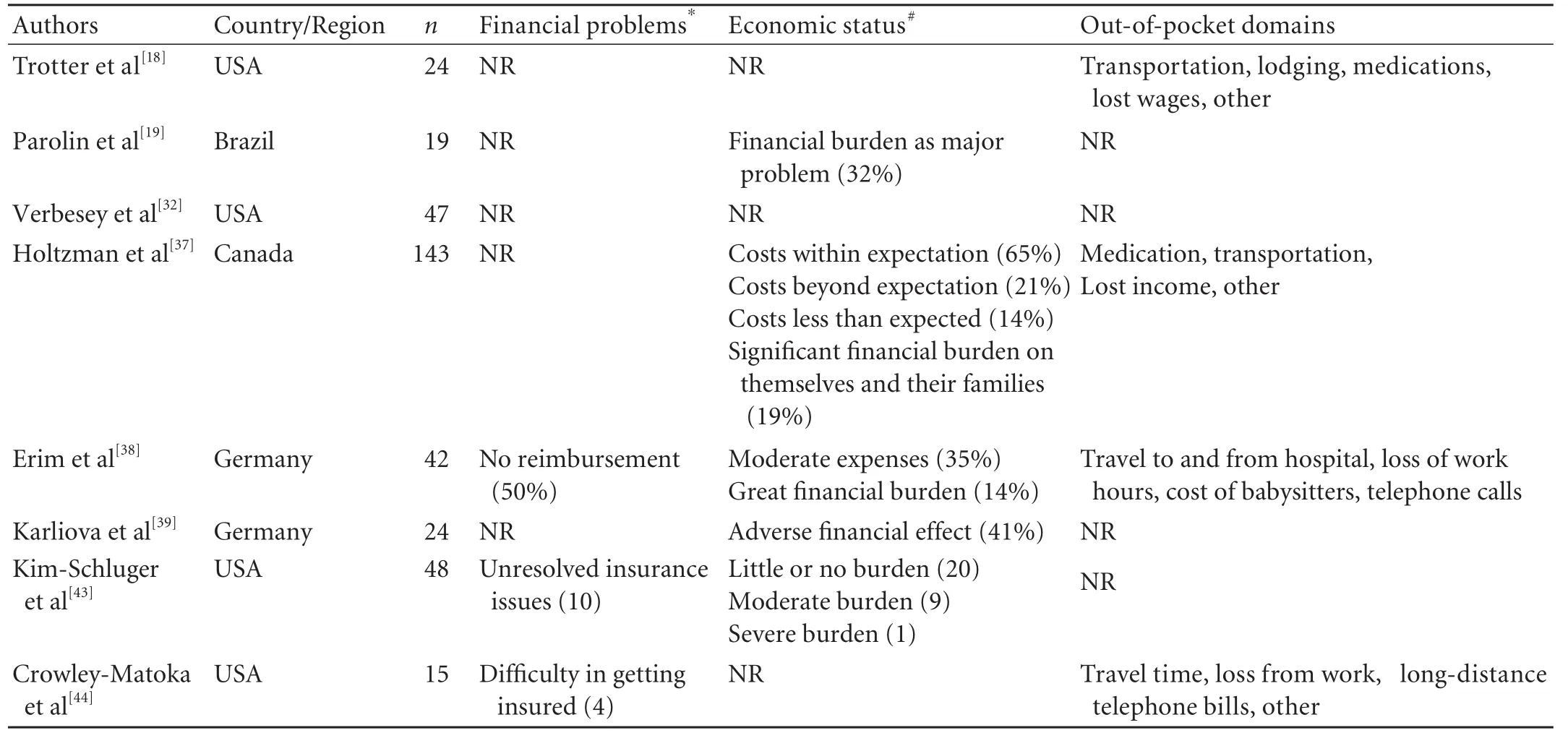
Table 2. Financial problems experienced by living liver donors after donation
Conclusion and perspectives
In conclusion, living liver donors generally experience good physical and mental quality of life after transplantation, whereas quite a number suffer from financial burdens, unfavorable changes in employment, or interpersonal relationship changes with regard to psychosocial aspects. In a bid to achieve satisfactory outcomes in HRQoL at both the physical and psychosocial levels, steps should be taken to advocate standard follow-up protocols in every liver transplantation center, better guaranteeing the process of informed consent and promoting multidisciplinary cooperation.
Only with a multidisciplinary perioperative modality can an LDLT be accomplished in favor of both the donor and the recipient.[50]It is imperative for health care professionals to cooperate throughout liver transplantation from donor selection to postoperative follow-up. Preoperatively, radiologists, hepatologists and psychiatrists need to work together to assess the suitability of potential donors and the selection of those eligible as well as providing support and assistance in thedecision-making process, which occasionally involves social workers familiar with liver transplantation. During the operation and the period immediately after operation, cooperation between surgeons, anesthetists and nurses is indispensable throughout the surgery and monitoring. Long after the operation, support may be needed from local governments, philanthropic organizations and even the media to help disadvantaged donors and families to overcome financial difficulties, and resume a normal life as before donation.

Table 3. Collected series: long-term quality of life assessment in living liver donors
Finally, although great efforts have been made to overcome the liver source challenge by expanding the donor pool,[51,52]in order to cure terminally ill people and sustain intact the well-being of a healthy individual, we should take advantage of the emerging techniques of regenerative medicine to produce livers in vitro to optimize organ sources.
Funding:None.
Ethical approval:Not needed.
Contributors:CPX wrote the main body of the article under the supervision of YLN. YLN provided advice on medical aspects. YLN is the guarantor.
Competing interest:No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
1 Surman OS, Cosimi AB, Fukunishi I, Kawaii T, Findley J, Kita Y, et al. Some ethical and psychiatric aspects of right-lobe liver transplantation in the United States and Japan. Psychosomatics 2002;43:347-353.
2 Papachristou C, Walter M, Frommer J, Klapp BF. A model of risk and protective factors influencing the postoperative course of living liver donors. Transplant Proc 2009;41:1682-1686.
3 Trotter JF, Hill-Callahan MM, Gillespie BW, Nielsen CA, Saab S, Shrestha R, et al. Severe psychiatric problems in right hepatic lobe donors for living donor liver transplantation. Transplantation 2007;83:1506-1508.
4 Brown RS Jr, Russo MW, Lai M, Shiffman ML, Richardson MC, Everhart JE, et al. A survey of liver transplantation from living adult donors in the United States. N Engl J Med 2003; 348:818-825.
5 Lo CM. Complications and long-term outcome of living liver donors: a survey of 1,508 cases in five Asian centers. Transplantation 2003;75:S12-15.
6 Umeshita K, Fujiwara K, Kiyosawa K, Makuuchi M, Satomi S, Sugimachi K, et al. Operative morbidity of living liver donors in Japan. Lancet 2003;362:687-690.
7 Beavers KL, Sandler RS, Shrestha R. Donor morbidity associated with right lobectomy for living donor liver transplantation to adult recipients: a systematic review. Liver Transpl 2002;8:110-117.
8 Middleton PF, Duffield M, Lynch SV, Padbury RT, House T, Stanton P, et al. Living donor liver transplantation--adult donor outcomes: a systematic review. Liver Transpl 2006;12:24-30.
9 Hashikura Y, Ichida T, Umeshita K, Kawasaki S, Mizokami M, Mochida S, et al. Donor complications associated with living donor liver transplantation in Japan. Transplantation 2009; 88:110-114.
10 Ghobrial RM, Freise CE, Trotter JF, Tong L, Ojo AO, Fair JH, et al. Donor morbidity after living donation for liver transplantation. Gastroenterology 2008;135:468-476.
11 Shih FJ, Hu RH, Ho MC, Lin HY, Lin MH, Lee PH. Changes in health-related quality of life and working competence before and after liver transplantation. Transplant Proc 2000; 32:2144-2148.
12 Goff JS, Glazner J, Bilir BM. Measuring outcome after liver transplantation: a critical review. Liver Transpl Surg 1998;4: 189-196.
13 Shih FJ, Lee PH, Wang JD, Hu RH, Lai MK, Lin HY, et al. Changes in quality of life and working capacity before and after kidney transplantation. Transplant Proc 1999;31:1981-1984.
14 Schlenk EA, Erlen JA, Dunbar-Jacob J, McDowell J, Engberg S, Sereika SM, et al. Health-related quality of life in chronic disorders: a comparison across studies using the MOS SF-36. Qual Life Res 1998;7:57-65.
15 McHorney CA, Ware JE Jr, Raczek AE. The MOS 36-Item Short-Form Health Survey (SF-36): II. Psychometric and clinical tests of validity in measuring physical and mental health constructs. Med Care 1993;31:247-263.
16 Ran S, Wen TF, Yan LN, Li B, Zeng Y, Chen ZY, et al. Risks faced by donors of right lobe for living donor liver transplantation. Hepatobiliary Pancreat Dis Int 2009;8:581-585.
17 Adcock L, Macleod C, Dubay D, Greig PD, Cattral MS, McGilvray I, et al. Adult living liver donors have excellent long-term medical outcomes: the University of Toronto liver transplant experience. Am J Transplant 2010;10:364-371.
18 Trotter JF, Talamantes M, McClure M, Wachs M, Bak T, Trouillot T, et al. Right hepatic lobe donation for living donor liver transplantation: impact on donor quality of life. Liver Transpl 2001;7:485-493.
19 Parolin MB, Lazzaretti CT, Lima JH, Freitas AC, Matias JE, Coelho JC. Donor quality of life after living donor liver transplantation. Transplant Proc 2004;36:912-913.
20 Miyagi S, Kawagishi N, Fujimori K, Sekiguchi S, Fukumori T, Akamatsu Y, et al. Risks of donation and quality of donors' life after living donor liver transplantation. Transpl Int 2005; 18:47-51.
21 Fukunishi I, Sugawara Y, Makuuchi M, Surman OS. Pain in liver donors. Psychosomatics 2003;44:172-173.
22 Pascher A, Sauer IM, Walter M, Lopez-Haeninnen E, Theruvath T, Spinelli A, et al. Donor evaluation, donor risks, donor outcome, and donor quality of life in adult-to-adult living donor liver transplantation. Liver Transpl 2002;8:829-837.
23 Basaran O, Karakayali H, Emiroğlu R, Tezel E, Moray G, Haberal M. Donor safety and quality of life after left hepatic lobe donation in living-donor liver transplantation. Transplant Proc 2003;35:2768-2769.
24 DuBay DA, Holtzman S, Adcock L, Abbey S, Greenwood S, Macleod C, et al. Adult right-lobe living liver donors: quality of life, attitudes and predictors of donor outcomes. Am J Transplant 2009;9:1169-1178.
25 Chan SC, Liu CL, Lo CM, Lam BK, Lee EW, Fan ST. Donor quality of life before and after adult-to-adult right liver live donor liver transplantation. Liver Transpl 2006;12:1529-1536.
26 DuBay DA, Holtzman S, Adcock L, Abbey SE, Greenwood S, Macleod C, et al. Cosmesis and body image after adult right lobe living liver donation. Transplantation 2010;89:1270-1275.
27 Beavers KL, Cassara JE, Shrestha R. Practice patterns for long-term follow-up of adult-to-adult right lobectomy donors at US transplantation centers. Liver Transpl 2003;9:645-648.
28 Chan SC, Fan ST, Liu CL, Lo CM, Lam BK, Lee EW. Working up donors for high-urgency and elective adult-to-adult live donor liver transplantation. Liver Transpl 2007;13:509-515.
29 Diaz GC, Renz JF, Mudge C, Roberts JP, Ascher NL, Emond JC, et al. Donor health assessment after living-donor liver transplantation. Ann Surg 2002;236:120-126.
30 Kusakabe T, Irie S, Ito N, Kazuma K. Feelings of living donors about adult-to-adult living donor liver transplantation. Gastroenterol Nurs 2008;31:263-272.
31 Humar A. Donor and recipient outcomes after adult living donor liver transplantation. Liver Transpl 2003;9:S42-44.
32 Verbesey JE, Simpson MA, Pomposelli JJ, Richman E, Bracken AM, Garrigan K, et al. Living donor adult liver transplantation: a longitudinal study of the donor's quality of life. Am J Transplant 2005;5:2770-2777.
33 Schulz KH, Kroencke S, Beckmann M, Nadalin S, Paul A, Fischer L, et al. Mental and physical quality of life in actual living liver donors versus potential living liver donors: a prospective, controlled, multicenter study. Liver Transpl 2009;15:1676-1687.
34 Walter M, Papachristou C, Fliege H, Hildebrandt M, Pascher A, Steinmüller T, et al. Psychosocial stress of living donors after living donor liver transplantation. Transplant Proc 2002;34:3291-3192.
35 Walter M, Bronner E, Pascher A, Steinmüller T, Neuhaus P, Klapp BF, et al. Psychosocial outcome of living donors after living donor liver transplantation: a pilot study. Clin Transplant 2002;16:339-344.
36 Fujita M, Akabayashi A, Slingsby BT, Kosugi S, Fujimoto Y, Tanaka K. A model of donors' decision-making in adult-toadult living donor liver transplantation in Japan: having no choice. Liver Transpl 2006;12:768-774.
37 Holtzman S, Adcock L, Dubay DA, Therapondos G, KashfiA, Greenwood S, et al. Financial, vocational, and interpersonal impact of living liver donation. Liver Transpl 2009;15:1435-1442.
38 Erim Y, Beckmann M, Valentin-Gamazo C, Malago M, Frilling A, Schlaak JF, et al. Quality of life and psychiatric complications after adult living donor liver transplantation. Liver Transpl 2006;12:1782-1790.
39 Karliova M, Malagó M, Valentin-Gamazo C, Reimer J, Treichel U, Franke GH, et al. Living-related liver transplantation from the view of the donor: a 1-year follow-up survey. Transplantation 2002;73:1799-1804.
40 Reichman TW, Fox A, Adcock L, Wright L, Abbey SE, Levy G, et al. Anonymous living liver donation: donor profiles and outcomes. Am J Transplant 2010;10:2099-2104.
41 Hayashi PH, Trotter JF. Review article: adult-to-adult right hepatic lobe living donor liver transplantation. Aliment Pharmacol Ther 2002;16:1833-1841.
42 Wigmore SJ, Forsythe JJ. Living-related liver transplantation from the view of the donor: a 1-year follow-up survey. Transplantation 2002;73:1799. Transplantation 2002;73:1701-1702.
43 Kim-Schluger L, Florman SS, Schiano T, O'Rourke M, Gagliardi R, Drooker M, et al. Quality of life after lobectomy for adult liver transplantation. Transplantation 2002;73:1593-1597.
44 Crowley-Matoka M, Siegler M, Cronin DC 2nd. Long-term quality of life issues among adult-to-pediatric living liver donors: a qualitative exploration. Am J Transplant 2004;4: 744-750.
45 Beavers KL, Sandler RS, Fair JH, Johnson MW, Shrestha R. The living donor experience: donor health assessment and outcomes after living donor liver transplantation. Liver Transpl 2001;7:943-947.
46 Walter M, Dammann G, Papachristou C, Pascher A, Neuhaus P, Danzer G, et al. Quality of life of living donors before and after living donor liver transplantation. Transplant Proc 2003;35:2961-2963.
47 Jin SG, Yan LN, Li B, Wen TF, Zhao JC, Zeng Y, et al. Quality of life and psychologic distress of recipients after adult livingdonor liver transplantation (LDLT)-A study from mainland China. Transplant Proc 2010;42:2611-2616.
48 Pomfret EA. What is the quality-of-life after live liver donation? Am J Transplant 2004;4:673-674.
49 Jay CL, Butt Z, Ladner DP, Skaro AI, Abecassis MM. A review of quality of life instruments used in liver transplantation. J Hepatol 2009;51:949-959.
50 Hwang GS, McCluskey SA. Anesthesia and outcome after partial hepatectomy for adult-to-adult donor transplantation. Curr Opin Organ Transplant 2010;15:377-382.
51 Levy GA. Progress in transplantation. Ther Drug Monit 2010;32:246-249.
52 Varo Pérez E, Castroagudín JF. The future of liver transplantation. Varo Pérez E, Castroagudín JF. Transplant Proc 2010;42:613-616.
Received November 26, 2010
Accepted after revision April 14, 2011
Author Affiliations: Division of Liver Transplantation, West China Hospital, Sichuan University, Chengdu 610041, China (Chen PX and Yan LN)
Lu-Nan Yan, MD, PhD, Division of Liver Transplantation, West China Hospital, Sichuan University, Chengdu 610041, China (Tel: 86-28-81812453; Fax: 86-28-85423724; Email: yanlunan688@ 163.com)
© 2011, Hepatobiliary Pancreat Dis Int. All rights reserved.
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- Prognostic role of diabetes mellitus in hepatocellular carcinoma patients after curative treatments: a meta-analysis
- Risk factors of severe ischemic biliary complications after liver transplantation
- Surgical treatment of Budd-Chiari syndrome: analysis of 221 cases
- Efficacy of liver transplantation for acute hepatic failure: a single-center experience
- Combined invagination and duct-to-mucosa techniques with modifications: a new method of pancreaticojejunal anastomosis
- Large regenerative nodules in a patient with Budd-Chiari syndrome after TIPS positioning while on the liver transplantation list diagnosed by Gd-EOB-DTPA MRI
