Synchronous gastric adenocarcinoma and pancreatic ductal adenocarcinoma
2010-12-14MirkoMuroniFrancescoAngeloMassimoPezzatiniSimoneSebastianiSamanthaNotoEmanuelaPilozziandGiovanniRamacciato
Mirko Muroni, Francesco D'Angelo, Massimo Pezzatini, Simone Sebastiani,Samantha Noto, Emanuela Pilozzi and Giovanni Ramacciato
Rome, Italy
Synchronous gastric adenocarcinoma and pancreatic ductal adenocarcinoma
Mirko Muroni, Francesco D'Angelo, Massimo Pezzatini, Simone Sebastiani,Samantha Noto, Emanuela Pilozzi and Giovanni Ramacciato
Rome, Italy
(Hepatobiliary Pancreat Dis Int 2010; 9: 97-99)
synchronous double cancer;gastric carcinoma;pancreatic carcinoma
Introduction
Recently an increase of the incidence of multiple primary cancers has been observed, and cases of two or more malignant primary tumors have appeared with a high frequency in the literature. The incidence of multiple primary malignant tumors is expected to increase with age.[1]We report a case of gastric adenocarcinoma associated with pancreatic ductal adenocarcinoma.
Case report
A 73-year-old woman was referred to the Department of Surgery of our hospital for persistent vomiting and weight loss during hospitalization at the Department of Diabetology for uncontrolled hyperglycemia.
Laboratory tests on admission showed evidence of anemia (HB 10.8 g/dl), PCR 1.4 mg/dl, and abnormal tumor markers levels: CEA 9.58 ng/ml (normal range 0.00-3.00), CA125 39.70 IU/ml (normal range 0.00-35.00),CA19-9 165.80 IU/ml (normal range 0.00-37.00), TPA 108 U/L (normal range 2.00-75.00).
Esophagogastroduodenoscopy demonstrated a large antral ulcerative lesion extending circumferentially in the gastric antrum and causing pyloric stenosis. Histological examination revealed an adenocarcinoma.
Abdominal CT showed thickening of the gastric wall to the antral and pyloric portion of the stomach (around 40 mm), and a solid lesion in the uncinate portion of the pancreas (around 25×12 mm), with vanishing limits,necrotic areas, and no evidence of distant metastases.
MRI showed a pancreas of reduced volume and con fi rmed alterations at the uncinate portion due to the presence of a nodular mass of around 3×1.7 cm, with a fl uid component in its context. The formation was characterized by vanishing pro fi les and adhesions to the anterior wall of the third duodenal portion. A strict adhesion was suggested to the superior mesenteric vein.

Fig. 1. CT of the upper abdomen showing thickening of the gastric wall in the antral and pyloric portion of the stomach,and a solid lesion in the uncinate portion of the pancreas with vanishing limits and necrotic areas.

Fig. 2. MRI demonstrating pancreas with structural alterations at the uncinate portion and a nodular mass with a fl uid component in the context. The formation appeared with a vanishing pro fi le and was strictly adherent to the anterior wall of the third duodenal portion.
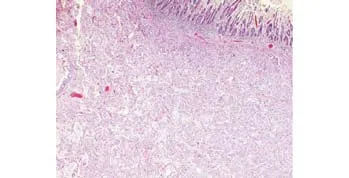
Fig. 3. Colloidal adenocarcinoma of the pancreas invading the duodenum (HE staining, original magni fi cation ×2.5).
The biopsy taken during the esophagogastroduodenoscopy revealed an adenocarcinoma.
The patient was transferred to the Department of Surgery for pancreaticoduodenectomy according to Whipple with regional Fortner type Ⅰ extension (SMV resection).
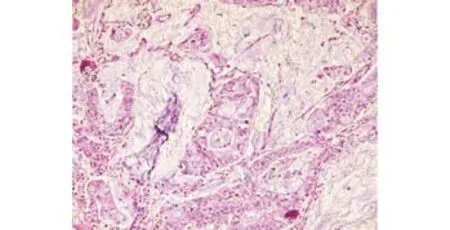
Fig. 4. Colloidal adenocarcinoma of the pancreas. Pools of mucin are primarily extracellular in location. The tumor is composed of irregular glands or clumps of cells lying free in mucinous lakes. There is evident nuclear atypia (HE staining, original magni fi cation ×10).

Fig. 5. Adenocarcinoma of the stomach. There is residual normal mucosa in the lower left corner (HE staining, original magni fi cation ×2.5).

Fig. 6. Adenocarcinoma of the stomach, Lauren intestinal typeⅡ. The tumor is composed of well-formed glands (HE staining,original magni fi cation ×10).
Final histology demonstrated a ductal adenocarcinoma of the pancreas (G3) with a mucinous type colloidal component (40% of the neoplasm) and an intraductal cystic papillary mucinous component. The neoplasm in fi ltrated the duodenum wall, peripancreatic tissue, and the segment of mesenteric vein. One of the seven peripancreatic lymph nodes sampled was positive for neoplasm (pT3, pN1, pMx, G3 V1 R0).
The gastric neoplasm was a moderately differentiated gastric adenocarcinoma (G2) with gastric mural invasion up to the subserous fat (Pt2B), and it was of Lauren intestinal type. The vascular invasion of the tumor was histologically con fi rmed (V1) (pT2b, pN0,pMx, G2 V1). None of the 24 lymph nodes has shown a center of metastases. The patient did not receive any adjuvant treatment.chronous gastric adenocarcinoma and pancreatic ductal adenocarcinoma. Surgical resection remains the only potentially curative treatment for adenocarcinoma of the stomach and pancreas. Long survival is rare in patients with pancreatic cancer. Despite the advanced age of the patient and the synchronous cancer of the pancreas, we consider surgical intervention is a chance for the patient to prolong her life and improve its life quality by feeding again.
Discussion
Cases of double synchronous cancers involving the stomach and pancreas are relatively rare.[2,3]In patients with gastric carcinoma, the prevalence of second tumors varies from 2.8% to 6.8%.[4]The incidence of gastric carcinoma associated with pancreatic carcinoma accounts for 3.8% in all cases of gastric carcinoma associated with carcinoma of other organs.[2,5]
In the present case, gastric neoplasm was diagnosed by esophagogastroduodenoscopy. The symptoms of the patient included weight loss and recurrent vomiting due to the neoplasm causing stenosis of the pilorus and hindering the progression of the food bolus. A characteristic symptom was also anemia caused by the ulcerated mass.
CT scan performed during preoperative evaluation revealed the presence of a synchronous neoplasm of the pancreas. Abdominal MRI subsequently showed changes in the uncinate portion of the pancreas and the presence of a nodular mass of around 3×1.7 cm was con fi rmed. This lesion was strictly adherent to the anterior wall of the third duodenal portion and to the superior mesenteric vein.
Pancreatoduodenectomy combined with resection of the superior mesenteric vein was performed according to the Fortner type Ⅰ regional pancreatectomy. The vein was repaired by end-to-end vascular anastomosis.[6-8]
After the intervention, the patient was maintained on parenteral nutrition for 9 days and subsequently a liquid diet was given. An elementary diet was started on the 14th postoperative day.
In conclusion, this is an unusual case of syn-
Funding: None.
Ethical approval: Not needed.
Contributors: MM wrote the fi rst draft of this commentary. All authors contributed to the intellectual context and approved the fi nal version. MM is the guarantor.
Competing interest: No bene fi ts in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
1 Eriguchi N, Aoyagi S, Hara M, Okuda K, Tamae T, Fukuda S, et al. Synchronous or metachronous double cancers of the pancreas and other organs: report on 12 cases. Surg Today 2000;30:718-721.
2 Miyaguni T, Muto Y, Kusano T, Yamada M, Matsumoto M,Shiraishi M. Synchronous double cancers of the remnant stomach and pancreas: report of a case. Surg Today 1995;25:1038-1042.
3 Goh BK, Loh HL, Soo KC. Synchronous pancreatic serous cystic tumor, intraductal papillary mucinous tumor and gastric carcinoma: report of a case. Pancreas 2005;31:195-197.
4 Lundegårdh G, Hansson LE, Nyrén O, Adami HO, Krusemo UB. The risk of gastrointestinal and other primary malignant diseases following gastric cancer. Acta Oncol 1991;30:1-6.
5 Eriguchi N, Aoyagi S, Hara M, Okuda K, Tamae T, Fukuda S,et al. A case of synchronous double cancers of the pancreas and stomach. Kurume Med J 2000;47:169-171.
6 Fortner JG, Kim DK, Cubilla A, Turnbull A, Pahnke LD, Shils ME. Regional pancreatectomy: en bloc pancreatic, portal vein and lymph node resection. Ann Surg 1977;186: 42-50.
7 Fortner JG. Regional pancreatectomy for cancer of the pancreas, ampulla, and other related sites. Tumor staging and results. Ann Surg 1984;199:418-425.
8 Shibata C, Kobari M, Tsuchiya T, Arai K, Anzai R, Takahashi M, et al. Pancreatectomy combined with superior mesentericportal vein resection for adenocarcinoma in pancreas. World J Surg 2001;25:1002- 1005.
BACKGROUND: The association between gastric and pancreatic carcinoma is a relatively rare condition. In gastric carcinoma patients, the prevalence of second tumors varies 2.8% to 6.8% according to the reported statistics. Gastric cancer associated with pancreatic cancer is uncommon.
METHODS: We report a case of a 73-year-old patient hospitalized for vomiting and weight loss. Esophagogastroduodenoscopy demonstrated an ulcerative lesion of the gastric antrum. Computed tomography and magnetic resonance showed a gastric thickening in the antral and pyloric portion and a nodular mass (3×1.7 cm) in the uncinate portion of the pancreas.
RESULTS: The patient underwent pancreaticoduoden-ectomy according to Whipple regional type Ⅰ Fortner. Histological examination of the specimen demonstrated a moderately differentiated adenocarcinoma of the stomach and a poorly differentiated ductal adenocarcinoma of the pancreas.
CONCLUSIONS: Long survival is rare in patients with associated gastric and pancreatic cancer. Surgical resection remains the only potentially curative treatment.
Author Af fi liations: Department of General Surgery (Muroni M,D'Angelo F, Pezzatini M, Sebastiani S and Ramacciato G), and Department of Pathology (Noto S and Pilozzi E), La Sapienza University of Rome,Second School of Medicine, St. Andrea Hospital, via di Grottarossa 1035,00189 Rome, Italy
Mirko Muroni, MD, Department of General Surgery, La Sapienza University of Rome, St. Andrea Hospital, viale Gino Cervi 53 L, 00139, Rome, Italy (Fax: 0039-06-33775322; Email:mirkomuroni@libero.it).
© 2010, Hepatobiliary Pancreat Dis Int. All rights reserved.
January 13, 2009
Accepted after revision August 12, 2009
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- Thrombosis of gallbladder vein presenting as acute peritonitis
- Liver transplantation for acute intermittent porphyria: a viable treatment?
- Contrast-free air cholangiography-assisted unilateral plastic stenting in malignant hilar biliary obstruction
- Growth inhibition induced by short hairpin RNA to silence survivin gene in human pancreatic cancer cells
- Outpatient versus inpatient laparoscopic cholecystectomy: a single center clinical analysis
- Primary hepatic neuroendocrine carcinoma:clinical analysis of 11 cases