Contrast-free air cholangiography-assisted unilateral plastic stenting in malignant hilar biliary obstruction
2010-12-14VirendraSinghGurpreetSinghVikasGuptaRajeshGuptaandRakeshKapoor
Virendra Singh, Gurpreet Singh, Vikas Gupta, Rajesh Gupta and Rakesh Kapoor
Chandigarh, India
Contrast-free air cholangiography-assisted unilateral plastic stenting in malignant hilar biliary obstruction
Virendra Singh, Gurpreet Singh, Vikas Gupta, Rajesh Gupta and Rakesh Kapoor
Chandigarh, India
(Hepatobiliary Pancreat Dis Int 2010; 9: 88-92)
air cholangiogram;hilar obstruction;malignant;plastic stent;metal stent;unilateral
Introduction
Management of unresectable malignant hilar biliary obstruction is challenging. Magnetic resonance cholangiopancreatography (MRCP)is a choice for de fi ning the anatomic extent of hilar tumors and making stenting feasible before therapeutic endoscopic retrograde cholangiopancreatography (ERCP).[1-4]However,it is costly. Cannulation and contrast injection of an occluded bile duct after ERCP and incomplete drainage precipitate infection.[5-8]There are reports on the use of contrast-free methods[9]or MRCP and/or CT to selectively target endoscopic placement of metal stents with encouraging results.[4,10,11]However, MRCP and metal stents are costly. In a recent study we demonstrated the safety and ef fi cacy of contrast-free unilateral balloon-assisted plastic stenting in patients with type Ⅱmalignant hilar biliary obstruction,[12]but this method is not possible to de fi ne the biliary anatomy before deploying the stent. Therefore, we studied the outcome of air cholangiography-assisted unilateral plastic stenting in patients with type Ⅱ malignant hilar biliary obstruction.
Methods
From January 2007 to December 2008, 10 patients withunresectable carcinoma of the gallbladder with typeⅡ malignant hilar biliary obstruction were included in the study. The diagnosis was based on ultrasound or computed tomography with ultrasound-guided fi ne needle aspiration cytology. The type of hilar stricture was de fi ned on the basis of Bismuth's classi fi cation[13]with the help of MRCP. Successful drainage was de fi ned as a loss of pruritus and a 30% fall in bilirubin in 30 days.[14]All patients were given prophylactic antibiotics,and this medication was continued for 5 days after the procedure. ERCP was done without any contrast and a guidewire (Jag-Wire, Boston Scienti fi c, Natick, Mass)was passed deep inside the right or left duct (Fig. 1). A small amount of air was injected above the suspected site of hilar stricture under fl uoroscopic control and the right/left duct was visualized (Fig. 2). After visualizing the right/left duct, the catheter was withdrawn below the site of stricture without pulling the guidewire and again a small amount of air was injected below the stricture under fl uoroscopic control, visualizing the type of stricture (Fig. 3). Unilateral 10 Fr, 10/12 cm Amsterdamtype plastic stents were placed above the stricture as identi fi ed by air cholangiography (Fig. 4). The successful stent insertion was con fi rmed by fl ow of bile through the stent. The patients were re-evaluated at one week and then at monthly intervals. A retrospectively analyzed group of 10 patients treated with contrast-free unilateral metal stenting served as controls.
Informed consent was obtained from all patients.The Ethics Committee of the Postgraduate Institute of Medical Education and Research, Chandigarh, approved the study. Baseline characteristics of the patients were expressed as mean (SD). Patient characteristics were compared between the two groups by Student's t test or the Chi-square test with Yates' correction for continuity as appropriate. Kaplan-Meier life-table analysis-estimated cumulative survival and curves were compared by the log-rank test and the Chi-square test. A P value <0.05 was considered statistically signi fi cant.

Fig. 1. Contrast-free guidewire cannulation of the right hepatic duct.

Fig. 2. Air cholangiogram visualizing the right ductal system.

Fig. 3. Air cholangiogram visualizing the right ductal system with the infrahilar bile duct.
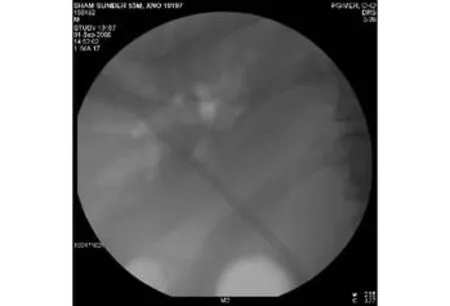
Fig. 4. Plastic stent being placed across the stricture.
Results
The 10 patients with type Ⅱ malignant hilar biliary obstruction were treated with contrast-free air cholangiography-assisted unilateral plastic stenting. A retrospectively analyzed group of 10 patients treated with contrast-free unilateral metal stenting served as controls.The baseline clinical and biochemical characteristics are shown in Table 1. Air cholangiography detected type Ⅱmalignant hilar biliary obstruction in all patients, as did by MRCP. Successful stent insertion was achieved in all patients. Drainage was successful in all patients in both groups (Table 2). In patients with successful drainage,pruritus disappeared, bilirubin level decreased, and anorexia improved. There were no major complications.One patient in each group developed mild pancreatitis,which improved after conservative treatment. No 30-day mortality occurred.
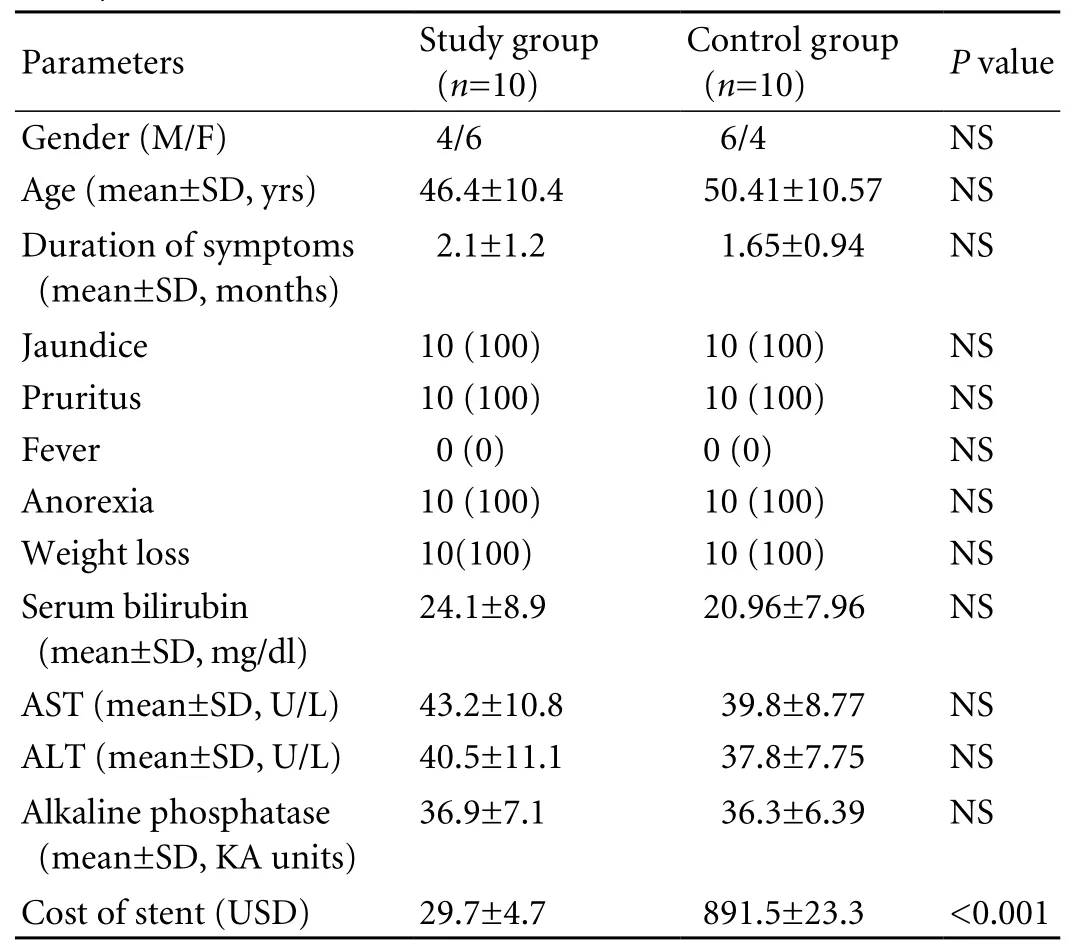
Table 1. Baseline characteristics of patients with malignant hilar biliary obstruction
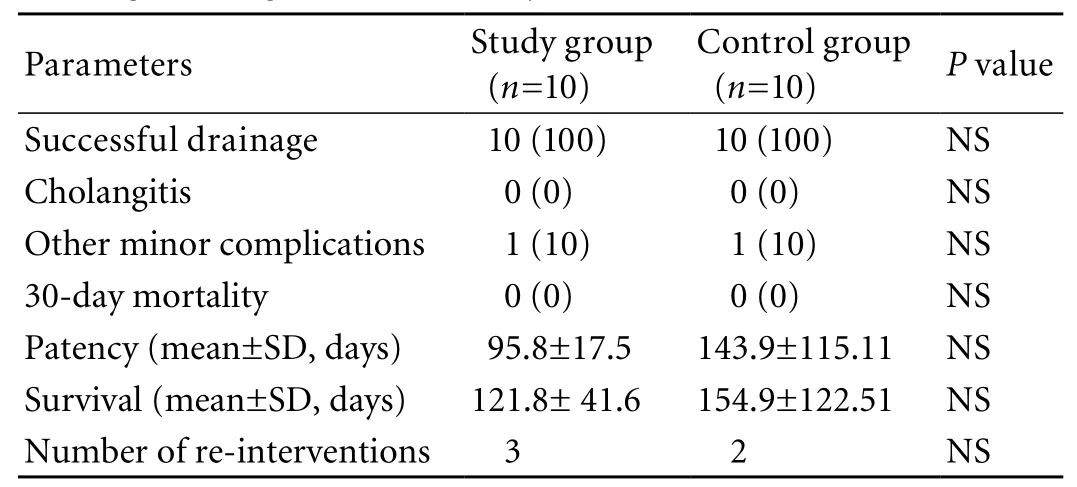
Table 2. Comparison of contrast-free air cholangiography-assisted unilateral plastic stenting and contrast-free unilateral metal stenting in malignant hilar biliary obstruction
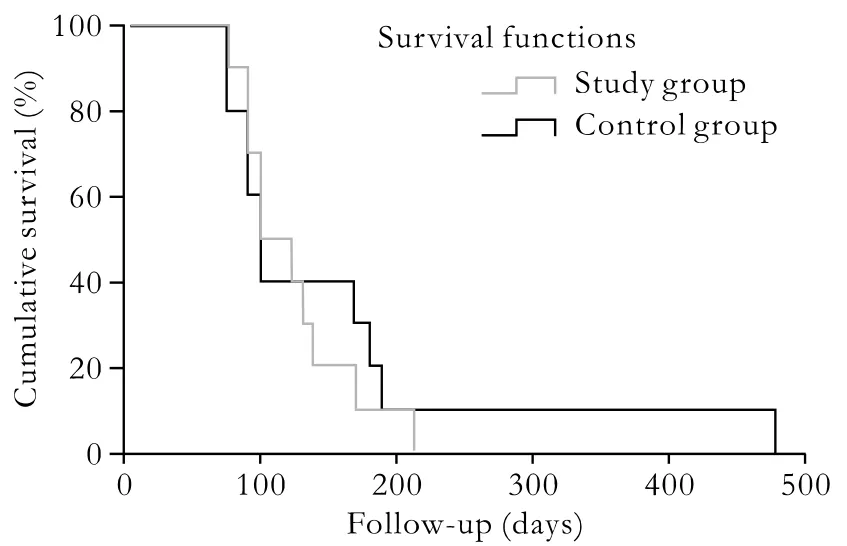
Fig. 5. Kaplan-Meier survival curves. Cumulative survival of patients treated with air cholangiography-assisted unilateral plastic stent and contrast-free unilateral metal stent. At the end of the observation period, none of the patients in either group was alive.
On follow-up, the mean patency after initial stent placement was 95.8±17.5 days (range 75-130 days) in the study group and 143.9±115.11 days (range 75-450 days) in the control group (P=0.20) (Table 2). The mean survival was 121.8±41.6 days (range 75-210 days) in the study group and 154.9±122.51 days (range 75-480 days)in the control group (P=0.42) (Table 2). The Kaplan-Meier method showed an estimated median survival of 100∶95% CI (65.9, 134.1) days in the study group and 98∶95% CI (84.1, 111.9) days in the control group(P=0.62) (Fig. 5). Three patients in the study group and 2 in the control group required re-intervention due to stent blockage (P>0.05).
Discussion
MRCP as an increasingly recognized imaging technique in the evaluation of hilar strictures provides a detailed cholangiographic map noninvasively.[1-3]The accuracy of MRCP in the evaluation of intraductal tumor extension ranges from 78% to 84% in two recent studies and is comparable to ERCP.[1,15]In the present study, air cholangiography detected type Ⅱobstruction in 100% patients, as did by MRCP. With the help of air cholangiography, it is possible to de fi ne the biliary anatomy on the ipsilateral side above and below the hilum. However, it is not possible to assess the contralateral suprahilar ducts and it has been shown that right or left unilateral drainage is effective.[16,17]There is no study on air cholangiography in the management of malignant hilar biliary obstruction.
Endoscopic drainage of patients with malignant hilar biliary obstruction is a palliative treatment of choice; however, it is technically dif fi cult. There are con fl icting reports regarding unilateral or bilateral stenting in these patients.[5,16-19]Deviere et al[5]found that bilateral drainage is better than unilateral drainage.Polydorou et al[17]compared the results of right versus left hepatic duct endoprosthesis insertion and showed similar successful drainage and a 30-day mortality, and they concluded that more than one stent is not justi fi ed as a routine procedure in patients with malignant hilar biliary obstruction. It is known that only 25%-30% of the liver volume needs to be drained to achieve adequate palliation with improved clinical, biochemical, and radiological parameters.[20]Cholangitis after ERCP and stent insertion occurs in 5%-38% of patients and is the result of contrast injection above the stricture without adequate drainage of all opaci fi ed ducts.[21]Chang et al[18]demonstrated the best survival if both lobes are drained and the worst survival if both lobes are opaci fi ed and only one is drained. In a randomized study of 157 consecutive patients with malignant hilar obstruction De Palma et al[16]found that unilateral drainage is associated with a signi fi cantly higher successful drainage (81% vs. 73%, P=0.049) and a lower rate of cholangitis (8% vs. 16%, P=0.013) with a minimal contrast injection above the stricture.
Recently, CT- or MRCP-guided stenting of the targeted hepatic lobe has been done.[4,10]Hintze et al[4]reported a high successful drainage (86%) and a low cholangitis (6%) in a study of 35 patients with types Ⅲand Ⅳ hilar obstruction with MRCP-guided unilateral stenting with minimal contrast injection above the stricture. Freeman and Overby[10]found that MRCP and/or CT-guided unilateral metal stenting in 35 patients with malignant hilar biliary obstruction provided safe and effective palliation in most patients. Tytgat et al[22]pointed out that in type Ⅱ or Ⅲ hilar strictures there is a risk of cholangitis in the undrained lobe, even if no contrast is seen entering it. In the absence of contrast contamination, there may be an increased risk of cholangitis in an obstructed segment related to a rise in intrabiliary pressure leading to disruption of the tight junctions between hepatocytes, impaired Kupffer cell function, and lack of clearance of contaminants which occurs with normal bile fl ow.[23]In a recent study we demonstrated the safety and usefulness of the contrastfree method of unilateral metal stenting in 18 patients with type Ⅱ malignant hilar biliary obstruction.[9]In another study, contrast-free plastic stenting in 20 patients with malignant biliary obstruction showed promising results.[24]However, there were only two patients with hilar obstruction in this study and plastic stents were placed without de fi nite localization of stricture. But successful stent insertion was achieved in all patients without cholangitis or 30-day mortality.In another pilot study, we demonstrated the safety and ef fi cacy of unilateral contrast-free balloon-assisted plastic stenting in 15 patients with type Ⅱ malignant hilar biliary obstruction; however, it was not possible to de fi ne the biliary anatomy before deploying the stent.[12]In the present study, all patients in both groups had successful drainage and none developed cholangitis or died within 30 days. Metal stents have been shown to have longer patency than plastic stents;[25,26]however, the longer patency of metal stents failed to reach statistical signi fi cance. There is no study on air cholangiographyassisted unilateral plastic stenting in malignant hilar biliary obstruction.
In conclusion, air cholangiography-assisted plastic stenting is as safe and effective as contrast-free unilateral metal stenting in patients with type Ⅱ malignant hilar biliary obstruction for palliation, but at a fraction of the cost. However, a larger study is required.
Funding: None.
Ethical approval: Not needed.
Contributors: SV proposed the study and wrote the fi rst draft.All authors contributed to the patient enrollment and follow-up.SV is the guarantor.
Competing interest: No bene fi ts in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
1 Zidi SH, Prat F, Le Guen O, Rondeau Y, Pelletier G. Performance characteristics of magnetic resonance cholangiography in the staging of malignant hilar strictures. Gut 2000;46:103-106.
2 Yeh TS, Jan YY, Tseng JH, Chiu CT, Chen TC, Hwang TL, et al.Malignant perihilar biliary obstruction: magnetic resonance ch olangiopancreatographic fi ndings. Am J Gastroenterol 2000;95:432-440.
3 Lee MG, Lee HJ, Kim MH, Kang EM, Kim YH, Lee SG, et al.Extrahepatic biliary diseases: 3D MR cholangiopancreatography compared with endoscopic retrograde cholangiopancreatography.Radiology 1997;202:663-669.
4 Hintze RE, Abou-Rebyeh H, Adler A, Veltzke-Schlieker W, Felix R, Wiedenmann B. Magnetic resonance cholangiopancreatography-guided unilateral endoscopic stent placement for Klatskin tumors. Gastrointest Endosc 2001;53:40-46.
5 Deviere J, Baize M, de Toeuf J, Cremer M. Long-term follow-up of patients with hilar malignant stricture treated by endoscopic internal biliary drainage. Gastrointest Endosc 1988;34:95-101.
6 Huibregtse K, Tytgat GN. Palliative treatment of obstructive jaundice by transpapillary introduction of large bore bile duct endoprosthesis. Gut 1982;23:371-375.
7 Dutta SK, Cox M, Williams RB, Eisenstat TE, Standiford HC.Prospective evaluation of the risk of bacteremia and the role of antibiotics in ERCP. J Clin Gastroenterol 1983;5:325-329.
8 McMahon LF Jr, Gorelick FS. ERCP and bacteremia. J Clin Gastroenterol 1983;5:358-359.
9 Singh V, Singh G, Verma GR, Singh K, Gulati M. Contrastfree unilateral endoscopic palliation in malignant hilar biliary obstruction: new method. J Gastroenterol Hepatol 2004;19:589-592.
10 Freeman ML, Overby C. Selective MRCP and CT-targeted drainage of malignant hilar biliary obstruction with selfexpanding metallic stents. Gastrointest Endosc 2003;58:41-49.
11 De Palma GD, Pezzullo A, Rega M, Persico M, Patrone F, Mastantuono L, et al. Unilateral placement of metallic stents for malignant hilar obstruction: a prospective study.Gastrointest Endosc 2003;58:50-53.
12 Singh V, Singh G, Verma GR, Gupta V, Gupta R, Kapoor R, et al. Contrast-free balloon-assisted unilateral plastic stenting in malignant hilar biliary obstruction: a new method. Dig Endosc 2008;20:190-193.
13 Bismuth H, Corlette MB. Intrahepatic cholangioenteric anastomosis in carcinoma of the hilus of the liver. Surg Gynecol Obstet 1975;140:170-178.
14 Polydorou AA, Cairns SR, Dowsett JF, Hat fi eld AR, Salmon PR, Cotton PB, et al. Palliation of proximal malignant biliary obstruction by endoscopic endoprosthesis insertion. Gut 1991;32:685-689.
15 Manfredi R, Masselli G, Maresca G, Brizi MG, Vecchioli A, Marano P. MR imaging and MRCP of hilar cholangiocarcinoma. Abdom Imaging 2003;28:319-325.
16 De Palma GD, Galloro G, Siciliano S, Iovino P, Catanzano C.Unilateral versus bilateral endoscopic hepatic duct drainage in patients with malignant hilar biliary obstruction: results of a prospective, randomized, and controlled study. Gastrointest Endosc 2001;53:547-553.
17 Polydorou AA, Chisholm EM, Romanos AA, Dowsett JF,Cotton PB, Hat fi eld AR, et al. A comparison of right versus left hepatic duct endoprosthesis insertion in malignant hilar biliary obstruction. Endoscopy 1989;21:266-271.
18 Chang WH, Kortan P, Haber GB. Outcome in patients with bifurcation tumors who undergo unilateral versus bilateral hepatic duct drainage. Gastrointest Endosc 1998;47:354-362.
19 Ducreux M, Liguory C, Lefebvre JF, Ink O, Choury A, Fritsch J,et al. Management of malignant hilar biliary obstruction by endoscopy. Results and prognostic factors. Dig Dis Sci 1992;37:778-783.
20 Dowsett JF, Vaira D, Hat fi eld AR, Cairns SR, Polydorou A,Frost R, et al. Endoscopic biliary therapy using the combined percutaneous and endoscopic technique. Gastroenterology 1989;96:1180-1186.
21 Larghi A, Tringali A, Lecca PG, Giordano M, Costamagna G.Management of hilar biliary strictures. Am J Gastroenterol 2008;103:458-473.
22 Tytgat GN, Bartelsman JF, Den Hertog Jager FC, Huibregtse K, Mathus-Vliegen EM. Upper intestinal and biliary tract endoprosthesis. Dig Dis Sci 1986;31:57S-76S.
23 Sung JY, Costerton JW, Shaffer EA. Defense system in the biliary tract against bacterial infection. Dig Dis Sci 1992;37:689-696.
24 De Palma GD, Lombardi G, Rega M, Simeoli I, Masone S,Siciliano S, et al. Contrast-free endoscopic stent insertion in malignant biliary obstruction. World J Gastroenterol 2007;13:3973-3976.
25 Peters RA, Williams SG, Lombard M, Karani J, Westaby D.The management of high-grade hilar strictures by endoscopic insertion of self-expanding metal endoprostheses. Endoscopy 1997;29:10-16.
26 Davids PH, Groen AK, Rauws EA, Tytgat GN, Huibregtse K. Randomised trial of self-expanding metal stents versus polyethylene stents for distal malignant biliary obstruction.Lancet 1992;340:1488-1492.
BACKGROUND: Endoscopic palliation in malignant hilar biliary obstruction requires endoscopic retrograde cholangiopancreatography (ERCP), whereas contrast injection leads to cholangitis. Contrast-free metal stenting with or without magnetic resonance cholangiopancreatography (MRCP) has shown encouraging results, but MRCP and metal stents are costly. There have been no reports on the use of air cholangiography.
METHODS: We prospectively evaluated the role of air cholangiography-assisted unilateral plastic stenting in 10 patients with type Ⅱ malignant hilar biliary obstruction. A retrospectively analysed group of 10 patients treated with contrast-free unilateral metal stenting served as historical controls.
RESULTS: Ten patients with unresectable type Ⅱ malignant hilar biliary obstruction were studied. Air cholangiography detected type Ⅱ obstruction in all patients, similar to MRCP.The patients underwent unilateral stenting. Successful endoscopic drainage was achieved in all patients. The mean patency of the stent was 95.8±17.5 days in the study group and 143.9±115.1 days in the control group (P=0.20). The mean survival was 121.8±41.6 days in the study group and 154.9±122.5 days in the control group (P=0.42). Kaplan-Meier analysis showed an estimated median survival of 100∶95% CI (65.9, 134.1) days in the study group and 98∶95% CI (84.1, 111.9) days in the control group (P=0.62).Cholangitis occurred in none of the patients and there were no 30-day deaths nor major complications. Air cholangiographyassisted unilateral plastic stenting was cheaper than contrastfree unilateral metal stenting.
CONCLUSION: Air cholangiography-assisted unilateral plastic stenting is as safe and effective as contrast-free unilateral metal stenting in type Ⅱ malignant hilar biliary obstruction for palliating patients, but it is cheaper.
Author Af fi liations: Departments of Hepatology (Singh V), Surgery (Singh G, Gupta V and Gupta R), and Radiotherapy (Kapoor R), Postgraduate Institute of Medical Education and Research, Chandigarh-160012, India
Virendra Singh, MD, Additional Professor of Hepatology, Department of Hepatology, Postgraduate Institute of Medical Education and Research, Chandigarh-160012, India (Fax: 0172-2744401;Email:virendrasingh100@hotmail.com)
© 2010, Hepatobiliary Pancreat Dis Int. All rights reserved.
September 24, 2009
Accepted after revision December 1, 2009
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- Thrombosis of gallbladder vein presenting as acute peritonitis
- Synchronous gastric adenocarcinoma and pancreatic ductal adenocarcinoma
- Liver transplantation for acute intermittent porphyria: a viable treatment?
- Growth inhibition induced by short hairpin RNA to silence survivin gene in human pancreatic cancer cells
- Outpatient versus inpatient laparoscopic cholecystectomy: a single center clinical analysis
- Primary hepatic neuroendocrine carcinoma:clinical analysis of 11 cases