Endoscopic nasojejunal feeding tube placement in patients with severe hepatopancreatobiliary diseases:a retrospective study of 184 patients
2010-12-14FengJiJingLiZhaoXiJinChunHuaJiaoYuYaoHuQinWeiXuandWeiXingChen
Feng Ji, Jing-Li Zhao, Xi Jin, Chun-Hua Jiao, Yu-Yao Hu, Qin-Wei Xu and Wei-Xing Chen
Hangzhou, China
Endoscopic nasojejunal feeding tube placement in patients with severe hepatopancreatobiliary diseases:a retrospective study of 184 patients
Feng Ji, Jing-Li Zhao, Xi Jin, Chun-Hua Jiao, Yu-Yao Hu, Qin-Wei Xu and Wei-Xing Chen
Hangzhou, China
(Hepatobiliary Pancreat Dis Int 2010; 9: 54-59)
tube feeding, nasojejunal;endoscopy;parenteral nutrition, total;hepatobiliary disease;pancreatic disease
Introduction
Severe hepatopancreatobiliary (HPB) diseases create a catabolic stress state promoting a systemic in fl ammatory response and nutritional deterioration. They remain potentially lethal without any speci fi c proven treatment. Nutritional support plays an important role in the management of patients with such diseases.[1-3]As an important method of enteral nutrition (EN), endoscopic nasojejunal feeding tube placement (ENFTP) has been increasingly common. It can solve the EN problem of patients with severe HPB diseases who have the complications of mechanical obstruction or gastric emptying disturbance in the upper gastrointestinal (UGI) tract. Besides, it is suitable for patients with severe pancreatitis to avoid the problem of pancreatic exocrine activity induced by food stimulation in the cephalic and gastric phases.[4]It has been convincingly demonstrated in numerous studies that ENFTP is preferable to total parenteral nutrition(TPN) as it leads to signi fi cantly better glycemic control,maintains intestinal structure and function, improvesthe immune response, and decreases gastrointestinal complications, infection rate, mortality, length of hospital stay, and hospital costs.[5-7]The aim of this study was to assess the clinical value of ENFTP in patients with severe HPB diseases and compare it with TPN.
MethodsPatients
A prospective study was conducted in patients with severe HPB diseases, and complete clinical data were collected from the wards of the First Af fi liated Hospital,Zhejiang University School of Medicine, Hangzhou,China, between January 2001 and April 2008. During a 4-week observation period, 184 patients were consecutively and synchronously enrolled. Of these patients, 88 received ENFTP support and 96 received TPN. There were no statistical differences in age, sex,weight, height, disease composition, acute physiology,and chronic health evaluation Ⅱ (APACHE Ⅱ) score between the two groups at admission (Table 1).
Experimental groups

Fig. 1. Placement of a N-J tube in a patient with gastroplegia after liver transplantation. A: Gastroscopic image from the patient with large volume of gastric residuals; B: a N-J tube placed at the jejunum through the biopsy channel of the gastroscope under visual control.
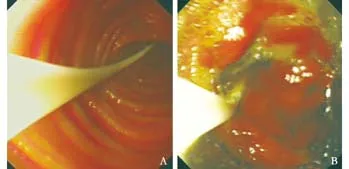
Fig. 2. A gastroscopic N-J tube placed in a patient with functional delayed gastric emptying after pancreatoduodenectomy for pancreatic head carcinoma. The tube was placed at the jejunum (A)and afferent loop (B) via a gastroscope under visual control.
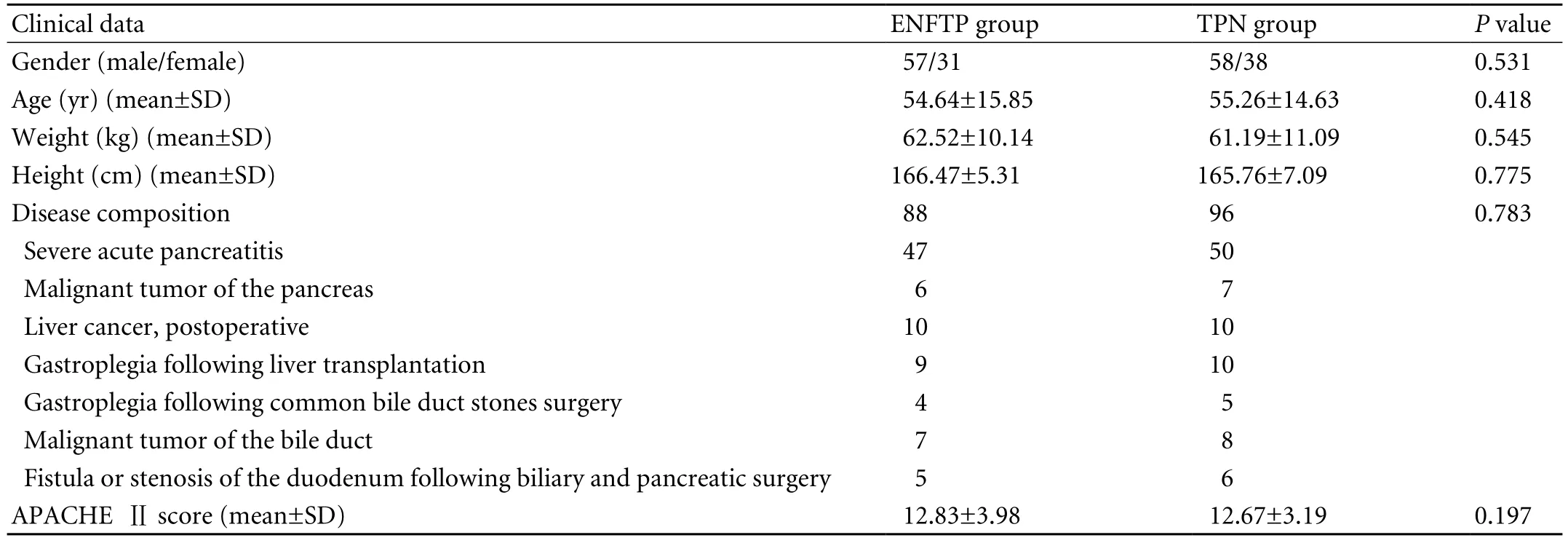
Table 1. Demographic data, disease distribution, and severity score of ENFTP and TPN groups at admission
In the ENFTP group, a nasojejunal (N-J) tube (size 8FR, length 240 cm, NJFT-8, Wilson-Cook Medical Inc.,USA) was placed at the upper jejunum or the horizontal part of the duodenum through the biopsy channel of the gastroscope (GIF-XQ 240 or -V70, Olympus, Japan),except for patients with serious mechanical obstruction of the UGI so that the gastroscope could not reach the site (Figs. 1-3). The proximal end was passed through the nose by a nasal catheter and fi xed on the cheek.The volume and concentration of EN suspension was increased gradually (from an initial concentration of 8%-10% to the sustaining concentration of 20%-25%)according to the patients' tolerance, and the temperature was kept at about 40 ℃ using an electric warmer. On the fi rst day, 500 ml of 5% glucose saline was infused slowly via the N-J tube at a rate of 40-60 ml/h. The next day, 500 ml EN suspension with complete protein or dietary fi ber was infused at the same rate as the fi rst day.On the third day, the volume could be increased to 1000 ml at a rate of 60-80 ml/h. During the fourth to seventh days, as well as the following three weeks, 1000-2000 ml was infused at a rate of 100-120 ml/h. Mostly, EN suspension was infused by gravity drip or an infusion pump, especially in critically ill patients. With regard to those patients who could not tolerate ENFTP completely in the beginning, underfeeding was compensated with partial parenteral nutrition until they could fully tolerate it. To avoid obstruction, the tube was washed with 20-30 ml warm water every 4 hours during the continuous infusion, as well as before and after infusion.
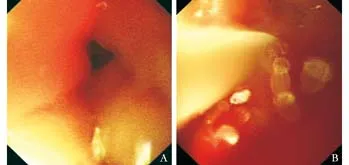
Fig. 3. A gastroscopic N-J tube placed in a patient with duodenum stricture for gallbladder cancer invasion. A: Gastroscopic image of the stricture hole 4 mm in diameter; B: a N-J tube placed at the jejunum by inserting it into the stricture hole gastroscopically.
Measurement indices
Levels of hemoglobin, red blood cell count, lymphocyte count, serum glucose, prealbumin, total protein,albumin, creatinine, cholesterol, triglyceride, and calcium were measured at baseline and after 1, 2, and 4 weeks of nutritional support. Besides, complication rate,mortality, nutritional support time, mean nutrition cost,mechanical ventilation time, mean time in intensive care unit (ICU), duration of hospital stay, and APACHE Ⅱscore were also analyzed. Since the level of amylase is not related to nutritional state, we did not consider it.
Statistical analysis
Measurement data are expressed as mean±SD and were analyzed by Student's t test, while categorical data were analyzed by the Chi-square test. Analysis of variance (ANOVA) for repeated measurement was used for self control comparison and group comparison. SPSS 13.0 was used to analyze the data. A P value less than 0.05 was regarded as statistically signi fi cant.
Results
After 4 weeks of nutritional support, the levels of hemoglobin, red blood cell count, and prealbumin rose more in the ENFTP group than in the TPN group(P<0.05). The fasting blood glucose levels of the groupsboth decreased signi fi cantly while the decrease was more notable in the ENFTP group (P<0.05). The lymphocyte count and blood calcium levels rose conspicuously(P<0.05), but there was no statistical difference between the two groups. Group and self control comparisons of levels of total serum protein, albumin, creatinine,blood cholesterol, and triglyceride showed no statistical difference (Table 2). Besides, compared with the TPN group, the ENFTP group had a signi fi cantly lower incidence of nosocomial infection, septicemia,peripancreatic infection, abdominal infection, biliary infection, multiple organ dysfunction syndrome (MODS),and hyperglycemia, as well as shorter nutritional support time and length of hospital stay, lower daily nutrition cost, and improved APACHE Ⅱ score (Table 3). However,N-J feeding did not reduce the incidence of pulmonary infection, acute respiratory distress syndrome (ARDS),GI tract bleeding, intestinal obstruction, pancreatic pseudocyst, mechanical ventilation time, length of ICU stay, and total mortality (Table 3).
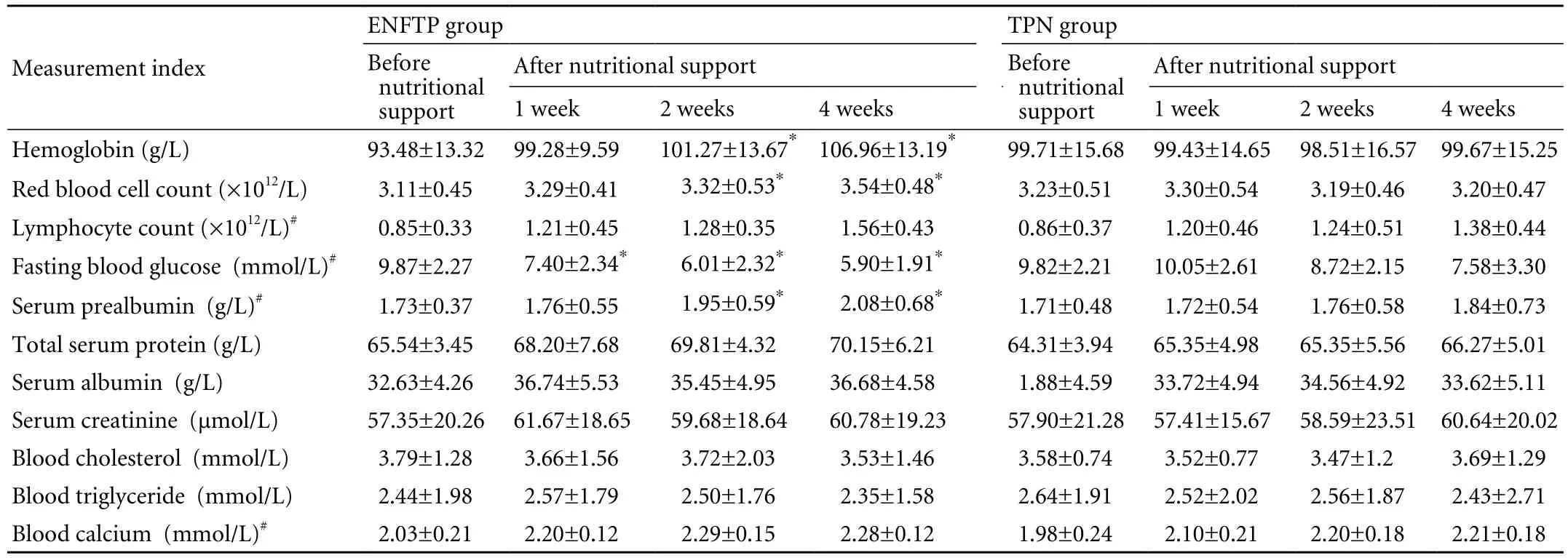
Table 2. Comparison of laboratory indices between the ENFTP and TPN groups (mean±SD)
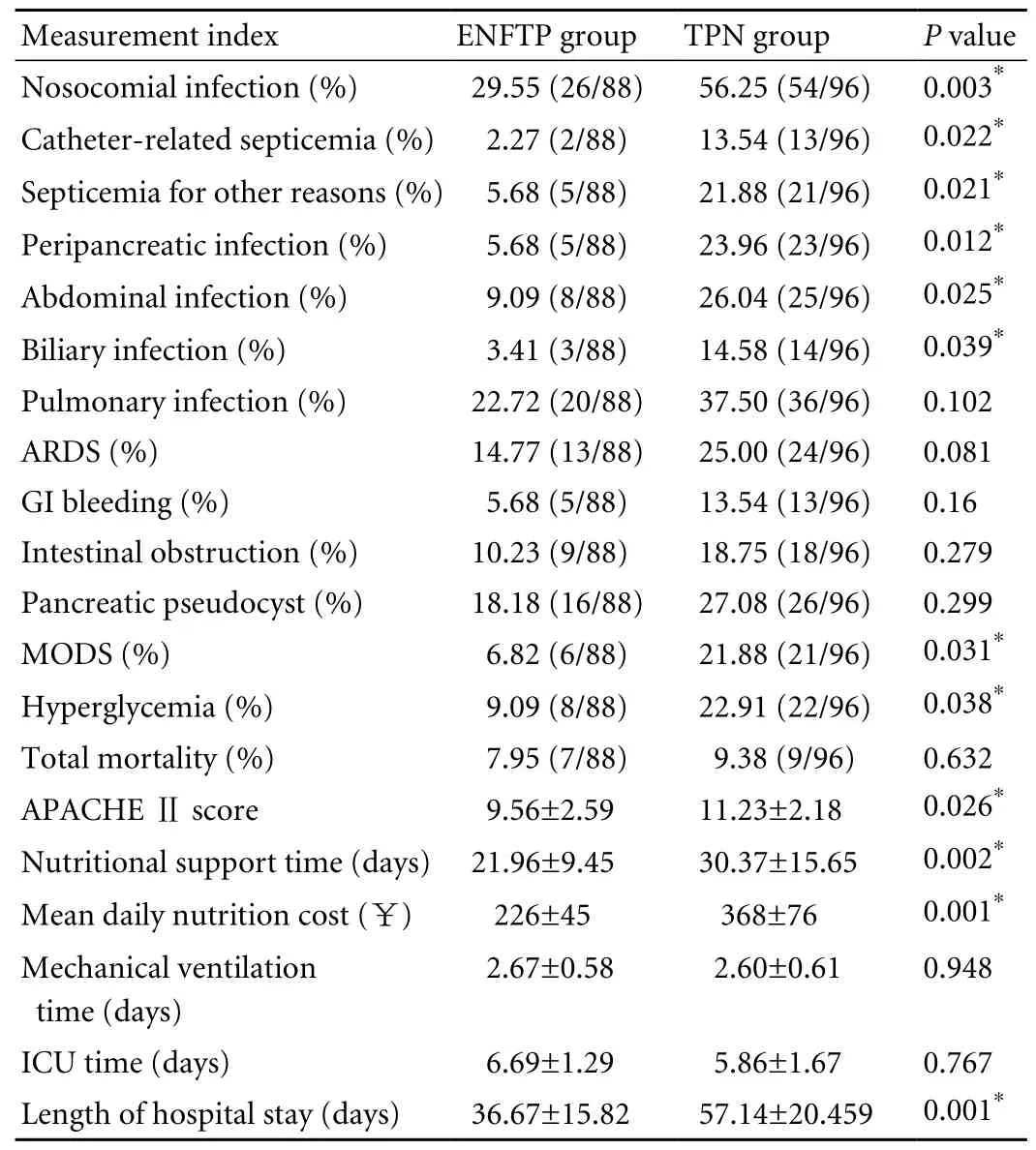
Table 3. Comparison of non-laboratory indices between the ENFTP and TPN groups
Discussion
Patients with severe HPB diseases are always in a state of stress and hypermetabolism, which is accompanied by progressive weight loss, malnutrition, and depressed immune function. This results in disease progression and poor prognosis. Since underfeeding may aggravate the clinical condition,[8]nutritional support is regarded as an essential component of management by improving nutritional status and immune function. Though TPN still occupies an important position in the nutritional support of patients with severe HPB diseases,[9]several studies have shown that long-term use of TPN may suppress immune function, destroy the intestinal barrier, increase the permeability of intestinal mucosa resulting in abnormal colonization of intestinal fl ora and endotoxemia,[10]and fi nally induce intestinal failure and MODS. On the contrary, EN can improve nutritional status and effectively promote intestinal function. Several randomized clinical trials have shown that EN is much more effective and economical than TPN.[5-7]Accumulating clinical evidence shows that EN improves survival and reduces the complications accompanying severe HPB diseases. The explanations are complex and related to the following:[11]a) EN avoids TPN complications; b) Luminal nutrition maintains intestinal health; c) Enteral amino acids are more effective in supporting splanchnic protein synthesis;d) EN may prevent the progression to multiple organ failure. Considering that these patients always have the complications of UGI mechanical obstruction or gastric emptying disturbance and the problem of pancreatic secretion during an attack of acute pancreatitis, the application of mouth-gastric EN is restricted. Therefore,ENFTP is a practicable method of EN at present.[12]Nevertheless, no related clinical research has been reported so far.
This study systematically evaluated the clinical value of ENFTP in patients with severe HPB diseases,and compared it with TPN. The results showed that ENFTP signi fi cantly raised the levels of hemoglobin,red blood cell count and prealbumin, and decreased the level of hyperglycemia. Hemoglobin and red blood cell count showed rising trends in the ENFTP group,while changing less in the TPN group. This might be related to destruction of red blood cells and hemoglobin as the plasma osmotic pressure was changed by the intravenous nutrition fl uid. The prealbumin level rose more markedly in the ENFTP than in the TPN group,indicating that ENFTP promoted the recovery of hepatic function more effectively in patients with severe HPB diseases. It is known that hyperglycemia in critically ill patients is associated with increased risk of infectious complications and mortality, while good control of blood glucose can improve the prognosis.[5,13,14]Our research showed that the fasting blood glucose level decreased more noably in the ENFTP group,indicating that ENFTP enhanced basal secretion of insulin and consumption of peripheral glucose, thereby antagonizing the hazard of stress hyperglycemia.
In addition, it is assumed that better glycemic control in patients fed enterally may be associated with secretion of biochemical mediators in the gut and liver closer to physiological conditions,[15]while the glucose dosage is inaccurately calculated, the infusion rate is not individually controlled, or exogenous insulin is insuf fi ciently administered through the parenteral route.Because the decrease of lymphocyte count in critically ill patients is closely related to secondary infection and prolonged length of ICU stay, effective restoration of the decrease of lymphocyte count might improve their prognoses.[16]EN can restore immune function reduced by surgical trauma, and enhance humoral and cellular immune function postoperatively.[9]We found that the lymphocyte count of both groups increased conspicuously after nutritional support, indicating that both methods promoted the recovery of immunologic barrier function and improved the prognosis. In addition, comparison of levels of total serum protein,albumin, creatinine, blood cholesterol, and triglyceride showed no statistical difference, indicating that they had similar effects in reducing consumption of nutrient substances (e.g. protein, fat), negative nitrogen balance,and catabolic metabolism caused by operation or disease.
With respect to complications, Abou-Assi et al[17]conducted a randomized study comparing EN and TPN in two groups of patients with acute pancreatitis and found that the catheter-related infection rate was signi fi cantly lower in the EN than in the TPN group.Besides, Richter et al[18]reported that EN had a notable advantage in decreasing total incidence of infection and catheter-related infection. Our results are consistent with these studies. We found that the total incidence of complications was conspicuously higher in the TPN than in the ENFTP group, especially catheter-related septicemia, nosocomial infection, peripancreatic infection, and biliary infection. This might be due to the fact that TPN worsens the in fl ammatory process,increases endotoxin exposure, leads to metabolic and electrolyte disturbances, alters the gut barrier by causing increased intestinal permeability, results in abnormal habitation of intestinal fl ora and endotoxemia, and develops sepsis and multiple organ failure.[19]On the contrary, EN enhances intestinal perfusion, preserves mucosal mass and intestinal microbial ecology, improves immune function, and reduces infections.[20]Topical nutrients are the most potent stimulators of mucosal regeneration by stimulating the release of growth factors and mucosal blood fl ow, probably due to the presence of the amino acid arginine which is a precursor of nitric oxide and growth factors.[11]In addition to its mucosal protective and immunomodulatory effects,EN is the most effective means of supporting intestinal metabolism.[11]By down-regulating splanchnic cytokine production and modulating the acute phase response,EN reduces catabolism and preserves protein.[21]
Our research showed that the ENFTP group had a signi fi cantly shorter nutritional support time and length of hospital stay and lower daily nutrition cost as reported elsewhere.[5-7]This might be due to the fact that the basal diseases and injuries of some vital organs (e.g.heart and lung) of the TPN group were aggravated as a result of a higher incidence of infection, and therefore a prolonged time of antibiotic use, nutritional support,and hospital stay was inevitably required. In contrast,ENFTP helps patients to change from arti fi cial feeding to an oral diet earlier, which promotes earlier recovery.In addition, EN with a diet enriched in glutamine has a bene fi cial effect on the recovery of IgG and IgM-proteins with a trend to shorter disease duration.[22]APACHE Ⅱ score is an objective marker in re fl ecting the severity of disease. Reports show that the APACHEⅡ score decreases more visibly after EN support than after TPN support, with a signi fi cant difference between the two.[16,21]In our study, ENFTP reduced the severity of patients' conditions more effectively and was signi fi cantly bene fi tial to their recovery, as the APACHEⅡ score decreased more notably in this group. However,in comparison with the TPN group, N-J feeding did not signi fi cantly decrease the incidence of pulmonary infection, ARDS, GI bleeding, intestinal obstruction, or pancreatic pseudocyst. This might be due to the fact that the incidence of these complications is not closely related to the improvement of intestinal barrier function. There was no signi fi cant difference in mechanical ventilation time, length of ICU stay and mortality between the two groups. This might be due to the fact that nutritional support is just an important part of systemic therapy and has no decisive action on some in fl uential factors in prognosis.
In conclusion, compared with TPN, ENFTP solves the EN problem of patients with severe HPB diseases who have mechanical obstruction or gastric emptying disturbance in the UGI, and pancreatic exocrine activity stimulated by ordinary EN during an attack of acute pancreatitis. It also improves nutritional indices (e.g.hemoglobin), decreases the incidence of complications(e.g. various infections), shortens nutritional support time and length of hospital stay, and promotes recovery.Therefore, ENFTP is an economic, safe, and effective method of nutritional support and deserves further clinical application.
Funding: None.
Ethical approval: Not needed.
Contributors: JF and ZJL proposed the study and wrote the fi rst draft. XJ, JCH, HYY and XQW analyzed the data. JF and CWX performed ENFTP. All authors contributed to the design and interpretation of the study and to further drafts. JF is the guarantor.Competing interest: No bene fi ts in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
1 Forsmark CE, Baillie J; AGA Institute Clinical Practice and Economics Committee; AGA Institute Governing Board. AGA Institute technical review on acute pancreatitis.Gastroenterology 2007;132:2022-2044.
2 Banks PA, Freeman ML; Practice Parameters Committee of the American College of Gastroenterology. Practice guidelines in acute pancreatitis. Am J Gastroenterol 2006;101:2379-2400.
3 Pezzilli R, Fantini L, Morselli-Labate AM. New approaches for the treatment of acute pancreatitis. JOP 2006;7:79-91.
4 Meier R, Ockenga J, Pertkiewicz M, Pap A, Milinic N, Mac fi e J,et al. ESPEN Guidelines on Enteral Nutrition: Pancreas. Clin Nutr 2006;25:275-284.
5 Petrov MS, Zagainov VE. In fl uence of enteral versus parenteral nutrition on blood glucose control in acute pancreatitis: a systematic review. Clin Nutr 2007;26:514- 523.6 McClave SA, Chang WK, Dhaliwal R, Heyland DK. Nutrition support in acute pancreatitis: a systematic review of the literature. JPEN J Parenter Enteral Nutr 2006;30:143-156.
7 Petrov MS, van Santvoort HC, Besselink MG, van der Heijden GJ, Windsor JA, Gooszen HG. Enteral nutrition and the risk of mortality and infectious complications in patients with severe acute pancreatitis: a meta-analysis of randomized trials. Arch Surg 2008;143:1111-1117.
8 Meier RF, Beglinger C. Nutrition in pancreatic diseases. Best Pract Res Clin Gastroenterol 2006;20:507-529.
9 Abou-Assi S, O'Keefe SJ. Nutrition in acute pancreatitis. J Clin Gastroenterol 2001;32:203-209.
10 Gramlich L, Taft AK. Acute pancreatitis: practical considerations in nutrition support. Curr Gastroenterol Rep 2007;9:323-328.
11 Ioannidis O, Lavrentieva A, Botsios D. Nutrition support in acute pancreatitis. JOP 2008;9:375-390.
12 McClave SA, Snider H, Owens N, Sexton LK. Clinical nutrition in pancreatitis. Dig Dis Sci 1997;42:2035-2044.
13 Van den Berghe G, Wilmer A, Hermans G, Meersseman W,Wouters PJ, Milants I, et al. Intensive insulin therapy in the medical ICU. N Engl J Med 2006;354:449-461.
14 van den Berghe G, Wouters P, Weekers F, Verwaest C,Bruyninckx F, Schetz M, et al. Intensive insulin therapy in the critically ill patients. N Engl J Med 2001;345:1359-1367.
15 Gianotti L, Braga M, Vignali A, Balzano G, Zerbi A, Bisagni P, et al. Effect of route of delivery and formulation of postoperative nutritional support in patients undergoing major operations for malignant neoplasms. Arch Surg 1997;132:1222-1230.
16 Lin L, Cai XJ, Pan KH. Apoptosis of circulating lymphocyte in surgical critically ill patients associated with poor outcome.Zhongguo Wei Zhong Bing Ji Jiu Yi Xue 2007;19:25-27.
17 Abou-Assi S, Craig K, O'Keefe SJ. Hypocaloric jejunal feeding is better than total parenteral nutrition in acute pancreatitis: results of a randomized comparative study. Am J Gastroenterol 2002;97:2255-2262.
18 Richter B, Schmandra TC, Golling M, Bechstein WO.Nutritional support after open liver resection: a systematic review. Dig Surg 2006;23:139-145.
19 Scolapio JS. A review of the trends in the use of enteral and parenteral nutrition support. J Clin Gastroenterol 2004;38:403-407.
20 Petrov MS, Kukosh MV, Emelyanov NV. A randomized controlled trial of enteral versus parenteral feeding in patients with predicted severe acute pancreatitis shows a signi fi cant reduction in mortality and in infected pancreatic complications with total enteral nutrition. Dig Surg 2006;23:336-345.
21 Windsor AC, Kanwar S, Li AG, Barnes E, Guthrie JA, Spark JI, et al. Compared with parenteral nutrition, enteral feeding attenuates the acute phase response and improves disease severity in acute pancreatitis. Gut 1998;42:431-435.
22 Grant JP, Jame S, Grabowski V, Trexler KM. Total parenteral nutrition in pancreatic disease. Ann Surg 1984; 200:627-631.
BACKGROUND: Total parenteral nutrition (TPN) has been recognized as the mainstay of nutritional support in patients with severe hepatopancreatobiliary (HPB) diseases for decades.However, recent studies advocate the utilization of endoscopic nasojejunal feeding tube placement (ENFTP), rather than the conventional approach. This study was designed to compare the clinical value of ENFTP and TPN in patients with severe HPB diseases.
METHODS: Two groups of patients with severe HPB diseases were analyzed retrospectively. One group of 88 patients
ENFTP, and the other 96 received TPN. Routine blood levels, serum glucose and prealbumin, hepatic and renal function, serum lipid, and calcium were measured at baseline and after 1, 2, and 4 weeks of nutritional support.Also, complication rate, mortality, nutritional support time,mechanical ventilation time, mean length of time in intensive care unit, and duration of hospital stay were analyzed.
RESULTS: After 4 weeks of nutritional support, the degree of recovery of red blood cells, prealbumin, and blood glucose was greater in the ENFTP than in the TPN group (P<0.05).Furthermore, the ENFTP group showed a lower incidence of septicemia, multiple organ dysfunction syndrome, peripancreatic infection, biliary infection, and nosocomial infection, in addition to shorter nutritional support time and hospital stay (P<0.05).CONCLUSIONS: ENFTP is much more effective than TPN in assisting patients with severe HPB diseases to recover from anemia, low prealbumin level, and high serum glucose, as well as in decreasing the rates of various infections (pulmonary infection excluded), multiple organ dysfunction syndrome rate, nutrition support time, and length of hospital stay.Therefore, ENFTP is safer and more economical for clinical application.
Author Af fi liations: Department of Gastroenterology, First Af fi liated Hospital, Zhejiang University School of Medicine, Hangzhou 310003,China (Ji F, Zhao JL, Jin X, Jiao CH, Hu YY, Xu QW and Chen WX)
Feng Ji, MD, Department of Gastroenterology,First Af fi liated Hospital, Zhejiang University School of Medicine, Hangzhou 310003, China (Tel: 86-571-87236568; Fax: 86-571-87235577; Email:jifeng1126@sina.com)
© 2010, Hepatobiliary Pancreat Dis Int. All rights reserved.
nutritional support of nitrogen (0.15-0.20 g/kg per day) and calories(25-30 kcal/kg per day) equal to the ENFTP group. A 20%-30% concentration of 250-500 ml medium-chain or long-chain fat emulsion and 500-1000 ml amino acids were infused via the internal jugular vein or a peripheral vein. Additional liquid, glucose, various vitamins, and trace elements were added if necessary.
Received March 6, 2009
Accepted after revision November 3, 2009
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- Critical fl icker frequency for diagnosis and assessment of recovery from minimal hepatic encephalopathy in patients with cirrhosis
- Risk factors for early recurrence of smallhepatocellular carcinoma after curative resection
- Pathological changes at early stage of multiple organ injury in a rat model of severe acute pancreatitis
- Potential etiopathogenesis of seventh day syndrome following living donor liver transplantation: ischemia of the graft?
- Comparatively lower postoperative hepatolithiasis risk with hepaticocholedochostomy versus hepaticojejunostomy
- Effect of sodium salicylate on oxidative stress and insulin resistance induced by free fatty acids
