Inflammatory boweI diseases and hepatitis C virus infection
2010-06-29YanDongLiJianJiangLinandShuSenZheng
Yan-Dong Li, Jian-Jiang Lin and Shu-Sen Zheng
Hangzhou, China
Inflammatory boweI diseases and hepatitis C virus infection
Yan-Dong Li, Jian-Jiang Lin and Shu-Sen Zheng
Hangzhou, China
BACKGROUND:Data on the prevalence of hepatitis C in patients with inflammatory bowel diseases (IBD) are limited and conflicting. This study was to assess the prevalence of hepatitis C virus (HCV) infection in IBD patients and to define the clinical and immunologic profile of IBD associated with HCV infection.
METHODS:Ten patients (seven females and three males) with IBD and HCV infection were consecutively recruited in our department between June 2005 and May 2010. We analyzed the clinical and serologic description of all patients.
RESULTS:The mean age of the 10 patients was 41 years and the median disease duration was 7 years. With present and/or past HCV infection, the patients had clinical manifestations and were positive for endoscopic study or histological test. Compared with the HCV-negative IBD group, the HCV-positive IBD group have a higher positive rate of autoantibodies (antinuclear antibodies, antieutrophil cytoplasmic antibody, and anti-SSa/SSb). In the HCV-positive group, 8 patients were positive for p-antieutrophil cytoplasmic antibody, 4 positive for antinuclear antibodies, and 3 positive for anti-SSa/SSb. Four patients had an elevated level of transaminase (alanine transminase, and aspartate transminase).
CONCLUSIONS:HCV positive in IBD may induce autoantibodies (antinuclear antibodies, antieutrophil cytoplasmic antibody, anti-SSa/SSb) and damage of liver function. In managing IBD patients, physicians should be aware of screening of HCV and prescribe antiviral treatment.
(Hepatobiliary Pancreat Dis Int 2010; 9: 398-401)
inflammatory bowel disease; hepatitis C; ulcerative colitis; Crohn's disease
Introduction
Ulcerative colitis (UC) and Crohn's disease (CD) are chronic inflammatory conditions of the gastrointestinal tract collectively referred as inflammatory bowel diseases (IBD). Hepatitis C is a common infection worldwide. About 2.7 million people in the United States have been infected with chronic hepatitis C virus (HCV).[1]In China, the overall anti-HCV(+) rate is estimated to be 3.2%.[2]Although the prevalence has decreased in recent years, the risk of viral C hepatitis has long been considered to be increased in patients
with IBD.[3,4]Blood transfusion and surgery have been identified as the two main risk factors. However, recent epidemiologic studies have found that the prevalence of HCV in IBD patients is similar to or even lower than that in the general population.[5,6]This study aimed to detect the prevalence of anti-HCV in our inpatient clinic and to define the clinical and immunologic profile of 10 patients with IBD and HCV infection.
Methods
Patients
Ten patients (7 females and 3 males) with HCV infection were recruited from 610 patients with IBD who had been treated at our department between June 2005 and May 2010. IBD diagnosis was based on the IBD criteria proposed by the IBD Section of the British Society of Gastroenterology in 2004.[7]
Methods
HCV infection was confirmed by recombinant immunoblot assay and/or detection of serum HCV-RNA by polymerase reaction. Autoantibodies [antinuclearantibodies (ANA), antieutrophil cytoplasmic antibody (ANCA), anti-SSa/SSb] were detected in sera by indirect immunofluorescence. The levels of serum transaminases [alanine transminase (ALT), aspartate transminase (AST)] were determined by Jaffe kinetic assay. The level of aspartate transminase being 1.5-fold higher than the baseline level was considered abnormal.
Statistical analysis
Statistical analysis was performed by SPSS software version 11.0 (SPSS Inc., Chicago, IL., USA). The parameters were studied using the Chi-square test or Fisher's exact test. APvalue less than 0.05 was considered statistically significant.
Results
Of the 10 patients, 7 were female and 3 male, with mean age of 41 years (IQR: 24-51), and their median disease duration was 8 years (IQR: 5-14). Present and/or past HCV infection was found in 1.64% of the 610 patients recruited. All the patients had clinical manifestations and they were all positive for endoscopic examination or histological test. Eight IBD patients with p-ANCA and HCV infection were compared with 600 IBD patients with HCV infection. A large number of autoantibodies were noted in the HCV infection group. Most of the patients showed p-ANCA antibodies (80%) and a higher positive rate of ANA (40%). Four patients (40%) were positive for anti-SSa/SSb.
The clinical features of the 10 patients with IBD-HCV infection were compared with those of 600 patients with primary IBD (Table). The patients with IBD-HCV infection (mean age, 41 vs. 34 years;P<0.05) showed a higher prevalence of ANCA and ANA. 40% patients demonstrated p-ANCA antibodies alone or associated with ANA. Three patients were positive for anti-Ro/SSaand/or anti-La/SSb. Three patients showed an increased levels of AKP and GGT, and 4 had increased levels of ALT, AST. Abdominal ultrasound revealed hepatomegaly and hepatic steathosis in 3 patients, but none of them had hepatic failure. Of the 7 HCV-RNA positive patients receiving anti-virus treatment (interferon and ribavirin), 6 turned to be negative after treatment with HCVRNA, 4 showed normal liver function, and 1 failed to antivirus treatment. No adverse events were observed and gastrointestinal symptoms were improved. HCV treatment appeared to be effective in IBD patients.
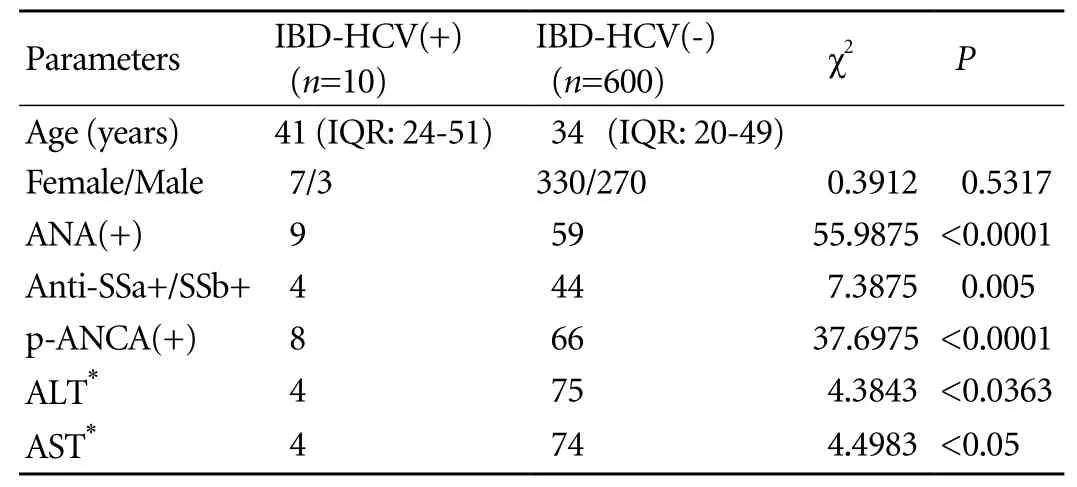
Table. Main serological and clinical features in 10 patients with IBD-HCV infection and in 600 patients with IBD
Discussion
Chronic HCV infection is a major and growing public health problem. Approximately 170 million of people worldwide are infected with HCV, but the prevalence varies greatly from 0.2% to 26% among countries.[8-10]In China, the overall anti-HCV(+) rate is stratified according to geographic origins (higher in northern China than in southern China); in recent years the prevalence of HCV has decreased dramatically.[11-13]The anti-HCV(+) frequency was 0.335% among 559 890 blood donors in 2007 in this country.[14]IBD patients who underwent surgery or received blood transfusion may have a higher risk for HCV infection.[2,3]In Italy Biancone et al[3]tested sera from 332 patients with CD and 374 controls for the presence of antibodies of HCV. The HCV prevalence rate (7.4%) in the CD patients was higher than that in the control group. In 2000 Longo et al[4]found that 117 IBD patients in France presented with antibodies to HCV with a seroprevalence rate of 5.98% (7/117), which was higher than the estimated prevalence of 0.86% for HCV infection in France. In Spain 0.79% of CD patients and 1.59% of UC patients were positive for anti-HCV.[5]
In the present study the rate of HCV infection was about 1.64% which was lower than that in Italy and France and higher than that in Spain. This percentage of infection was higher than the estimated rate of 0.335% in southern China in 2007. Patients with HCV infection were older on average in IBD patients, indicating old age may be related to the increased requirement for blood transfusion and surgery. Exposure to HCV was detected in IBD patients, and HCV positivity was related to a large number of autoantibodies. It is likely that HCV infection induces the autoimmune reaction and the production of autoantibodies.
Several autoantibodies associated with HCV infection have been recognized.[15,16]Although the non-organspecific autoantibodies have also been detected in patients with hepatitis C, their pathogenesis and clinicalsignificance are unclear. In our study HCV infection in IBD showed a higher positive rate for ANA, anti-SSa+/ SSb+ and p-ANCA. The other features of our study showed that HCV infection in IBD showed increased levels of ALT and AST. The relationship between a large number of autoantibodies and increased liver function damage has not been elucidated. Hepatitis viruses especially HCV which has been implicated most often in autoimmune hepatitis may induce abnormal liver function although the precise mechanism of virus inducing auto reactivity is debatable.
Current therapeutic agents for HCV include interferon and ribavirin. The effect of interferon on IBD is controversial. Several case reports suggest the potential benefit of interferon in treatment of IBD,[17,18]but others demonstrate new-onset IBD during the treatment or exacerbation of existing IBD with a predominance of UC.[19,20]In our study, HCV treatment was effective for IBD patients. Apart from disappearance of adverse events, gastrointestinal symptoms and liver test results were improved in the patients who received antivirus treatment. Non-pegylated interferon was used to treat the patients till the end of the treatment.
In conclusion, although the prevalence of HCV infection in our department is not common, it may induce such autoantibodies as ANA, ANCA, anti-SSa+/SSb+ as well as damage of liver function. Physicians managing IBD patients should be aware of screening of HCV and provide antiviral treatment to the patients.
Funding:None.
Ethical approval:Not needed.
Contributors:ZSS proposed the study. LYD wrote the first draft and analyzed the data. All authors contributed to the design and interpretation of the study and to further drafts. ZSS is the guarantor.
Competing interest:No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
1 No authors listed. Hepatitis C--global prevalence (update). Wkly Epidemiol Rec 1999;74:425-427.
2 Xia GL, Liu CB, Cao HL, Li S, Zhan MY, Sub CA, et al. Prevalence of hepatitis B and C virus infections in the general Chinese population: results from a nationwide cross-sectional seroepidemiologic study of hepatitis A, B, C, D, and E virus infections in China, 1992. Int Hepatol Commun 1996;5:62-73.
3 Biancone L, Pavia M, Del Vecchio Blanco G, D'Incà R, Castiglione F, De Nigris F, et al. Hepatitis B and C virus infection in Crohn's disease. Inflamm Bowel Dis 2001;7:287-294.
4 Longo F, Hebuterne X, Tran A, Staccini P, Hastier P, Schneider S, et al. Prevalence of hepatitis C in patients with chronic inflammatory bowel disease in the region of Nice and evaluation of risk factors. Gastroenterol Clin Biol 2000;24:77-81.
5 Loras C, Saro C, Gonzalez-Huix F, Mínguez M, Merino O, Gisbert JP, et al. Prevalence and factors related to hepatitis B and C in inflammatory bowel disease patients in Spain: a nationwide, multicenter study. Am J Gastroenterol 2009;104: 57-63.
6 Tolentino YF, Fogaca HS, Zaltman C, Ximenes LL, Coelho HS. Hepatitis B virus prevalence and transmission risk factors in inflammatory bowel disease patients at Clementino Fraga Filho university hospital. World J Gastroenterol 2008;14:3201-3206.
7 Carter MJ, Lobo AJ, Travis SP; IBD Section, British Society of Gastroenterology. Guidelines for the management of inflammatory bowel disease in adults. Gut 2004;53:V1-16.
8 Aymard JP, Botte C, Contal P, Janot C, Streiff F. Seroprevalence of hepatitis C antibodies among blood donors. Study of second generation ELISA and RIBA tests and surrogate markers. Pathol Biol (Paris) 1993;41:149-153.
9 Shakil AO, Conry-Cantilena C, Alter HJ, Hayashi P, Kleiner DE, Tedeschi V, et al. Volunteer blood donors with antibody to hepatitis C virus: clinical, biochemical, virologic, and histologic features. The Hepatitis C Study Group. Ann Intern Med 1995;123:330-337.
10 Panigrahi AK, Panda SK, Dixit RK, Rao KV, Acharya SK, Dasarathy S, et al. Magnitude of hepatitis C virus infection in India: prevalence in healthy blood donors, acute and chronic liver diseases. J Med Virol 1997;51:167-174.
11 Ding X, Gu H, Zhong ZH, Zilong X, Tran HT, Iwaki Y, et al. Molecular epidemiology of hepatitis viruses and genotypic distribution of hepatitis B and C viruses in Harbin, China. Jpn J Infect Dis 2003;56:19-22.
12 Zhao SM, Jiang TL, Gao FX, Lu L, Zheng HQ, Hu J, et al. Analysis of true voluntary blood donors with anti-HCV prevalence and implications for donor management in Chongqing, China. Transfus Med 2007;17:210-211.
13 Nainan OV, Lu L, Gao FX, Meeks E, Robertson BH, Margolis HS. Selective transmission of hepatitis C virus genotypes and quasispecies in humans and experimentally infected chimpanzees. J Gen Virol 2006;87:83-91.
14 Fu Y, Xia W, Wang Y, Tian L, Pybus OG, Lu L, et al. The seroprevalence of hepatitis C virus (HCV) among 559,890 first-time volunteer blood donors in China reflects regional heterogeneity in HCV prevalence and changes in blood donor recruitment models. Transfusion 2010 Apr 23; [Epub ahead of print].
15 Feld JJ, Dinh H, Arenovich T, Marcus VA, Wanless IR, Heathcote EJ. Autoimmune hepatitis: effect of symptoms and cirrhosis on natural history and outcome. Hepatology 2005;42: 53-62.
16 Lidar M, Lipschitz N, Langevitz P, Barzilai O, Ram M, Porat-Katz BS, et al. Infectious serologies and autoantibodies in Wegener's granulomatosis and other vasculitides: novel associations disclosed using the Rad BioPlex 2200. Ann N Y Acad Sci 2009;1173:649-657.
17 Musch E, Andus T, Malek M. Induction and maintenance of clinical remission by interferon-beta in patients with steroidrefractory active ulcerative colitis-an open long-term pilot trial. Aliment Pharmacol Ther 2002;16:1233-1239.
18 Musch E, Andus T, Kruis W, Raedler A, Spehlmann M,Schreiber S, et al. Interferon-beta-1a for the treatment of steroid-refractory ulcerative colitis: a randomized, doubleblind, placebo-controlled trial. Clin Gastroenterol Hepatol 2005;3:581-586.
19 Villa F, Rumi MG, Signorelli C, Saibeni S, Del Ninno E, Ferrero Bogetto S, et al. Onset of inflammatory bowel diseases during combined alpha-interferon and ribavirin therapy for chronic hepatitis C: report of two cases. Eur J Gastroenterol Hepatol 2005;17:1243-1245.
20 Morimoto K, Yamagami H, Hosomi S, Ohira M, Suekane T, Kamata N, et al. Development of pouchitis with combination therapy with peg-interferon alpha-2b and ribavirin for chronic hepatitis C in a patient with ulcerative colitis who underwent pouch surgery. Am J Gastroenterol 2009;104:1609-1610.
Accepted after revision June 28, 2010
When learning something, one should not be self-abased nor self-important.
— Gu Yanwu
February 15, 2010
Author Affiliations: Department of General Surgery, First Affiliated Hospital, Zhejiang University School of Medicine, Hangzhou 310003, China (Li YD, Lin JJ and Zheng SS)
Shu-Sen Zheng, MD, PhD, FACS, Department of General Surgery, First Affiliated Hospital, Zhejiang University School of Medicine, Hangzhou 310003, China (Tel: 86-571-87236601; Email: lee1952@163.com)
© 2010, Hepatobiliary Pancreat Dis Int. All rights reserved.
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- Hepatobiliary & Pancreatic Diseases International (HBPD INT)
- Efficacy of Shanvac-B recombinant DNA hepatitis B vaccine in heaIth care workers of Northern India
- Radiofrequency ablation, heat shock protein 70 and potential anti-tumor immunity in hepatic and pancreatic cancers: a minireview
- Outcome of hepatocellular carcinoma treated by liver transplantation: comparison of living donor and deceased donor transplantation
- Norcantharidin inhibits growth of human gallbladder carcinoma xenografted tumors in nude mice by inducing apoptosis and blocking the cell cycle in vivo
- Meetings and Courses
