儿童新型冠状病毒感染并发纵隔气肿八例影像学及临床特点研究
2025-01-01付强任作雷林志强龚剑峰王长征王婷胡雅兰谭举方
【摘要】 背景 儿童新型冠状病毒感染(COVID-19)影像学与成人有一定差异,主要表现为胸膜下磨玻璃影、斑片状高密度影、实变影等,合并纵隔气肿者并不多见。大量气肿形成可严重影响呼吸及循环功能,导致明显喘憋、低氧血症,需积极处理。目的 分析并总结儿童COVID-19并发纵隔气肿的影像学及临床特征。方法 回顾分析2022-12-01—2023-01-30在长江大学附属荆州医院儿科住院的8例COVID-19并发纵隔气肿的患儿年龄、性别、影像学、临床特点及诊疗情况。结果 8例患儿年龄3岁7个月~12岁,男女比3∶5,高分辨率CT(HRCT)均显示双肺感染合并纵隔气肿。气肿多同时累及颈部及胸壁。肺部表现多种多样:胸膜下磨玻璃影、实变、树芽征、支气管血管束增粗、支气管壁增厚及网格征等,未见大片实变及“白肺”。1例患儿合并少量胸腔积液。临床表现除有发热、咳嗽外,均有明显气促,肺部听诊干湿啰音可不显著。4例合并肺炎支原体感染、1例合并卡他布兰汉菌感染。合并肺炎支原体感染者应用阿奇霉素,合并卡他布兰汉菌感染者给予头孢噻肟治疗。8例患儿均给予氧疗。1例患儿白细胞总数及超敏C反应蛋白明显升高,明显气急,低氧血症,常规治疗无好转,给予有创呼吸机治疗3 d后好转撤机。5例应用静脉丙种球蛋白(IVIG),3例使用糖皮质激素。1周后复查胸部CT,纵隔气肿均完全吸收,肺部病灶明显好转。结论 COVID-19并发纵隔气肿者多为学龄前期或学龄期儿童,婴幼儿少见。可同时合并颈部及胸壁积气。肺部病变可累及间质或实质、双肺均受累,表现形式多样。起病多有明显气急,积极氧疗。白细胞计数明显升高,同时超敏C反应蛋白明显升高者,要密切关注呼吸情况,积极使用IVIG,适时适量应用糖皮质激素,必要时采用呼吸机人工辅助通气。
【关键词】 新型冠状病毒感染;纵隔气肿;临床特征;体层摄影术,螺旋计算机;儿童
【中图分类号】 R 563.12 【文献标识码】 A DOI:10.12114/j.issn.1007-9572.2023.0733
Imaging and Clinical Characteristics of 8 Cases of COVID-19 Complicated with Pneumomediastinum in Children
FU Qiang1,REN Zuolei2,LIN Zhiqiang3,GONG Jianfeng4,WANG Changzheng5,WANG Ting1,HU Yalan1,TAN Jufang1*
1.Gynaecology,Jingzhou Hospital Affiliated to Yangtze University,Jingzhou 434020,China
2.Case Statistics Section,Jingzhou Hospital Affiliated to Yangtze University,Jingzhou 434020,China
3.Public Health Section,Jingzhou Hospital Affiliated to Yangtze University,Jingzhou 434020,China
4.Radiology,Jingzhou Hospital Affiliated to Yangtze University,Jingzhou 434020,China
5.Laboratory,Jingzhou Hospital Affiliated to Yangtze University,Jingzhou 434020,China
*Corresponding author:TAN Jufang,Associate chief physician/Master supervisor;E-mail:tanjufang@yangtzeu.edu.cn
【Abstract】 Background The imaging of COVID-19(COVID-19) in children is different from that of adults,mainly manifested as subpleural ground glass shadows,patchy high-density shadow,and solid shadow,and rarely complicated with pneumomediastinum. The formation of a large number of emphysema can seriously affect the respiratory and circulatory function,resulting in obvious wheezing and hypoxemia,which need to be actively treated. Objective To analyze and summarize the imaging and clinical characteristics of COVID-19 with pneumomediastinum in children. Methods A retrospective analysis was conducted on 8 pediatric patients with COVID-19 complicated with pneumomediastinum admitted to the Department of Pediatrics at Jingzhou Hospital Affiliated with Yangtze University from December 1,2022 to January 30,2023,including age,gender,imaging,clinical characteristics,and treatment. Results 8 children were 3.5 years to 12 years,with a female ratio of 3∶5. High Resolution CT Scan in all children showed double lung infection combined with pneumomediastinum,and multiple emphysema involved the neck and chest wall. The pulmonary manifestations were various:subpleural ground glass shadow,consolidation,tree bud sign,vascular bronchial bundle thickening and bronchial wall thickening,grid sign,etc.,no large consolidation and \"white lung\" found. One case was observed to have a small amount of pleural effusion. In addition to fever and cough,the clinical manifestations were obvious shortness of breath,pulmonary auscultation,but dry or moist rales were not significant. Four children with mycoplasma infection were treated with azithromycin,and one with B. catarrhalis. was treated with azithromycin. All given oxygen therapy. A patient was treated with an invasive ventilator because traditional treatment was unable to alleviate her dyspnea and hypoxemia. The patient's leucocytes and hypersensitive CRP were significantly increased. After 3 days,the symptoms improved and the machine was successfully withdrawn. 5 cases were treated with intravenous immunoglobulin(IVIG),and 3 cases were treated with glucocorticoids. a week after the review of chest CT,pneumomethinum were completely absorbed,and lung lesions significantly improved. Conclusion Children with pneumomediastinum complicated by COVID-19 were mostly pre-school or school-age children,rare in infants. Pneumomediastinum can coexist with gas accumulation in the neck and chest wall. In addition,pulmonary lesions could involve the stroma or parenchyma,and both lungs were affected,with various manifestations. At the onset of the disease,there were obvious shortness of breath,active oxygen therapy was recommended. When the white blood cell count and hypersensitivity CRP significantly increase,close attention should be paid to respiratory conditions. IVIG and glucocorticoids may have positive effects,and if necessary,a mechanical ventilation should also be used.
【Key words】 COVID-19;Mediastinal emphysema;Clinical characteristics;Tomography,spiral computed;Child
儿童新型冠状病毒感染(COVID-19)影像学与成人有一定差异。成人患者胸部CT肺内早期表现为磨玻璃或斑片影,双肺多发、胸膜下分布为主,可进展为实变,部分严重者可呈“白肺”,肺外可有纵隔气肿、气胸、胸腔积液、心包积液等。大部分儿童患者肺内改变较成人轻,表现为单侧或双侧肺炎、斑片状或磨玻璃影。重者可有双肺多发肺叶病灶[1],较少发展为“白肺”。儿童COVID-19合并纵隔气肿者报道不多,大量气肿形成可严重影响呼吸及循环功能,导致明显喘憋、低氧血症,需积极处理[2]。本文对8例COVID-19并发纵隔气肿患儿影像学及临床特点进行分析,以提高儿科医护人员对该疾病的认识。
1 资料与方法
1.1 病例资料
选择2022-12-01—2023-01-31在长江大学附属荆州医院儿科住院的8例COVID-19并发纵隔气肿患儿为研究对象。纳入标准:(1)新型冠状病毒核酸检测阳性;(2)影像学检查及临床资料完整;(3)排除其他肺炎。本研究经本院伦理学委员会审批(批准号:20230155),患儿家属均知情同意并签署知情同意书。
1.2 方法
1.2.1 诊断标准:COVID-19诊断依据国家卫生健康委员会发布的《新型冠状病毒感染肺炎诊疗方案(第九版》。患儿入院后采集口咽拭子标本,检测有无COVID-19感染。检测方法:将口咽拭子标本混匀后取200 uL保存液采用磁珠法处理提取新型冠状病毒核酸,应用PCR-荧光探针法在ABI-7500实时荧光定量扩增仪上检测。扩增曲线为标准“S”型曲线且Ct值lt;38判读为阳性。扩增试剂购自广州达安基因股份有限公司(国械注准20203400063)。
1.2.2 胸部CT检查:在发病初、治疗一周症状体征明显缓解后行胸部CT检查,观察支气管、肺及纵隔情况。胸部CT检查采用联影uCT530CT,扫描时取头先进、仰卧体位,均匀自由呼吸。扫描范围从肺尖到肺底。扫描参数:管电压100 kV,管电流自动调节,扫描层厚5.0 mm,层间距5.0 mm,扫描结束后以1 mm层厚、0.8 mm层间距重建,采用肺窗和纵隔窗观察图像,肺窗观察窗位为-500 Hu,窗宽为-1 200 Hu;纵隔窗观察窗位为40 Hu,窗宽为400 Hu。
1.2.3 肺炎支原体抗体滴度检测:患儿入院后采集静脉血2 mL(EDTA抗凝),检测肺炎支原体(MP)-IgG抗体滴度,观察有无肺炎支原体感染。MP-IgG抗体滴度采用冷凝集试验进行检测,操作方法:将待检血清做倍比稀释至1∶512,同时设置阴性对照,加入5%洗涤O型红细胞,于2~8 ℃放置2 h后观察结果。MP-IgM检测:取待检血浆10 μL加入样品孔中,加2~3滴样品稀释液,检测开始后5~10 min内若出现检测线和质控线,可判为阳性,若仅出现质控线判为阴性,10 min以上判读结果无效。检测试剂购自珠海丽珠试剂有限公司(国械注准:20183400122)。
1.2.4 痰培养:入院后在使用抗生素之前留取患儿痰液标本,留取前清水漱口2~3次,及时送检,以明确有无细菌、真菌等感染。培养方法:取适量痰液,加等量消化液消化20 min,接种哥伦比亚血琼脂平板、伊红美蓝平板和巧克力平板,待细菌生长后,取可疑致病菌做纯培养,用布鲁克质谱仪鉴定细菌,同时做药物敏感试验。
2 结果
2.1 临床资料
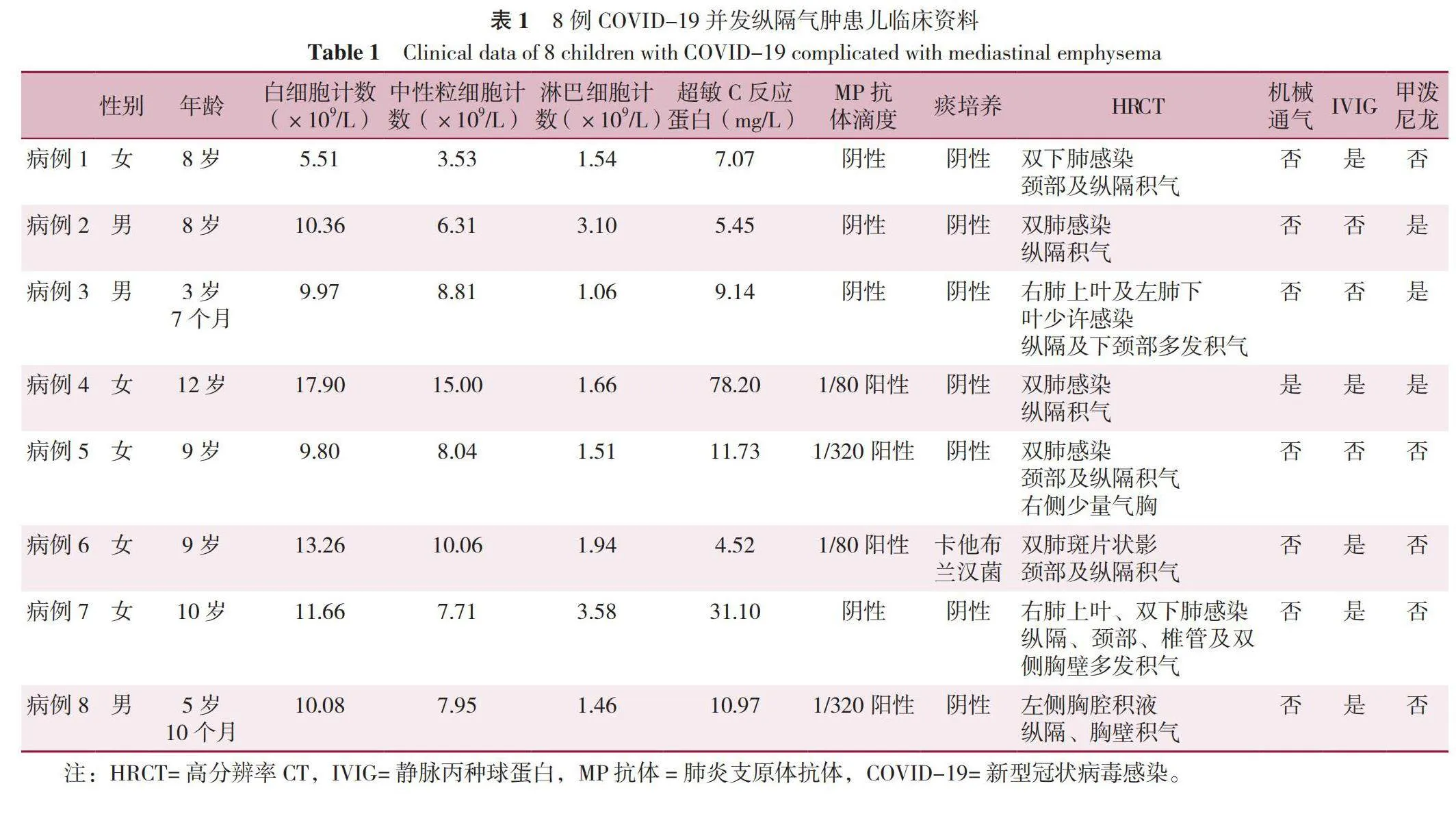
8例COVID-19并发纵隔气肿患儿年龄3岁7个月~12岁,男女比3∶5;临床表现除有发热、咳嗽外,均有明显气促,肺部听诊干湿啰音不显著;4例合并支原体感染、1例合并卡他布兰汉菌感染;均给予氧疗、雾化吸入治疗,合并支原体感染者应用阿奇霉素、合并卡他布兰汉菌感染者给予头孢噻肟治疗。1例患儿白细胞总数及超敏C反应蛋白明显升高,明显气急,低氧血症,常规治疗无好转,给予有创呼吸机人工辅助通气治疗3 d后好转撤机,5例应用静脉丙种球蛋白(IVIG),1周后复查胸部CT,纵隔气肿均完全吸收,肺部病灶明显好转,见表1。
2.2 胸部影像学
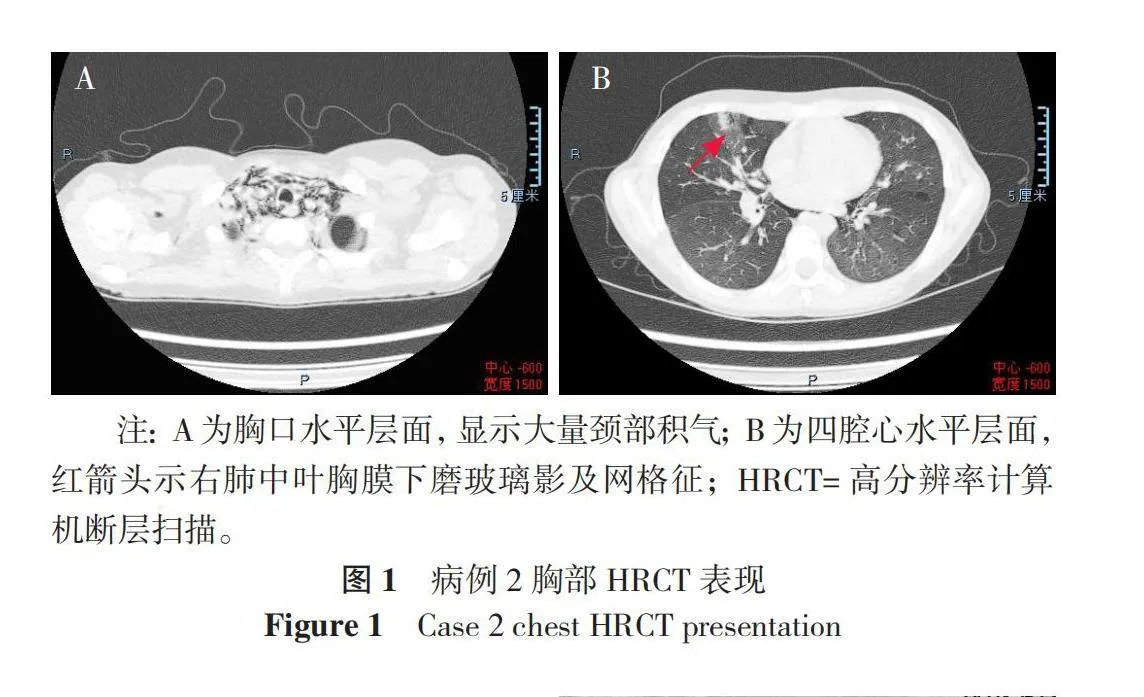
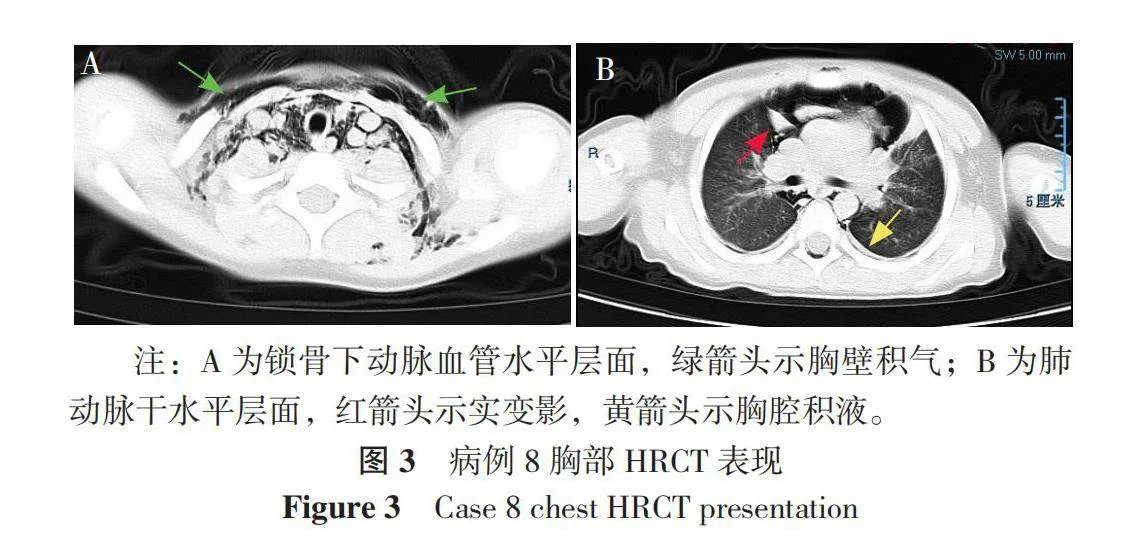
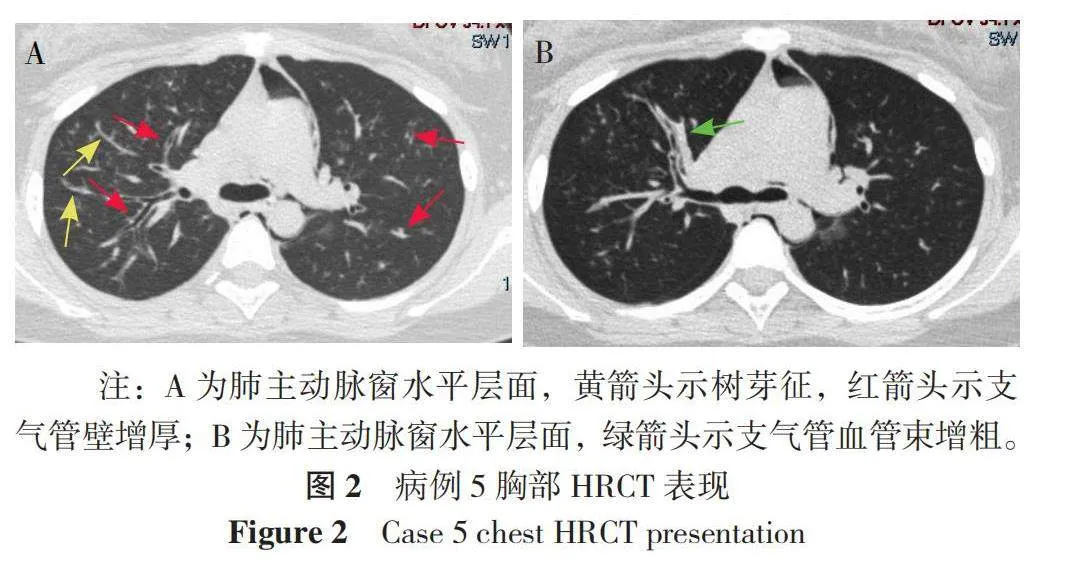
8例患儿高分辨率计算机断层扫描(HRCT)均显示双肺感染合并纵隔气肿,气肿多同时累及颈部及胸壁。肺部表现多种多样:胸膜下磨玻璃影、实变、树芽征、支气管血管束增粗、支气管壁增厚、网格征等,未见大片实变及“白肺”等表现,1例合并胸腔积液。病例2表现为颈部大量积气、双肺感染、胸膜下磨玻璃影及网格征,见图1。病例5表现为双肺感染、树芽征、支气管壁增厚及支气管血管束增粗,见图2。病例8表现为胸壁积气、双肺感染、实变及少量胸腔积液,见图3。
3 讨论
纵隔气肿是指纵隔结缔组织内有气体积聚,可来源于小气道或肺泡,也可来源于上呼吸道、肺内气管或消化道[3];来源于小气道或肺泡者,大多是因为肺部感染,损伤肺泡Ⅱ型上皮细胞,表面张力增加,肺泡塌陷,邻近肺泡过度通气,导致肺泡破裂,气体漏出,通过间质及血管鞘,到达纵隔[4]。少数纵隔气肿是因为支气管异物,导致活瓣形成,气道远端积气,压力增加导致肺泡破裂[5]。极少数青少年自发性气胸病因及发病机制不明[6]。王玉琪等[7]认为儿童纵隔气肿的病因构成由高到低分别为呼吸道感染、支气管哮喘、新生儿呼吸窘迫综合征、支气管异物等,认为儿童纵隔气肿发病率并不低。
2019年以来COVID-19在全球范围内流行,成人COVID-19合并纵隔气肿者并不少见,国内外均有报道[8-10]。儿童COVID-19并发纵隔气肿报道较少,目前仅有一些个案报道[11-13],文献中报道的3例患儿病情凶险,均入住重症监护室治疗,1例为3个月龄小婴儿,肺部CT显示双肺实变,纵隔及颈部明显积气,气管插管困难,最终使用直接喉镜进行插管,并行胸膜及纵隔引流及呼吸机治疗;另1例为9岁女童,髓母细胞瘤术后发生呼吸窘迫综合征,确诊为COVID-19,病情迅速恶化,进入重症监护室治疗;第3例为11岁女孩,纵隔气肿、肺气肿、皮下气肿,心肺衰竭,行人工模肺治疗,该患者本身患有腺苷脱氨酶2缺乏症。本中心从2022年12月—2023年1月共收治441例COVID-19患儿住院治疗,并发纵隔气肿者8例,占比1.8%。由此可见,纵隔气肿在COVID-19中发生率并不低,可能还有少部分少量纵隔气肿因为普通DR平片显示不明显而漏诊。与文献报道不同的是,本研究中8例患儿均为学龄前期及学龄期儿童,未见小婴儿组COVID-19合并纵隔气肿者。同时,仅1例需要入住重症监护室治疗,可能与患儿不伴有导致免疫力低下的基础疾病有关。文献中1例为3月龄小婴儿,另2例患儿患肿瘤性疾病及免疫缺陷症,可能是导致病情更为凶险的原因之一[11-13]。
胸部CT对纵隔气肿有很好的分辨率,对于极少量纵隔积气、颈部及胸壁积气均可明显提示,对临床医生判断病情有较大帮助,同时,对肺内病变程度及性质也有较好评估[14]。8例患儿HRCT均显示双肺感染合并纵隔气肿,气肿多同时累及颈部及胸壁,说明肺泡壁破裂或肺间质“漏气”严重,但肺内病灶并不一定表现为大片实变或“白肺”,可能的原因是新型冠状病毒毒力强、侵蚀力高,极大破坏了肺泡表面Ⅱ型细胞,导致气体漏出,穿过肺间质及血管鞘,到达纵隔或皮下[15],病例4因为大量积气、呼吸窘迫、低氧血症,行有创呼吸机人工辅助通气治疗,提示对于有明显气急,但肺部体征不明显者,应尽快行胸部影像学检查以明确有无纵隔气肿形成。8例患儿肺部表现多种多样:胸膜下磨玻璃影、实变、树芽征、支气管血管束增粗、支气管壁增厚、网格征等,未见大片实变及“白肺”等表现,1例合并胸腔积液。磨玻璃影是COVID-19最常见的影像学改变。病毒首先侵袭肺间质,包括小叶间隔、小叶内间隔、胸膜下等,炎性渗出,CT下显示密度增高影,但基底部血管影仍可见,表现为磨玻璃影,渗出进一步增加,小叶内间隔及小叶间隔进一步增厚,可表现为“网格征”或“铺路石征”,当支气管血管束渗出增加时,即表现为支气管血管束增粗。渗出进一步增多,肺泡纤维蛋白积聚,掩盖基底部血管束,可发展为实变影。
吴爱民等[16]报道了45例肺炎合并纵隔气肿,其中明确病毒病原者占多数,如呼吸道合胞病毒、腺病毒及流感病毒等,支原体其次,细菌占少数,部分为混合感染。8例COVID-19合并纵隔气肿患儿中,4例合并支原体感染、1例合并卡他布兰汉菌感染。据报道,成人COVID-19合并细菌感染者以革兰阴性杆菌为主,如肺炎克雷白杆菌、鲍曼不动杆菌、大肠埃希菌等,也见金黄色葡萄球菌、肠球菌等[17]。本研究显示儿童合并支原体感染较多见。
8例患儿中仅1例显示少量胸腔积液。感染性胸腔积液多见于结核感染、肺炎支原体感染、腺病毒感染等,肺炎链球菌肺炎鲜见胸腔积液。COVID-19致胸腔积液者并不多见,多为少量积液,且可较快恢复[18]。病例8有左侧胸腔积液,该患儿实验室检验提示有较高滴度肺炎支原体抗体存在(MP抗体滴度≥1∶160),同时存在呼吸道症状及影像学表现,不能排除同时罹患肺炎支原体感染可能,当然,如果病程中双份血清MP抗体滴度上升4倍以上,即可明确诊断同时合并肺炎支原体感染,遗憾的是,未进行动态观察MP抗体滴度变化,如果确实存在的话,其胸腔积液的成因就不一定单纯是COVID-19造成的。
8例患儿均给予氧疗、雾化吸入、肺炎支原体抗体滴度≥1∶160者应用阿奇霉素、合并卡他布兰汉菌感染者给予头孢噻肟治疗;应用IVIG的5例患儿病情进展,有明显气促、氧饱和度≤93%或不稳定、精神及食欲不佳,同时合并心肌损害等。IVIG使用方法:400 mg·kg-1·d-1,连用5 d或未达5 d但临床症状明显好转即停用。IVIG可特异性结合抗原,激活补体,并有免疫黏附、中和及溶解病毒作用,有报道应用于重型COVID-19,可减少病毒对肺泡的损伤,显著提升临床治疗效果[19]。3例患儿症状重,影像学进展较快,应用静脉滴注甲泼尼龙治疗,2 mg·kg-1·d-1,连用3~5 d。《儿童2019冠状病毒病(COVID-19)诊疗指南(第二版)》[20]
对IVIG及糖皮质激素的应用指征及用法进行了推荐。刘敏等[21]在一项糖皮质激素治疗重症COVID-19患者Meta分析研究中认为糖皮质激素治疗重症COVID-19有效,且未明显增加不良反应。所有患儿1周后复查胸部CT,纵隔气肿均完全吸收,肺部病灶明显好转。病例4患儿存在明显气急、低氧血症,常规治疗无好转,给予有创呼吸机机械通气治疗3 d后好转撤机。与另7例患儿不同的是,病例4患儿外周血白细胞计数明显升高、超敏C反应蛋白明显升高,结合患儿临床表现,考虑患儿合并脓毒症。有研究报道,COVID-19导致脓毒症可加剧急性肺损伤,白细胞总数及超敏C反应蛋白均是诊断脓毒症的重要实验室指标[22]。同时,患儿淋巴细胞比率降低,提示机体免疫功能受损,因为新型冠状病毒具有嗜淋巴细胞性,可通过直接损伤、诱导凋亡及免疫损伤等多方面导致淋巴细胞减少,而淋巴细胞是机体产生非特异性及特异性免疫的关键细胞。有研究认为,重症COVID-19患者淋巴细胞计数降低,可作为预测预后风险的因素之一[23]。
儿童COVID-19并发纵隔气肿者可同时合并颈部及胸壁积气,肺部病变可累及间质或实质、双肺均受累,表现形式多样。起病多有明显气急,积极氧疗,防治合并细菌及支原体感染、白细胞计数明显升高,淋巴细胞比率明显降低,同时超敏C反应蛋白明显升高者,要密切关注呼吸情况,积极使用IVIG,适时适量应用糖皮质激素及IVIG,必要时采用呼吸机人工辅助通气。但本研究病例数较少,COVID-19发生纵隔气肿的高危因素为何,还需要更大样本量进一步观察。
作者贡献:付强、谭举方提出研究思路、写作、评论与编辑、经费筹措、监督、最终版本修订,对论文整体负责;任作雷负责数据采集;林志强负责流行病学调查;龚剑峰负责影像学质控;王长征负责检验数据监督;王婷、胡雅兰负责审查、编辑、验证。
本文无利益冲突。
参考文献
刘洁,罗万军,邓志宏,等. 91例儿童新型冠状病毒肺炎确诊病例临床及流行病学特征[J]. 中华医院感染学杂志,2020,30(11):1625-1629. DOI:10. 11816 /cn.ni.2020-200550.
KHAIRE N,DESHMUKH S,AGARWAL E,et al. “Pneumomediastinum:a marker of severity in Covid-19 disease”[J]. Heliyon,2023,9(1):e12981. DOI:10.1016/j.heliyon.2023.e12981.
FRÜH J,ABBAS J,CHEUFOU D,et al. Spontaneous pneumomediastinum(Hamman's syndrome) with pneumorrhachis as a rare cause of acute chest pain in a young patient with acute asthma exacerbation[J]. Pneumologie,2023,77(7):430-434. DOI:10.1055/a-2007-9778.
VALENTE BARBAS C S,MARINI ISOLA A,BALDISSEROTTO S. Worsening COVID-19 acute respiratory distress syndrome:pneumomediastinum?[J]. Crit Care Med,2023,51(1):145-148. DOI:10.1097/CCM.0000000000005733.
WEN X,SHI J,HUANG A P,et al. Clinical analysis of severe cases of bronchial foreign body with mediastinal and subcutaneous emphysema in children[J]. Lin Chuang Er Bi Yan Hou Tou Jing Wai Ke Za Zhi,2021,35(3):267-269. DOI:10.13201/j.issn.2096-7993.2021.03.017.
GUNAWARDENE A. Mackler's triad in spontaneous pneumomediastinum[J]. ANZ J Surg,2023,93(1/2):437. DOI:10.1111/ans.18147.
王玉琪,周云连,陈志敏. 120例纵隔气肿患儿临床特征和影响因素分析[J]. 中国妇幼保健,2021,36(6):1354-1356. DOI:10.19829/j.zgfybj.issn.1001-4411.2021.06.044.
丁义,黄增发,赵胜超,等. 新型冠状病毒肺炎(COVID-19)临床及影像学特征分析[J]. 放射学实践,2020,35(3):281-285. DOI:10.13609/j.cnki.1000-0313.2020.03.008.
AGHAJANZADEH M,ALAVI FOUMANI A,TANGESTANINEJAD A,et al. Spontaneous tension pneumomediastinum with pneumothorax and subcutaneous emphysema as a complication of COVID-19 disease[J]. Clin Case Rep,2023,11(7):e7570. DOI:10.1002/ccr3.7570.
ALNEYADI M,JAIGANESH T,CHATHA H. Spontaneous Pneumomediastinum in an asthmatic pediatric patient,triggered by SARS-COVID-19 infection[J]. Vis J Emerg Med,2023,32:101734. DOI:10.1016/j.visj.2023.101734.
SINCLAIR V,SHARIEFF I,GASKELL B,et al. COVID-19 presenting with spontaneous massive pneumomediastinum in a three-month-old child[J]. Anaesth Rep,2021,9(2):e12126. DOI:10.1002/anr3.12126.
CARROLL A G,QUINN N,BYRNE C,et al. Pneumomediastinum in a child with severe COVID-19[J]. BJR Case Rep,2020,7(1):20200062. DOI:10.1259/bjrcr.20200062.
MOSCATELLI A,PEZZATO S,BURATTI S,et al. COVID-19 pneumomediastinum:possible role of transesophageal echo in bedside percutaneous bicaval double-lumen ECMO cannulation in children. A case report[J]. Front Pediatr,2021,9:740853. DOI:10.3389/fped.2021.740853.
MACCARRONE V,LIOU C,D'SOUZA B,et al. The Macklin effect closely correlates with pneumomediastinum in acutely ill intubated patients with COVID-19 infection[J]. Clin Imaging,2023,97:50-54. DOI:10.1016/j.clinimag.2023.03.003.
SELVARAJ V,DAPAAH-AFRIYIE K. Iatrogenic pneumothorax and pneumomediastinum in a patient with COVID-19[J]. R I Med J (2013),2020,103(10):32-33.
吴爱民,陈强,李岚,等. 儿童肺炎合并纵隔气肿45例临床分析[J]. 江西医药,2020,55(8):1098-1099,1129. DOI:10.3969/j.issn.1006-2238.2020.08.041.
刘兰,黄红丽,加明明,等. 新型冠状病毒肺炎患者合并感染的临床特征[J]. 武汉大学学报(医学版),2023,44(6):667-672. DOI:10.14188/j.1671-8852.2022.0756.
江凯,龚红霞,许磊磊,等. 新型冠状病毒肺炎胸部CT表现特征[J]. 医学影像学杂志,2021,31(1):129-132.
庞增,陈勇军,陈木春,等. 大剂量丙种球蛋白冲击疗法治疗新型冠状病毒重症肺炎2例[J]. 广东医科大学学报,2022,40(1):116-117.
陈志敏,傅君芬,舒强,等. 儿童2019冠状病毒病(COVID-19)诊疗指南(第二版)[J]. 浙江大学学报(医学版),2020,49(2):139-146. DOI:10.3785/j.issn.1008-9292.2020.02.01.
刘敏,杨程,冯春露,等. 糖皮质激素治疗重症新型冠状病毒肺炎患者有效性和安全性的Meta分析[J]. 中国循证医学杂志,2022,22(4):387-393.
GHAFOURI E,BIGDELI M,KHALAFIYAN A,et al. Unmasking the complex roles of hypocalcemia in cancer,COVID-19,and sepsis:engineered nanodelivery and diagnosis[J]. Environ Res,2023,238(Pt 1):116979. DOI:10.1016/j.envres.2023.116979.
唐新宁,董国伟,钟英成,等. 淋巴细胞亚群及炎症因子对新型冠状病毒肺炎患者的临床价值研究[J]. 标记免疫分析与临床,2023,30(1):25-29. DOI:10.11748/bjmy.issn.1006-1703.2023.01.005.
(收稿日期:2023-11-15;修回日期:2024-02-11)
(本文编辑:崔莎)