首发围绝经期抑郁症病人血清雌激素水平动态变化及其与认知功能的相关性
2024-07-10苏晓云贺继平张晓宇张丽娜杨芯雨
苏晓云 贺继平 张晓宇 张丽娜 杨芯雨
基金项目 2022年度吕梁市科学计划项目,编号:2022SHFZ25
作者简介 苏晓云,副教授,硕士,E?mail:694137579@qq.com
引用信息 苏晓云,贺继平,张晓宇,等.首发围绝经期抑郁症病人血清雌激素水平动态变化及其与认知功能的相关性[J].护理研究,2024,38(13):2302?2310.
Dynamic changes in serum oestrogen levels and their association with cognitive function in patients with first perimenopausal depression
SU Xiaoyun, HE Jiping, ZHANG Xiaoyu, ZHANG Li'na, YANG Xinyu
Fenyang College of Shanxi Medical University, Shanxi 032200 China
Corresponding Author SU Xiaoyun, E?mail:694137579@qq.com
Abstract Objective:To investigate the dynamic changes of serum oestrogen levels in patients with first?episode perimenopausal depression (PMD) and their correlation with cognitive function.Methods:127 patients with first?episode PMD who visited Shanxi Fenyang Hospital from December 2021 to December 2022 were selected to be included in the PMD group,and 200 perimenopausal women who underwent a physical examination at our hospital during the same period were selected to be included in the control group.General information was collected and levels of sex hormones (oestrone (E1),oestradiol(E2),serum prolactin (PRL)),follicle?stimulating hormone (FSH),and luteinising hormone (LH),and norepinephrine (NE),dopamine (DA),brain?derived neurotrophic factor (BDNF),and 5?hydroxytryptophan (5?HT) were measured in both groups at the time of visit;sex hormone and neurotransmitter levels were measured at different time points (at the time of consultation,3 months,6 months and 12 months after consultation) and cognitive function was assessed using the Montreal Cognitive Assessment Scale(MoCA) in the PMD group;sex hormone and neurotransmitter levels were analysed in relation to cognitive function using pearson's correlation;and risk factors affecting PMD were analysed using either unifactorial or multifactorial logistic regression equations;patients were divided into a cognitively impaired group (n=94) and a cognitively normal group (n=33) based on their MoCA scores at 12 months after the consultation,and clinical data and serological indices were compared between the two groups; the risk factors analysed using multifactorial logistic regression modelling.Results:The levels of E1,E2,NE,DA,BDNF,and 5?HT in the PMD group were significantly lower than those in the control group(P<0.05);and the levels of PRL,FSH,and LH in the women in the PMD group were significantly higher than those in the control group(P<0.05).With the increase of time,the levels of E1,E2,NE,DA,BDNF,and 5?HT in PMD patients showed a trend of gradual decrease,and there was a significant difference in the comparison between time points (P<0.05);with the increase of time, the levels of PRL,FSH,and LH in patients in the PMD group showed a trend of gradual increase,and there was a significant difference in the comparison between time points (P<0.05).After gradual exclusion of confounders with covariance,there was still an independent correlation between hormone indicators and the risk of cognitive impairment in patients with PMD (all P<0.001).Conclusion:Different levels of sex hormones and neurotransmitter factors all affect the occurrence of PMD,and there is a certain correlation between the level of cognitive functioning and sex hormones and neurotransmitter factors of perimenopausal women. Sex hormone dynamic level monitoring can be carried out on perimenopausal women in order to intervene in PMD at an earlier stage.
Keywords perimenopausal depression, PMD;estrogen;cognitive function;influencing factors;investigation and research
摘要 目的:探究首发围绝经期抑郁症病人血清雌激素水平动态变化及其与认知功能的相关性。方法:选取2021年12月—2022年12月于山西省汾阳医院就诊的首发围绝经期抑郁症病人127例纳入围绝经期抑郁症组,选取同期于我院进行体检的200名围绝经期妇女纳入对照组。收集两组女性的一般资料,并于就诊时和就诊后3个月、6个月及12个月检测两组性激素[雌酮(E1)、雌二醇(E2)、血清催乳素(PRL)、卵泡刺激素(FSH)和黄体生成素(LH)]、神经递质因子[去甲肾上腺素(NE)、多巴胺(DA)、脑源性神经营养因子(BDNF)和5?羟色胺(5?HT)]水平;并使用蒙特利尔认知评估量表(MoCA)评估病人的认知功能,根据病人就诊后12个月认知功能评分将病人分为认知障碍组(n=94)和认知正常组(n=33),比较两组病人临床资料与血清学指标,并使用多因素Logistic回归模型分析认知功能的影响因素。结果:围绝经期抑郁症组妇女E1、E2、NE、DA、BDNF、5?HT水平低于对照组(P<0.05),PRL、FSH、LH水平高于对照组(P<0.05)。随时间进展,围绝经期抑郁症病人E1、E2、NE、DA、BDNF、5?HT水平呈现逐渐降低趋势,且各时间点间比较差异有统计学意义(P<0.05);随时间进展,围绝经期抑郁症组病人PRL、FSH、LH水平呈现逐渐上升趋势,且各时间点间比较差异有统计学意义(P<0.05)。逐步排除混杂因素后,激素指标与围绝经期抑郁症病人认知障碍风险仍有相关性(P<0.001)。结论:不同性激素及神经递质因子水平会影响围绝经期抑郁症的发生,且围绝经期妇女认知功能与性激素、神经递质因子水平有一定的相关性,建议对围绝经期妇女进行性激素动态水平监测,以对围绝经期抑郁症进行早期干预。
关键词 围绝经期抑郁症;雌激素;认知功能;影响因素;调查研究
doi:10.12102/j.issn.1009-6493.2024.13.008
当女性处于围绝经期时,卵巢功能逐年衰减,导致女性雌激素分泌减少,严重者会造成女性器官或组织发生退行性病变,最终导致围绝经期综合征(perimenopausal syndrome,PMS)[1?2]。围绝经期抑郁症(perimenopausal depression,PMD)是PMS常见的心理症状之一,通常指在女性卵巢功能发生衰退至女性绝经后1年内,病人出现对事物毫无兴趣、情绪抑郁及不思饮食,并持续性存在[3?4]。围绝经期抑郁症发病机制涉及多种系统,包括内分泌、神经递质等[5],但由于其发病因素复杂,目前围绝经期抑郁症关键发病机制尚未明确。有研究表明,雌激素水平异常可导致女性罹患围绝经期抑郁症风险增加[6]。雌酮(estrone,E1)、雌二醇(estradiol,E2)是女性机体雌激素的重要组成,同时雌激素分泌受到卵泡刺激素(follicular stimulating hormone,FSH)和黄体生成素(luteinzing hormone,LH)的影响[7?9]。研究表明,抑郁会损害病人的认知功能,当病人存在认知障碍时,不仅会造成病人社会功能障碍,还会增加抑郁症反复发作风险,严重威胁病人生理与心理健康[10]。目前,雌激素代替治疗已广泛应用于围绝经期抑郁症临床治疗过程中,取得了较好的临床治疗效果[11],但有关雌激素在围绝经期的动态水平与围绝经期抑郁症病人认知水平相关性的研究鲜见报道。本研究通过分析首发围绝经期抑郁症病人雌激素动态水平与认知功能的关系,以期为围绝经期抑郁症临床治疗及后期认知修复提供依据。
1 对象与方法
1.1 研究对象
选取2021年12月—2022年12月于山西省汾阳医院就诊的首发围绝经期抑郁症病人127例纳入围绝经期抑郁症组,年龄45~54(48.82±2.09)岁;选取同期于我院进行体检的围绝经期妇女200名纳入对照组,年龄45~54(48.71±1.91)岁。本研究经我院伦理委员会批准,所有入选人员及其家属均知情同意。纳入标准:符合围绝经期诊断标准者[12];符合抑郁症诊断标准者[13];首发抑郁症,且近2个月内未经过抗抑郁治疗;配合本次研究,依从性较高者;意识清楚,可正常交流者。排除标准:围绝经期前患有除抑郁症外其他精神类疾病者;患有卵巢早衰症或切除卵巢者;存在严重自杀或自残倾向、存在躯体化症状者;既往药物或酒精依赖史者;伴有严重器质性疾病或恶性肿瘤者。
1.2 观察指标
1.2.1 一般资料
依据我院电子病历及基础情况调查表,收集年龄、体质指数(body mass index,BMI)、孕次、产次、婚姻满意度、文化程度、职业类型、初潮时间、既往月经状态、慢性病数量等。
1.2.2 血清学指标
所有妇女均于就诊日当天清晨空腹抽取静脉血5 mL,采用酶联免疫吸附法(ELISA)检测两组血清中性激素及神经递质因子水平,其中性激素包括E1、E2、血清催乳素(prolactin,PRL)、FSH和LH;神经递质因子包括去甲肾上腺素(noradrenaline,NE)、多巴胺(dopamine,DA)、脑源性神经营养因子(brain?derived neurotrophic factor,BDNF)和5?羟色胺(5?hydroxytryptamine,5?HT)。
围绝经期抑郁症组病人分别于就诊日当天和就诊3个月、6个月及12个月后抽取清晨空腹静脉血5 mL,采用ELISA检测两组血清中E1、E2、PRL、FSH、LH、NE、DA、BDNF、5?HT水平。
1.2.3 认知功能评估
围绝经期抑郁症组病人分别于就诊当天和就诊后3个月、6个月及12个月后采用中文版蒙特利尔认知评估量表(Montreal Cognitive Assessment,MoCA)评估病人认知功能,量表总分0~30分,包括抽象能力(0~2分)、语言(0~3分)、命名(0~3分)、视空间与执行功能(0~5分)、延迟记忆(0~5分)、注意力(0~6分)、定向力(0~6分)和记忆力(不计分)8个分量表[14]。
1.3 统计学分析
采用SPSS 26.0软件对数据进行处理。符合正态分布的定量资料以均数±标准差(x±s)表示,两组比较采用独立样本t检验或单因素方差分析;定性资料以例数、百分比(%)表示,两组比较采用χ2检验或Fisher精确检验。使用Pearson相关性分析性激素、神经递质水平与认知功能的相关性;采用多因素Logistic回归分析探讨影响因素。以P<0.05为差异有统计学意义。
2 结果
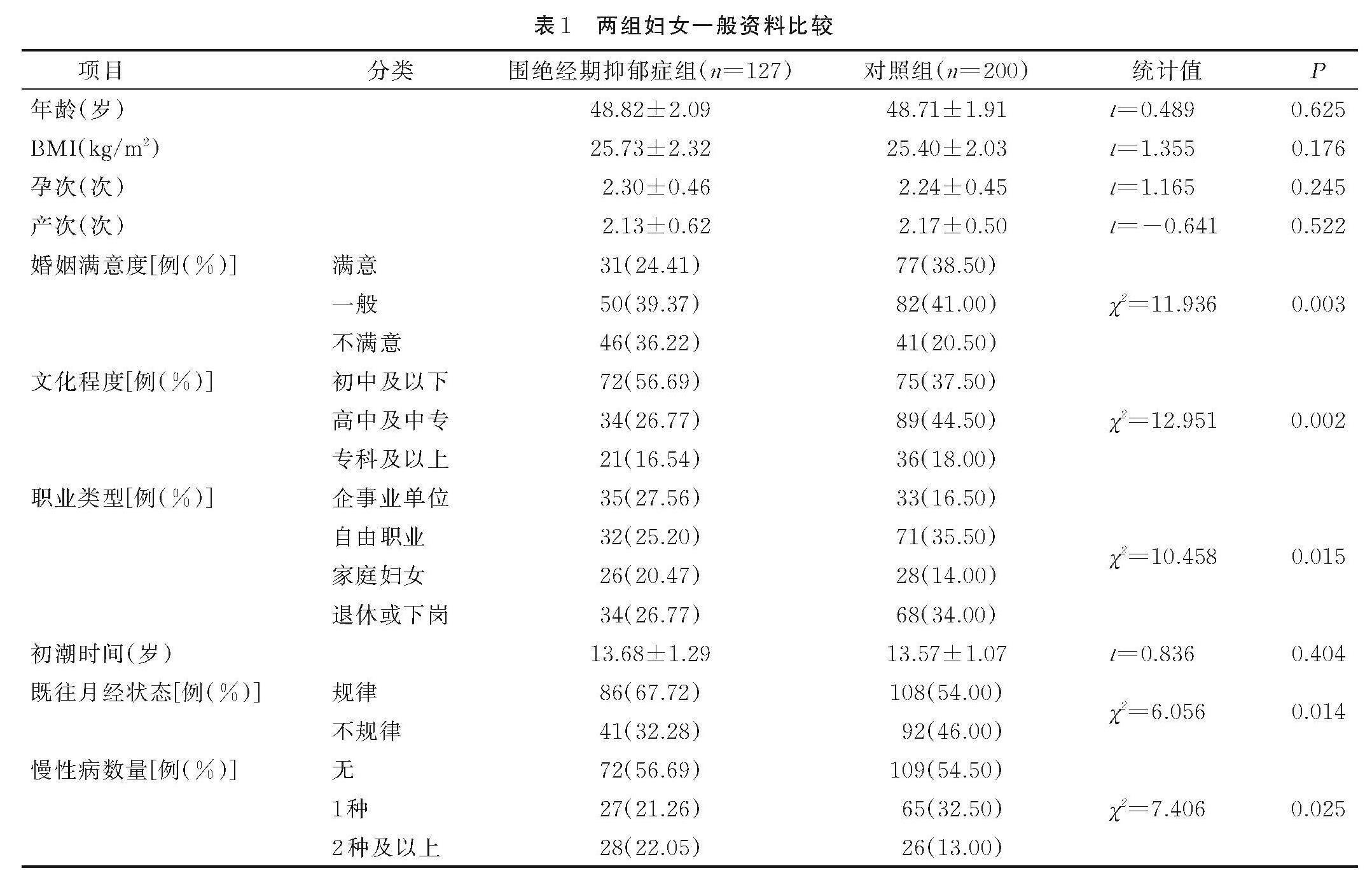
2.1 两组妇女一般资料比较
围绝经期抑郁症组与对照组年龄、BMI、孕次、产次、初潮时间比较差异均无统计学意义(P>0.05);围绝经期抑郁症组与对照组婚姻满意度、文化程度、职业类型、既往月经状态、慢性病数量比较差异均有统计学意义(P<0.05),见表1。
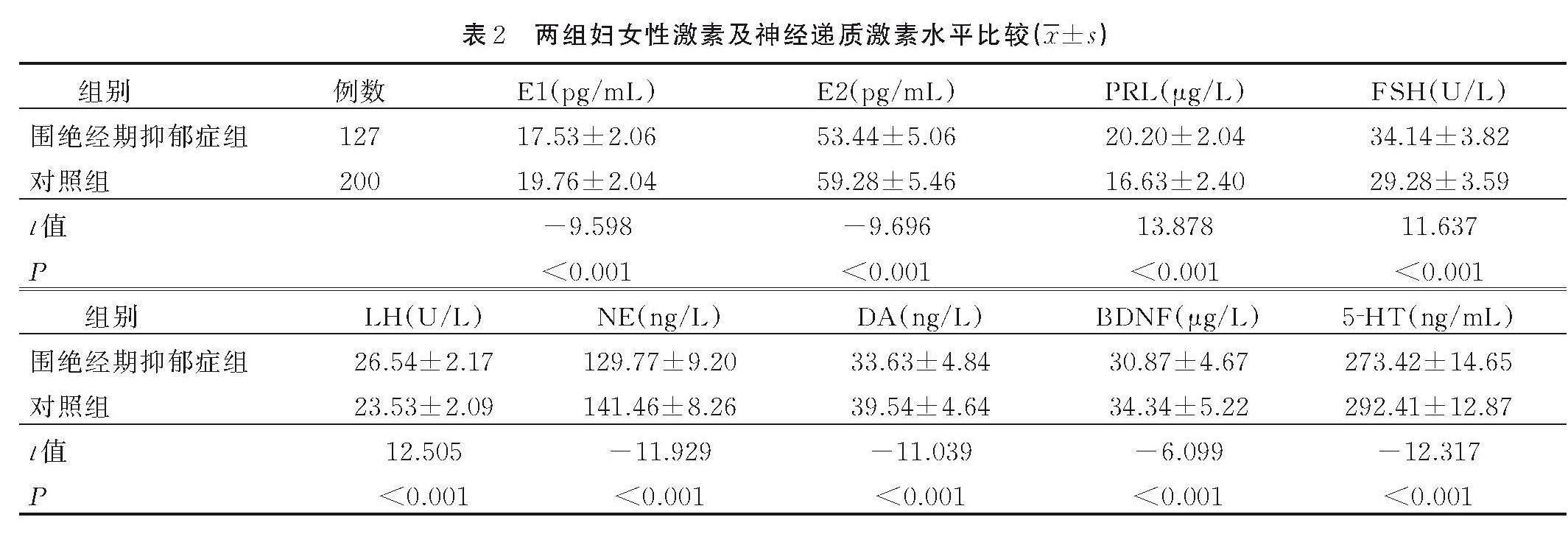
2.2 两组妇女就诊时性激素及神经递质激素水平比较
围绝经期抑郁症组妇女E1、E2、NE、DA、BDNF、5?HT水平低于对照组(P<0.05);围绝经期抑郁症组妇女PRL、FSH、LH水平高于对照组(P<0.05),见表2。
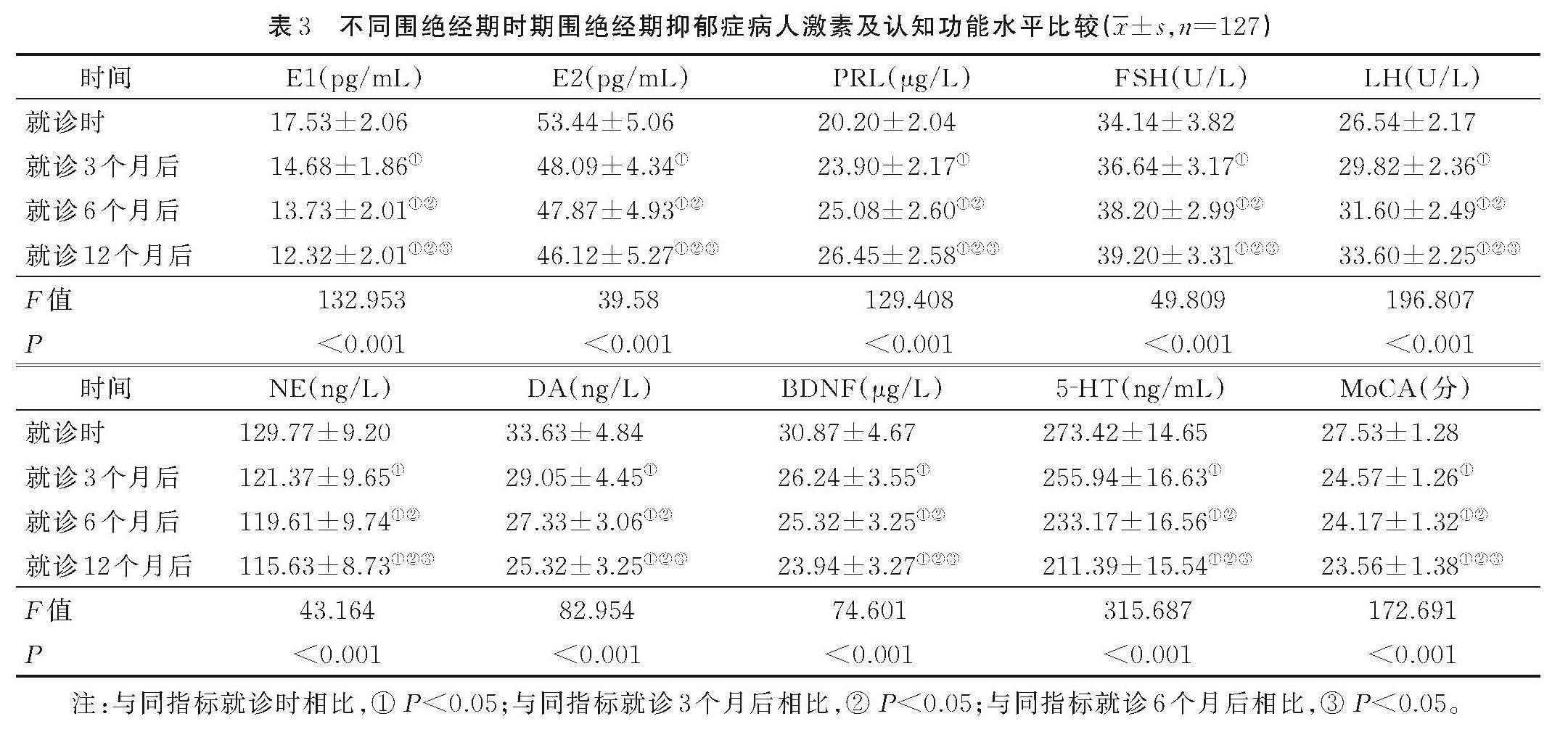
2.3 不同时期围绝经期抑郁症病人激素及认知功能比较
随时间发展,围绝经期抑郁症病人E1、E2、NE、DA、BDNF、5?HT及MoCA评分呈现逐渐降低趋势,且各时间点间比较差异均有统计学意义(P<0.05);随时间发展,围绝经期抑郁症组病人PRL、FSH、LH水平呈现逐渐上升趋势,且各时间点间比较差异均有统计学意义(P<0.05),见表3。
2.4 血清激素动态水平与认知功能的相关性
经Pearson相关性分析结果显示,就诊时、就诊3个月、6个月、12个月后,围绝经期抑郁症病人MoCA评分与E1、E2、NE、DA、BDNF、5?HT水平呈正相关(P<0.05);就诊时、就诊3个月、6个月、12个月后,围绝经期抑郁症病人MoCA评分与PRL、FSH、LH水平呈负相关(P<0.05),见表4。
2.5 不同认知功能病人的基本资料和实验室指标比较
根据病人就诊后12个月MoCA评分将围绝经期抑郁症病人分为认知障碍组(n=94)和认知正常组(n=33)。两组病人年龄、BMI、孕次、产次、职业类型、初潮时间、慢性病数量等比较差异均无统计学意义(P>0.05);认知障碍组病人与认知正常组病人婚姻满意度、文化程度、既往月经状态比较差异均有统计学意义(P<0.05);认知障碍组病人E1、E2、NE、DA、BDNF、5?HT、MoCA评分低于认知正常组病人(P<0.05);认知障碍组病人PRL、FSH、LH水平高于认知正常组病人(P<0.05),见表5。
2.6 围绝经期抑郁症病人激素水平与认知障碍的相关性
将激素指标纳入Logistic回归模型中,逐步排除存在共线性的混杂因素,矫正病人年龄、BMI、职业类型、慢性病数量、孕次、产次、初潮时间、既往月经状态、婚姻满意度、文化程度等协变量后,激素指标与围绝经期抑郁症病人认知障碍风险仍有相关性(P均<0.001);将激素指标水平根据中位数转化为二分类变量后,激素水平与围绝经期抑郁症病人认知障碍风险存在相关性(P均<0.001);将激素水平转化为五分位数组后,随激素水平的变化,围绝经期抑郁症病人认知障碍发生趋势性检验有统计学意义(均P<0.001),见表6。
3 讨论
处于围绝经期时,女性卵巢处于功能衰退状态,机体激素水平发生显著改变,此时期是女性抑郁发生的易感时期,且易发展为重度抑郁[15]。抑郁症属于精神障碍类疾病,其主要临床症状为兴趣缺失、意识活动减退、情绪低落等,且该类临床症状是长期的,严重者还会出现躯体化症状,诱发病人自残或自杀行为,对病人生活及社会造成严重影响[16]。围绝经期抑郁症常发生于围绝经期,除常见抑郁症状之外,还存在食欲减退、注意力分散、睡眠障碍等非典型临床症状[17]。随着心理学临床诊疗技术的飞速发展,围绝经期抑郁症检出率也呈现逐年上升趋势,在围绝经期抑郁症病人群体中,有50%~60%的病人为轻度抑郁,10%~30%的病人为重度抑郁,而重度抑郁是导致健康女性致残致死的第二大因素[18]。抑郁不仅会影响病人正常生活与社交,还会对病人神经认知功能造成损害。有研究表明,认知功能损害伴随抑郁症病人整个病程,对抑郁症病情进展及预后造成一定程度的影响[19]。
目前临床认为,围绝经期妇女卵巢所分泌的卵泡数量减少、雌激素水平降低等因素导致女性卵巢功能衰退,而性激素水平的降低还会造成女性下丘脑、垂体等内分泌相关器官功能衰退,进而诱发女性围绝经期内分泌失调[20?21]。在女性机体所有雌激素中,E2活性最高,当E2水平降低时,会导致机体促性腺激素LH及FSH水平上升,进而诱发机体内分泌系统紊乱,内环境发生异常,而单胺类神经递质水平受到性激素的影响,故而围绝经期女性更易发生心理疾病[22]。本研究结果显示,围绝经期抑郁症组病人雌激素E1、E2水平明显低于对照组,且围绝经期抑郁症组病人性激素PRL、FSH、LH水平明显高于对照组,同时围绝经期抑郁症组病人神经递质因子NE、DA、BDNF、5?HT水平也与对照组健康妇女存在明显差异,这与以往研究[23?24]一致。在本研究中,经单因素分析可知,除性激素及神经递质因子水平外,婚姻满意度、文化程度等社会因素也会对围绝经期抑郁症的发生造成一定的影响,可能是由于家庭亲密度及家庭支持对女性心理健康的影响较大。有研究表明,来自配偶的支持与鼓励是抑郁症较为重要的中介因子[25]。张晓丽等[26]的研究显示,采用阶梯式护理模式对缓解更年期女性抑郁症具有积极的意义。
由于围绝经期女性性激素水平处于动态变化的状态,因此,在对围绝经期抑郁症病人认知功能与性激素水平的相关性研究中,还应将性激素水平动态变化纳入研究范围。本研究结果显示,围绝经期抑郁症病人在围绝经期,随着时间进展,其E1、E2水平呈现逐渐降低趋势,而PRL、FSH、LH水平呈现逐渐上升趋势,同时随着时间进展,病人认知功能也逐渐降低。经Pearson相关性分析显示,E1、E2与病人认知功能呈正相关,而PRL、FSH、LH水平呈负相关,推测是由于随着时间的推移,病人性激素水平变化更大,造成病人心理状态水平更低,进而出现更低的认知功能,姜文慧等[27]也在其研究中得出相似结论。本研究还存在一定的局限性,即未将围绝经期抑郁症病人所处地区等因素纳入影响范围,因此,在今后的研究中,可对此类因素进行控制,对研究结果进行进一步论证。
4 小结
综上所述,首发围绝经期抑郁症病人雌激素水平与病人认知功能存在一定的相关性,同时围绝经期抑郁症的发生也与病人婚姻满意度、文化程度等社会因素相关,表明围绝经期抑郁症的发生机制是多方面的,应在女性围绝经期对其激素水平及日常生活进行综合分析,评估其罹患围绝经期抑郁症的可能性,以便尽早进行治疗,提高病人围绝经期生活质量。
参考文献:
[1] INAYAMA Y,MIZUNO K,YAMAGUCHI K,et al.Hormone replacement therapy and cancer risks in perimenopausal women:a retrospective cohort study using a Japanese claims database[J].The Journal of Obstetrics and Gynaecology Research,2023,49(7):1805-1814.
[2] 《围绝经期综合征(更年期综合征)重点人群治未病干预指南》编写组,中国医学科学院北京协和医院.围绝经期综合征(更年期综合征)重点人群治未病干预指南[J].北京中医药大学学报,2023,46(8):1048-1062.
Writing Group of "Guideline for prevention and intervention of perimenopausal syndrome in key populations",Peking Union Medical College Hospital,Chinese Academy of Medical Sciences.Guidelines for prevention and intervention of perimenopausal syndrome in key populations [J]. Journal of Beijing University of Chinese Medicine,2023,46(8):1048-1062.
[3] WILLI J,EHLERT U.Symptoms assessed in studies on perimenopausal depression:a narrative review[J].Sexual & Reproductive Healthcare,2020,26:100559.
[4] FENG J L,WANG W,ZHONG Y,et al.Acupuncture for perimenopausal depressive disorder:a systematic review and meta-analysis protocol[J].Medicine,2019,98(7):e14574.
[5] GORDON J L,HALLERAN M,BESHAI S,et al.Endocrine and psychosocial moderators of mindfulness-based stress reduction for the prevention of perimenopausal depressive symptoms:a randomized controlled trial[J].Psychoneuroendocrinology,2021,130:105277.
[6] STICKEL S,WAGELS L,WUDARCZYK O,et al.Neural correlates of depression in women across the reproductive lifespan:an fMRI review[J].Journal of Affective Disorders,2019,246:556-570.
[7] GENG Z X,NIE X L,LING L L,et al.Electroacupuncture may inhibit oxidative stress of premature ovarian failure mice by regulating intestinal microbiota[J].Oxidative Medicine and Cellular Longevity,2022,2022:4362317.
[8] CI?LAK M,KRUSZELNICKA I,ZEMBRZUSKA J,et al.Estrogen pollution of the European aquatic environment:a critical review[J].Water Research,2023,229:119413.
[9] 朱艳琼,韩宝三.天然雌激素雌酮、雌二醇和雌三醇的分析检测进展[J].化学世界,2020,61(4):237-244.
ZHU Y Q,HAN B S.Progress in detection of natural estrogens of estrone,estradiol and estriol[J].Chemical World,2020,61(4):237-244.
[10] 曹悦,崔健,肖心怡,等.抑郁症神经认知功能障碍的研究进展及其心理评估[J].神经疾病与精神卫生,2023,23(4):264-269.
CAO Y,CUI J,XIAO X Y,et al.Research progress on neurocognitive dysfunction in depression and its psychological assessment[J].Journal of Neuroscience and Mental Health,2023,23(4):264-269.
[11] 李慧敏,王晓霞,金莉娅,等.盐酸帕罗西汀联合利维爱治疗围绝经期抑郁症的疗效观察[J].中国妇幼保健,2019,34(9):2058-2060.
LI H M,WANG X X,JIN L Y,et al.Clinical observation of paroxetine hydrochloride combined with livial in the treatment of perimenopausal depression[J].Maternal and Child Health Care of China,2019,34(9):2058-2060.
[12] 贝政平,来佩琍,张斌.妇产科疾病诊断标准[M].北京:科学出版社,2007:55-59.
BEI Z P,LAI P L,ZHANG B.Diagnostic criteria for gynecological and obstetrical diseases [M].Beijing:Science Press,2007:55-59.
[13] 范肖冬.ICD-10精神与行为障碍分类:临床描述与诊断要点[M].北京:人民卫生出版社,1993:97-100.
FAN X D.ICD-10 classification of mental and behavioral disorders:clinical description and diagnostic points [M].Beijing:People's Medical Press,1993:97-100.
[14] 李怀苏,周雯,曾天芳,等.阿尔茨海默病患者睡眠结构异常与认知功能 MMSE、MoCA 评分的相关性研究[J].医学临床研究,2019,36(10):1890-1892.
LI H S,ZHOU W,ZENG T F,et al.Correlation between sleep structure abnormalities and cognitive function scores(MMSE and MoCA) in patients with Alzheimer's disease[J].Journal of Clinical Research,2019,36(10):1890-1892.
[15] MULHALL S,ANDEL R,ANSTEY K J.Variation in symptoms of depression and anxiety in midlife women by menopausal status[J].Maturitas,2018,108:7-12.
[16] 徐珒昭,马岩石,王丹萍,等.基于“微生物-肠-脑”轴的肠道菌群参与抑郁症相关研究进展[J].食品科学,2023,44(5):383-391.
XU J Z,MA Y S,WANG D P,et al.Progress in research on the involvement of intestinal flora in depression based on the "microbial-gut-brain" axis[J].Food Science,2023,44(5):383-391.
[17] MAKI P M,KORNSTEIN S G,JOFFE H,et al.Guidelines for the evaluation and treatment of perimenopausal depression:summary and recommendations[J].Journal of Women's Health,2019,28(2):117-134.
[18] 梁慧,杜忠剑.解结针法治疗围绝经期抑郁状态的疗效研究[J].针灸临床杂志,2020,36(2):42-45.
LIANG H,DU Z J.Effect of Jiejie acupuncture therapy on perimenopausal depression[J].Journal of Clinical Acupuncture and Moxibustion,2020,36(2):42-45.
[19] 米文芳,董强利,张兰.青少年抑郁症认知功能损害及影响因素的研究进展[J].新医学,2023,54(1):13-16.
MI W F,DONG Q L,ZHANG L.Research progress on cognitive impairment and influencing factors in adolescents with depression[J].Journal of New Medicine,2023,54(1):13-16.
[20] BACON E R,MISHRA A,WANG Y W,et al.Neuroendocrine aging precedes perimenopause and is regulated by DNA methylation[J].Neurobiology of Aging,2019,74:213-224.
[21] 过亚群,陈晔,陈美娟.基于《内经》论妇女围绝经期综合征的病机及治疗[J].四川中医,2019,37(12):20-23.
GUO Y Q,CHEN Y,CHEN M J.Pathogenesis and treatment of perimenopausal syndrome in women based on Internal Canon of Medicine[J].Journal of Sichuan of Traditional Chinese Medicine,2019,37(12):20-23.
[22] 权兴苗,王月,宋春侠,等.针灸对自然衰老围绝经期大鼠雌激素水平及单胺类神经递质的影响[J].中国老年学杂志,2022,42(11):2745-2749.
QUAN X M,WANG Y,SONG C X,et al.Effects of acupuncture and moxibustion on estrogen levels and monoamine neurotransmitters in naturally aging perimenopausal rats[J].Chinese Journal of Gerontology,2022,42(11):2745-2749.
[23] FROKJAER V G.Pharmacological sex hormone manipulation as a risk model for depression[J].Journal of Neuroscience Research,2020,98(7):1283-1292.
[24] HAN Y P,GU S M,LI Y M,et al.Neuroendocrine pathogenesis of perimenopausal depression[J].Frontiers in Psychiatry,2023,14:1162501.
[25] 王进,日火英支,刘佳佳,等.自助式夫妻沟通训练方案对产前抑郁症状及婚姻质量的影响[J].中国心理卫生杂志,2023,37(12):1045-1051.
WANG J,RIHUO Y Z,LIU J J,et al.Effectiveness of self-assisted couple communication program on prenatal depression symptoms and marital quality[J].Chinese Mental Health Journal,2023,37(12):1045-1051.
[26] 张晓丽,祝爱敏,刘楠,等.阶梯式心理护理对胃癌术后老年患者负性情绪和生活质量的影响[J].现代临床护理,2019,18(7):20-24.
ZHANG X L,ZHU A M,LIU N,et al.Effects of stepwise psychological care on anxiety,depression and quality of life in elderly patients with gastric cancer[J].Modern Clinical Nursing,2019,18(7):20-24.
[27] 姜文慧,董莹莹,高成阁,等.更年期抑郁症患者性激素水平与认知功能的关系[J].科学技术与工程,2021,21(3):941-945.
JIANG W W,DONG Y Y,GAO C G,et al.Relationship between sex hormone levels and cognitive function in patients with climacteric depression[J]. Science Technology and Engineering,2021,21(3):941-945.
(收稿日期:2024-04-08;修回日期:2024-06-03)
(本文编辑 崔晓芳)