Cardiac rehabilitation after cardiac surgery: An important underutilized treatment strategy
2024-05-08ChristosKourekStavrosDimopoulos
Christos Kourek,Stavros Dimopoulos
Abstract Physical inactivity remains in high levels after cardiac surgery,reaching up to 50%.Patients present a significant loss of functional capacity,with prominent muscle weakness after cardiac surgery due to anesthesia,surgical incision,duration of cardiopulmonary bypass,and mechanical ventilation that affects their quality of life.These complications,along with pulmonary complications after surgery,lead to extended intensive care unit (ICU) and hospital length of stay and significant mortality rates.Despite the well-known beneficial effects of cardiac rehabilitation,this treatment strategy still remains broadly underutilized in patients after cardiac surgery.Prehabilitation and ICU early mobilization have been both showed to be valid methods to improve exercise tolerance and muscle strength.Early mobilization should be adjusted to each patient’s functional capacity with progressive exercise training,from passive mobilization to more active range of motion and resistance exercises.Cardiopulmonary exercise testing remains the gold standard for exercise capacity assessment and optimal prescription of aerobic exercise intensity.During the last decade,recent advances in healthcare technology have changed cardiac rehabilitation perspectives,leading to the future of cardiac rehabilitation.By incorporating artificial intelligence,simulation,telemedicine and virtual cardiac rehabilitation,cardiac surgery patients may improve adherence and compliance,targeting to reduced hospital readmissions and decreased healthcare costs.
Key Words: Cardiac rehabilitation;Cardiac surgery;Cardiopulmonary exercise testing;Early mobilization;Treatment;Technology
INTRODUCTION
Cardiac surgery includes a variety of procedures with coronary artery by-pass grafting,valve replacement,aortic/mitral/tricuspid valve replacement or reconstruction,heart transplantation and Bentall surgery being the most frequent among them.Patients present a loss of cognitive and exercise capacity[1],muscle mass[2] and quality of life[3,4] after cardiac surgery due to anesthesia,surgical incision,duration of cardiopulmonary bypass,and mechanical ventilation[5].These complications,along with pulmonary complications after surgery,lead to extended intensive care unit (ICU) and hospital length of stay and significant mortality rates[5].Physical inactivity remains high after cardiac surgery,reaching up to 49%in these patients[6].Moreover,physical inactivity,even late after cardiac surgery,is associated with increased long-term mortality[6].
Cardiac rehabilitation is designed to improve cardiovascular health in patients with cardiovascular diseases and is recommended by guidelines as Class IA[7,8].In cardiac surgery,cardiac rehabilitation is associated with a lower 2-year mortality[9].Despite the well-known beneficial effects of cardiac rehabilitation after cardiac surgery,this treatment strategy still remains underutilized due to low rates of referrals,adherence and compliance.The aim of the present editorial is to highlight the role of cardiac rehabilitation in cardiac surgery and demonstrate the most recent advances in this field.
EARLY MOBILIZATION AND PREHABILITATION
Early mobilization should be considered as an important preventive and treatment method for ICU acquired weakness in patients after cardiac surgery.Despite its safety,feasibility,beneficial effects on exercise capacity[10] and its association with reduced length of ICU stay[11],more studies are required in order to provide confirming evidence[12].Early mobilization should be adjusted to each patient’s functional capacity,initiating from passive mobilization such as stretching,splinting,passive movements and neuromuscular electrical stimulation (NMES),and increasing the functional status with simple active range of motion and resistance exercises including sitting in a chair,leg press,squats from sitting position,walking,biking on an exercise bike,walking on stairs and inspiratory muscle training[13,14].Passive mobilization and NMES are usually implemented in intubated patients under mechanical ventilation,high-risk patients with hemodynamic instability or patients with reduced consciousness while active-assisted range-of motion exercises,inspiratory muscle training and resistance exercises are implemented in those who need mobilization after cardiac surgery,with satisfactory level of consciousness[13,14].In general,early mobilization has been shown safe and feasible in cardiovascular diseases[15-17] and critically ill patients[18],as well as in other medical conditions such as subarachnoid hemorrhage and external ventricular drain[19],continuous renal replacement therapy[20] and sepsis[21,22].Beyond all its beneficial effects,early mobilization of cardiac surgery patients requires close monitoring in the ICU due to possible side effects,including significant hemodynamic changes[23].As a result,expert multidisciplinary team approach and individualized rehabilitation program,adjusted to the patient’s functional status,are necessary in order to minimize adverse events[24].
Prehabilitation is another novel modality of rehabilitation defined as a process of improving functional capability of a patient prior to a surgical procedure.Recent studies have demonstrated that prehabilitation seems to improve functional capacity and enhance postoperative recovery in patients undergoing cardiothoracic surgery[25,26].Moreover,prehabilitation contributes to better quality of life in patients with stable coronary artery disease awaiting cardiac surgery[27].Growing evidence supports prehabilitation even in patients with advanced heart failure or extracorporeal membrane oxygenation as a bridge to left ventricle assist device or heart or lung transplantation.In these cases,prehabilitation should be performed daily for approximately 60 min including airway clearance techniques and ventilation in prone and supine position when required,and in-bed active-assisted range of motion exercises including sitting at the bedside,standing balance and tolerance,rolling,stretching,positioning in bed,strengthening and reconditioning exercises in the supine position,bedside cycling,inspiratory muscle training,out-of-bed activities such as standing at the bedside,strength of standing force,sitting on the edge of the bed and transfer from bed to chair,exercises in the sitting position on the edge of the bed,aerobic training on a cycle ergometer or a treadmill and inspiratory muscle training according to patient's functional capacity[14].
EXERCISE PRESCRIPTION
Exercise prescription is a quite complex procedure,especially in patients after cardiac surgery.The most difficult part is to establish the beneficial “dose” of exercise in order to achieve the maximum beneficial results and avoid harmful effects.Clinical assessment and risk stratificationviatransthoracic echocardiography and cardiopulmonary exercise testing(CPET) are required prior to participation in such rehabilitation programs.CPET is the gold standard for the prescription of maximum aerobic exercise intensity[28].Monitoring of heart rate (HR) dynamics and ventilation,as well as metabolic parameters such as oxygen uptake (VO2) and carbon dioxide output (VCO2),provides objective measurements of respiratory,metabolic,and cardiovascular responses to exercise and creates an individualized program for each patient[29].Therefore,exercise training can be classified in four intensity domains,based on the percentage of peak VO2,HR,HR reserve,and Borg scale;light to moderate,moderate to high,high to very high,and very high intensity[30].In the first phase of rehabilitation,it is usually suggested to start with lower intensities of exercise and mostly work on both frequency and duration of each session,rather than intensity.Intensity should be maintained quite constantly,close to the lowest limit of the moderate intensity range,and then,increase to higher levels depending on the rehabilitation phase and the individualized needs[30].
RECENT ADVANCES IN CARDIAC REHABILITATION
During the last decade,recent advances have been made in cardiac rehabilitation.Rapidly-advanced technology is the cornerstone in the future of cardiac rehabilitation.Wearables such as fitness bands and smartwatches that monitor heart rhythm during exercise in order to detect arrhythmias are used by 5% to 11% of the world’s adult population[31].Intelligent computing including artificial intelligence (AI) and complex modeling are now increasingly used in biologic systems so that to create individualized rehabilitation programs[32].Specifically,AI could estimate and quantify risk assessment of patients before and after cardiac surgeryviaspecial algorithms,using CPET,anaerobic threshold quantification,biomarkers and frailty parameters.Moreover,it could be a useful tool to predict mortality and morbidity[33],and detect dysrhythmias in electrocardiography during rehabilitation with promising results in accuracy and speed of interpretation[34,35],as well as in more advanced imaging such as echocardiography[36] and magnetic resonance imaging[37].Other significant variables,including simulation and telemedicine,could be valuable for solving access problems due to disparities,disabilities,long physical distance from health care centers,and lack of expertise and specialized personnel,as well as for high-risk situations such as virulent infections and combat[32].Virtual cardiac rehabilitation has been also shown to improve patients' adherence and compliance,reduce hospital readmissions,and decrease associated costs and cardiovascular risk[38,39].Synchronous audiovisual technology is used to supervise patient exercise and provide education in real-time.Technological advances should translate into actual benefits for patients and health care providers,providing higher-quality of services and safety in health care systems[32].
Cardiac rehabilitation,with its traditional form,is an individualized,patient-centered program.However,the future of cardiac rehabilitation will include more options for participants with in-person visits,virtual one-on-one visits,virtual group visits,and asynchronous exercise with or without remote monitoring[40].The choice whether the participation will include exclusively one delivery mode or a hybrid of 2 or more delivery modes depends on many variables related with the participants,such as their physical status,their opportunity of participation,the distance from the rehabilitation facilities,etc.
Finally,cardiac rehabilitation includes modification of previous lifestyle habits including smoking and alcohol cessation,loss of weight and medication adherence.Synchronous interventionsviatelemedicine could be used to improve access to these services,such as consultation with a registered dietitian or a behavioral therapist[40].Core advances of a cardiac rehabilitation program are demonstrated in Figure 1.
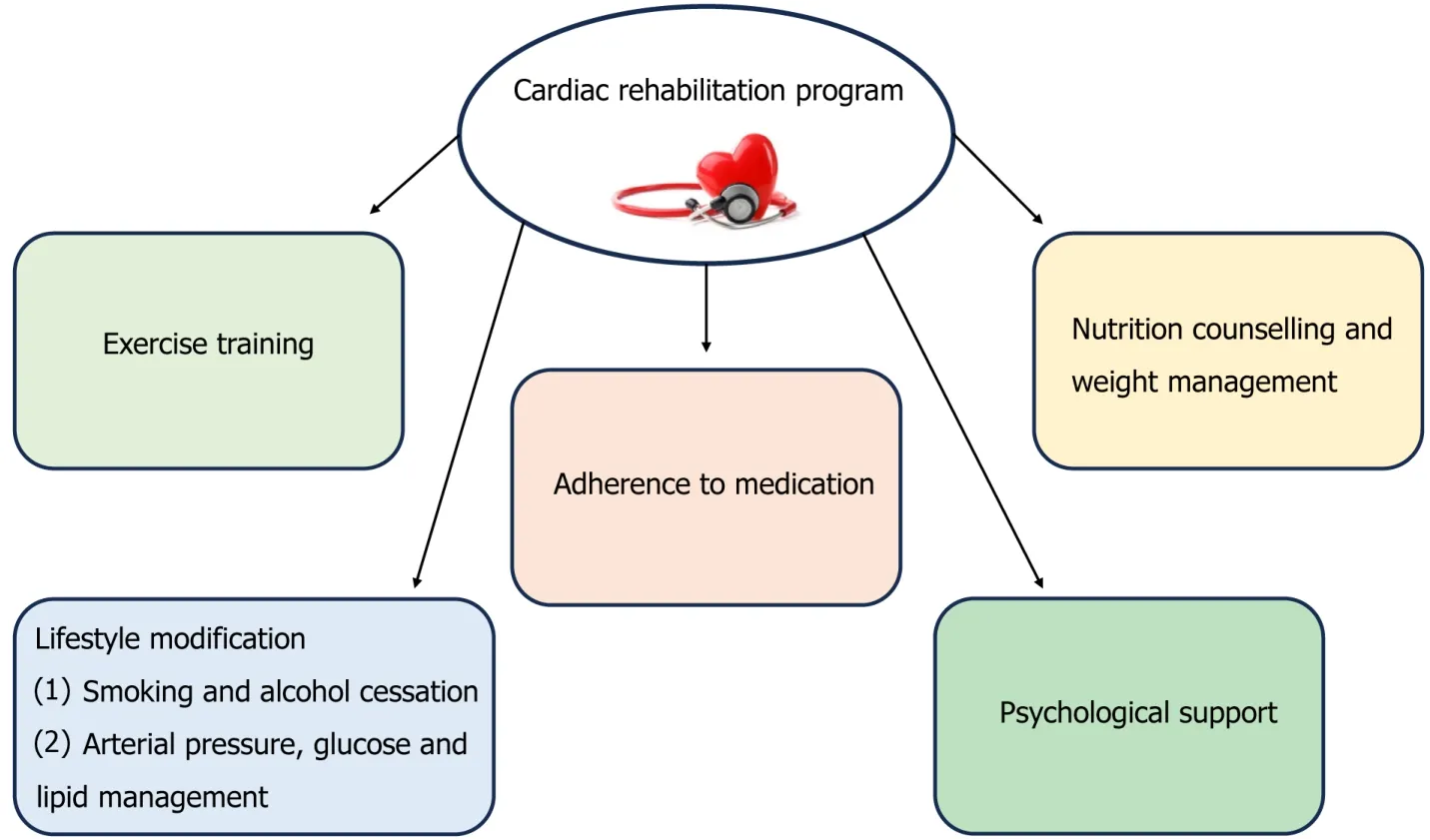
Figure 1 Components of a cardiac rehabilitation program.
CONCLUSION
Cardiac rehabilitation is a complex and multicomponent procedure that requires a multidisciplinary approach and includes physical activity promotion,health education,cardiovascular risk management and psychological support,personalized to the individual needs of patients after cardiac surgery.CPET remains the gold standard method for the prescription of optimal aerobic exercise intensity.Recent advances in cardiac rehabilitation have been made during the last decade,including the use of AI,simulation,telemedicine,and virtual cardiac rehabilitation that have improved adherence and compliance,and reduced hospital readmission,with decreased associated healthcare cost.However,new innovations are required in order to increase rates of patients’ participation and create ideal individualized protocols for each patient.
FOOTNOTES
Author contributions:Kourek C and Dimopoulos S contributed to this paper;Dimopoulos S designed the overall concept and outline of the manuscript;Kourek C contributed to the discussion and design of the manuscript;Kourek C and Dimopoulos S contributed to the writing,editing the manuscript,illustrations,and review of literature.
Conflict-of-interest statement:Authors have no conflict of interest to declare.
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers.It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license,which permits others to distribute,remix,adapt,build upon this work non-commercially,and license their derivative works on different terms,provided the original work is properly cited and the use is non-commercial.See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:Greece
ORCID number:Christos Kourek 0000-0003-4348-2153;Stavros Dimopoulos 0000-0003-2199-3788.
S-Editor:Chen YL
L-Editor:A
P-Editor:Zhang YL
杂志排行
World Journal of Cardiology的其它文章
- Facing ethical concerns in the age of precise gene therapy: Outlook on inherited arrhythmias
- Spontaneous coronary artery rupture after lung cancer surgery: A case report and review of literature
- Development and validation of a nomogram model for predicting the risk of pre-hospital delay in patients with acute myocardial infarction
- Seeing beneath the surface: Harnessing point-of-care ultrasound for internal jugular vein evaluation
- Risk of permanent pacemaker implantation following transcatheter aortic valve replacement: Which factors are most relevant?
- Inflammation as a cause of acute myocardial infarction in patients with myeloproliferative neoplasm