Two big orifices in the second duodenal portion: A case of an atypical double papilla
2024-03-04SlvtoreFrnesoVdldiPrmperoNikolPniMroMssiddChirRohiPierluigiMriRinldiAnMlenkoviMilutinBulji
Slvtore Frneso Vdlà di Prmpero ,Nikol Pni ,Mro Mssidd ,Chir Rohi ,Pierluigi Mri Rinldi ,An Mlenkovi ,Milutin Bulji
a Gastroenterology and GI Endoscopy Department, Mater Olbia Hospital, Olbia 07026, Italy
b Digestive Endoscopy Unit, University Clinic "Dr Dragisa Misovic-Dedinje", Belgrade 11000, Serbia
c Radiology Department, Mater Olbia Hospital, Olbia 07026, Italy
With the advent of endoscopic retrograde cholangiopancreatography (ERCP) in the early 1970s,anatomic anomalies of the Vaterian system were described endoscopically [1].Although the occurrence is rare,the common bile duct (CBD) and the pancreatic duct may fail to coalesce during embryologic development.This leads to double major papilla because both ducts open into the duodenum separately [1].In this way the cranial duct communicates with the CBD,while the caudal orifice communicates with the pancreatic duct [2].
Herein we presented a case with two separate drainage orifices,the cranial one communicating only with the bile duct and the caudal draining both the bile and pancreatic ducts,resulting in an atypical double papilla.This resulted in a double sphincterotomy in order to ease the biliary drainage avoiding residual debris in the mucosal limb between the two orifices.
A 53-year-old man was transferred to our tertiary care center with jaundice,recurrent acute right upper quadrant abdominal pain associated with neutrophilic leukocytosis and abnormal liver function tests [white blood cell (WBC) 10.8×109/L,neutrophil 8.9×109/L,aspartate aminotransferase (AST) 267 U/L,alanine aminotransferase (ALT) 433 U/L,total bilirubin 10.32 mg/dL,direct bilirubin 5.96 mg/dL,gamma-glutamyltransferase (GGT) 327 U/L,CRP 0.5 mg/dL].Abdominal ultrasound demonstrated gallbladder stones and bile ducts dilatation.Magnetic resonance cholangiopancreatography (MRCP) showed a small CBD stone and that the duct of Wirsung was slightly dilated in the head of the pancreas (Fig.1 A).Endoscopic examination during ERCP revealed a double orifice major papilla (Fig.1 B),with a minimum bile outflow from both orifices.After careful assessment,the cranial orifice at 11 o’clock was cannulated,and cholangiogram confirmed a mildly dilated CBD (Fig.1 C).Sphincterotomy and balloon stone extraction were performed (Fig.1 D and E).Subsequently the caudal orifice at 5 o’clock was cannulated (Fig.1 F) by a sphincterotome and a guidewire was placed again in the CBD.A second sphincterotomy was performed by cutting the mucosal limb and the muscular fibers between the two orifices (Fig.1 G) in order to facilitate biliary drainage and to avoid residual debris.After the second sphincterotomy,the main pancreatic duct orifice appeared clearly and was located in the inner part of the original caudal orifice(Fig.1 H).Pancreatogram was not performed since it was normal on MRCP.Two days after the procedure,the laboratory examination showed an improvement in the liver function profile (GGT 170 U/L,AST 67 U/L,ALT 250 U/L,total bilirubin 3.90 mg/dL,direct bilirubin 2.52 mg/dL).The patient underwent subsequent cholecystectomy,and his hospital course was uneventful.
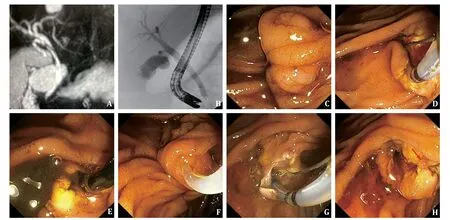
Fig.1. MRCP (A) and cholangiogram (B) show normal bilio-pancreatic ducts.Endoscopic view of the double papilla (C) and sphincterotomy from the cranial orifice (D) with drainage of dark bile (E).Cannulation of the caudal orifice (F) and cut of the mucosal limb between the two orifices (G) with evidence of the pancreatic orifice (arrow) (H).MRCP: magnetic resonance cholangiopancreatography.
The double major papilla is a very rare anatomical variant with changes in the bile duct and pancreatic duct opening due to the process of rotation and recanalization during embryologic development [3].This process determines the development of two separate orifices,the CBD and the main pancreatic duct [4–7].
In the case of choledocholithiasis,the clinical presentation and the endoscopic management of patients with double major papilla are similar to those of patients with normal anatomy.The treatment is by an ERCP with sphincterotomy of the cranial orifice that drains bile and subsequent debris removal.
On the other hand,the presentation and management of choledocholithiasis are different between patients with double major papilla and those with choledochoduodenal fistula.The clinical picture of choledochoduodenal fistula is usually characterized by a single episode of cholangitis,the endoscopic appearance is characterized by an orifice with regular or irregular non-granular margins,and the cholangiogram shows air in the biliary tree [8].The endoscopic management of choledochoduodenal fistula is by an ERCP with a sphincterotomy from the sphincter of Oddi reaching the fistulous orifice with subsequent CBD debris removal.
The case we described is different from both typical double major papilla and choledochoduodenal fistula: the clinical picture (recurrent cholangitis),the endoscopic aspect (two granular orifices draining bile),and the radiologic imaging on ERCP (cannulation of main bile duct from both the orifices,no air finding in the biliary tree) can be helpful to detect this very rare condition,in which the cranial orifice communicates only with the bile duct and the caudal one communicates with both bile and pancreatic ducts (Fig.2).

Fig.2. Anatomy of atypical double papilla.CBD: common bile duct.
In this situation,MRCP was useful to provide a whole picture of the pancreatobiliary tract and to exclude a pancreatobiliary maljunction [9,10].Anyway,not like endoscopic and ERCP imaging,MRCP is not able to identify an atypical double major papilla,because the bilio-pancreatic tract could seem to be regular on MRCP,not detecting the double orifice that will appear only during the endoscopic examination and appropriate cholangiogram.
Endoscopists should be aware of this rare variant of double major papilla.Its misleading interpretation can result in a single sphincterotomy of the cranial orifice with possible accumulation of debris in the residual ampulla between the two orifices,similar to what happens in the so called “sump syndrome” after choledochoduodenostomy [11].
When discussing anomalies of the Vaterian system,it is important to mention the pancreas divisum,the most common congenital malformation of the pancreas which occurs due to a failure of fusion of the ductal systems of the dorsal and ventral pancreatic buds.This leads to a dominant dorsal pancreatic duct draining through the minor papilla and a small ventral pancreatic duct draining through the major papilla [12].Three clinical conditions are associated with pancreas divisum: acute recurrent pancreatitis,chronic pancreatitis with chronic inflammation in the dorsal bed and abdominal “pancreatic-type” obstructive pain.Pancreas divisumpersedoes not require medical intervention.Patients who experience mild episodic acute pancreatitis should be managed medically.Surgical or endoscopic interventions relieve the obstruction by improving dorsal duct drainage via the minor papilla [13].Nowadays,pancreas divisum is efficiently diagnosed using MRCP and although clinical presentation of patients with pancreas divisum sometimes can be similar to those of double major papilla,MRCP should enable clinicians to discriminate these two entities.
Acknowledgments
None.
CRediT authorship contribution statement
Salvatore Francesco Vadalà di Prampero:Conceptualization,Supervision,Writing– review &editing.Nikola Panic:Conceptualization,Writing– original draft.Marco Massidda:Conceptualization,Writing– original draft.Chiara Rocchi:Conceptualization,Writing– original draft.Pierluigi Maria Rinaldi:Visualization.Ana Malenkovic:Writing– review &editing.Milutin Bulajic:Conceptualization,Writing– original draft.
Funding
None.
Ethical approval
The consent was obtained from the patient for publication of this report.
Competing interest
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- Recent advances in promising drugs for primary prevention of gastroesophageal variceal bleeding with cirrhotic portal hypertension
- Stereotactic body radiotherapy in pancreatic adenocarcinoma
- Application of ultrasonography-elastography score to suspect porto-sinusoidal vascular disease in patients with portal vein thrombosis
- Polydatin ameliorates hepatic ischemia-reperfusion injury by modulating macrophage polarization
- Hypomethylation of glycine dehydrogenase promoter in peripheral blood mononuclear cells is a new diagnostic marker of hepatitis B virus-associated hepatocellular carcinoma
- AGK2 pre-treatment protects against thioacetamide-induced acute liver failure via regulating the MFN2-PERK axis and ferroptosis signaling pathway