Stereotactic body radiotherapy in pancreatic adenocarcinoma
2024-03-04CarolinadelaPinta
Carolina de la Pinta
Radiation Oncology Department, Ramón y Cajal University Hospital, IRYCIS, Alcalá University, 28034 Madrid, Spain
Keywords: Chemoradiotherapy Pancreatic adenocarcinoma Radiotherapy Stereotactic body radiotherapy Stereotactic ablative radiotherapy
ABSTRACT Background: Stereotactic body radiotherapy (SBRT) in pancreatic cancer allows high delivery of radiation doses on tumors without affecting surrounding tissue.This review aimed at the SBRT application in the treatment of pancreatic cancer.Data sources: We retrieved articles published in MEDLINE/PubMed from January 2017 to December 2022.Keywords used in the search included: “pancreatic adenocarcinoma” OR “pancreatic cancer” AND “stereotactic ablative radiotherapy (SABR)” OR “stereotactic body radiotherapy (SBRT)” OR “chemoradiotherapy(CRT)”.English language articles with information on technical characteristics,doses and fractionation,indications,recurrence patterns,local control and toxicities of SBRT in pancreatic tumors were included.All articles were assessed for validity and relevant content.Results: Optimal doses and fractionation have not yet been defined.However,SBRT could be the standard treatment in patients with pancreatic adenocarcinoma in addition to CRT.Furthermore,the combination of SBRT with chemotherapy may have additive or synergic effect on pancreatic adenocarcinoma.Conclusions: SBRT is an effective modality for patients with pancreatic cancer,supported by clinical practice guidelines as it has demonstrated good tolerance and good disease control.SBRT opens a possibility of improving outcomes for these patients,both in neoadjuvant treatment and with radical intent.
Introduction
Pancreatic adenocarcinoma is the fourth most common cause of cancer death.The 5-year survival rate is less than 20%,and the most common form of presentation is in advanced stages.Its causes are not well known;however,there are numerous risk factors involved such as obesity,chronic pancreatitis,exposure to industrial substances,smoking or hereditary syndromes associated with pancreatic cancer or the presence of a family history of pancreatic cancer [1].
The pancreas is divided into head,body and tail.Tumors of the head of the pancreas are the most frequent,accounting for 60%-75% of cases.The symptoms of the disease depend on the stage and location of the tumor.In the early stages,symptoms are nonspecific,but in advanced stages,jaundice,pain and constitutional syndrome,among others,may appear.
Treatment of pancreatic adenocarcinoma should be evaluated by an experienced multidisciplinary team including gastroenterologists,surgeons,pathologists,medical oncologists,radiation oncologists and radiologists.In localized tumors,the treatment of choice is surgery,which offers the only chance of cure.However,at diagnosis,only 15%-20% of patients have resectable tumors,30%-40%have unresectable tumors and 40% have distant metastases [1].
To reduce the risk of recurrence after surgery,different adjuvant treatment schemes with chemotherapy or chemoradiotherapy(CRT) have been proposed,despite which,5-year overall survival rates remain short,around 25%-30% in node-negative patients and 10% in nodal disease.
This review aimed to summarize SBRT and its application in the treatment of pancreatic cancer.We retrieved the pertinent papers published in MEDLINE/PubMed from January 2017 to December 2022.Keywords used in the search included: “pancreatic adenocarcinoma” OR “pancreatic cancer” AND “stereotactic ablative radiotherapy (SABR)” OR “stereotactic body radiotherapy (SBRT)” OR“chemoradiotherapy (CRT)”.English language articles with information on technical characteristics,doses and fractionation,indications,recurrence patterns,local control and toxicities of SBRT in pancreatic tumors were included in this review.
CRT in pancreatic cancer
CRT in pancreatic cancer can be administered neoadjuvantly or adjuvantly.Neoadjuvant CRT improves surgical resections and facilitates the delineation of treatment volumes with radiotherapy,with a low incidence of complications.In addition,the neoadjuvant approach avoids delay of adjuvant chemotherapy treatment.
Locally advanced pancreatic adenocarcinoma could become surgical with neoadjuvant CRT.However,there is a disadvantage:CRT with conventional radiotherapy is a prolonged treatment that forces the delay of other treatments.
In the USA,the use of adjuvant CRT is accepted as a standard treatment,improving overall survival (OS) compared to surgery alone [2].Benefits have also been demonstrated in European studies [1].However,21%-35% of patients are not indicated because of postoperative complications and worsening recovery [3].Adjuvant CRT could delay the initiation of full-dose chemotherapy,in addition to presenting significant difficulty in lesion contouring and poor tolerance of healthy organs [4].
SBRT
SBRT is defined as a high-precision irradiation technique,which allows the administration of very high dose in a limited number of fractions to the tumor.SBRT has highly cytotoxic ablative biological effect,in addition to microvascular and stromal damage to the tumor tissues.Several cases have been described in which SBRT could enhance the anti-tumor immune response (Fig.1) and produce destruction of metastases far from the irradiated lesions [5].
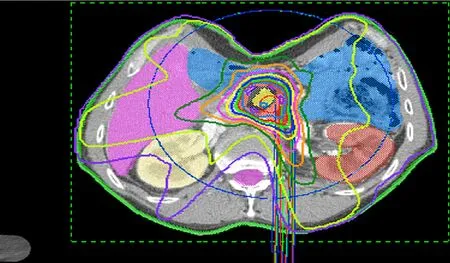
Fig.1. Pancreas SBRT dosimetry.SBRT: stereotactic body radiotherapy.
While conventional radiotherapies are administered in fractions of 1.8 to 2 Gy until doses of 60 or 70 Gy,the doses administered in SBRT exceed 5 Gy per fraction in 1 to 5 fractions,which is a higher radiobiological equivalent [6].
In pancreatic cancer,due to its anatomical location,radiotherapy treatment requires a design that minimizes doses in healthy organs.Therefore,historically the dose to pancreatic tumors has been limited by the tolerance of healthy organs,improving this situation with SBRT since the volumes are focused on the macroscopic tumor without irradiating the nodal areas,decreasing the treatment volumes and thus limiting the doses received by the surrounding healthy organs.
Therefore,SBRT provides advantages over treatment with conventional radiotherapy.On the one hand,it allows high radiation doses to be administered with excellent tolerance of the surrounding healthy tissues.On the other hand,it allows adequate local control without limiting the delay or interruption of systemic treatment,improving pain,and preserving patients’ quality of life.It is also possible to escalate the dose in the vascular area to facilitating R0 resections and decreasing the risk of local recurrence [7].
Technical requirements
SBRT is a technically more complex treatment than standard radiotherapy.The American Association of Physics in Medicine(AAPM) has provided recommendations for the technical requirements of the treatment.After the patient is immobilized,a four-dimensional computed tomography (4DCT) simulation or CT breath-hold with contrast medium is performed in which the treatment is planned.During treatment sessions,image-guided radiation therapy (IGRT) is mandatory.This consists of acquiring images before each treatment,ensuring the correct positioning of the patient and the tumor.A perfect correlation between what is planned days before and what is done on the day of treatment is necessary.For this purpose,it is usual to mark the tumor previously with fiducial marks or surgical clips.In addition,it is important to control tumor movement during irradiation with the techniques currently available dampening with abdominal compressor,respiratory tracking or respiratory gating systems [8].
Dose and fractionation
Pollom et al.reported no significant difference at 6 months and 1 year in OS between single-dose SBRT or multiple sessions [9].However,a statistical trend toward prolonged OS was observed in patients with multiple fractions,with the most frequent in pancreatic adenocarcinoma.Moreover,the earlier studies of SBRT in pancreatic cancer used fractionation schemes with very high doses,single dose of 25 Gy,being discarded after the publication of the tolerance profile [10].Subsequently,moderate fractionation schemes with 3-5 fractions of 4-10 Gy have shown good tolerance and good disease control and have opened the possibility of improved outcomes in these patients,both in neoadjuvant treatment and with radical intent [11–13].Brunner et al.reported that local control was associated with high prescription doses [11].Despite this,the optimal dose has not yet been established.
SBRT indications
SBRT in pancreatic tumors is applicable in inoperable tumors due to comorbidities or patient refusal,in unresectable relapses,borderline or locally advanced as definitive treatment or with neoadjuvant intention.Adjuvant SBRT is possible,although the evidence is limited [14].
SBRT as neoadjuvant in pancreatic cancer
When the intent of treatment is neoadjuvant,the objective of treatment is to sterilize blood vessels allowing complete tumor resections with negative margins,decreasing the probability of local recurrence in initially unresectable patients,and increasing pathological complete responses.These factors are associated with increased local control [15].The risk of postoperative recurrence with chemotherapy alone ranges from 13%-33% and decreases to 7%-16%combined with CRT [16,17].Two clinical trials have demonstrated the benefit of neoadjuvant treatment compared to resection and adjuvant treatment in resectable and borderline resectable pancreatic cancer.However,the optimal neoadjuvant treatment is unclear,with significant variation between centers [18,19].
Data on local recurrence after neoadjuvant chemotherapy and SBRT are limited [20,21].The H.Lee Moffitt Cancer Center study included 73 patients with localized pancreatic cancer (57 borderline and 16 locally advanced) who received induction chemotherapy [gemcitabine,docetaxel and capecitabine (66%),gemcitabine alone (25%) or FOLFIRINOX (5%)]and SBRT in 5 fractions [22].Fiftysix percent of patients with borderline resectable tumors were operated with 97% R0 resections.Median OS in patients achieving R0 was significantly longer than in unresectable patients (19.3 vs.12.3 months,P=0.03).These treatments are well tolerated with no acute toxicity greater than or equal to grade 3 and only 5.3% of chronic gastrointestinal toxicity greater than or equal to grade 3.In the study by Mellon et al.,159 patients were included (110 borderline,49 locally advanced);of the 49 borderline patients,51% were operated on,achieving R0 resections in 97% of the patients and 7%showed complete pathological response [20].The median OS in resected patients was 34 months.Acute toxicity grade 3 or higher occurred in 2% and late toxicity in 5%.The Johns Hopkins study included 74 patients;15 patients with locally advanced pancreatic cancer were resected with R0 rates of 80% and 13% had complete pathologic responses with a median survival of 20.2 months [21].The recently published study by Xiang et al.[23]analyzed the role of neoadjuvant SBRT in resectable pancreatic cancer in 175 patients compared to 1335 patients treated with conventional CRT demonstrating better OS.The study included treatment schedules of 20-25 Gy in single dose or 30-50 Gy at 5 Gy per fraction.SBRT was associated with higher complete pathologic complete response rates and negative resection margin.
Another study by Mellon et al.analyzed predictors of survival after pathologic response in borderline resectable and locally advanced pancreatic cancer patients treated with neoadjuvant chemotherapy and SBRT,with preoperative positron emission tomography (PET) and carbohydrate antigen 19-9 (CA19-9) factors associated with histological regression [24].However,another study by Katz et al.found no correlation with CA19-9 levels,although the tumor regression scale was not used [25].Dholakia et al.found that metabolic tumor volume and total lesion glycolysis are correlated with OS in patients with locally advanced pancreatic cancer [26].
The Alliance for Clinical Oncology Trial A021501 randomized patients with borderline resectable pancreatic cancer to eight cycles of mFOLFIRINOX or seven cycles of mFOLFIRINOX and SBRT with neoadjuvant intent [27].However,the study has prematurely closed the experimental arm after including 30 patients in each arm.mFOLFIRINOX neoadjuvant was associated with favorable OS,but the addition of SBRT did not improve survival compared to classical series.This study has many limitations such as the heterogeneity of the sample,the difficulty in assessing response after SBRT,and the lack of power to measure OS,among others.The MASTERPLAN study,a phase II study that will evaluate locoregional control at 12 months in patients with potentially operable or inoperable pancreatic cancer,has been launched [28].
The use of neoadjuvant SBRT has not been associated with increased complications or postoperative mortality [29].
SBRT in definitive pancreatic cancer
SBRT has been studied as a definitive treatment.The study by Comito et al.[13]included 45 patients treated with 45 Gy in 6 fractions with a median follow-up of 13.5 months;progression-free survival (PFS) was 90% at 2 years.The median PFS and OS were 8 and 13 months,respectively.Seventy-one percent of locally advanced pancreatic adenocarcinomas received chemotherapy prior to SBRT.The median OS from diagnosis was 19 months.No toxicities greater than or equal to grade 3 were described.In the study by Shaib et al.[30],radiotherapy was shown to be better than no treatment in patients with unresectable locally advanced cancer.
The use of SBRT in metastatic pancreatic adenocarcinoma is increasing,with local progression being responsible for 30% of the deaths of these patients,impacting the quality of life because of the pain it causes [31].
Side effects are usually grade 2 and are highly dependent on the location of the tumor;the risk of gastritis in pancreatic head tumors is higher than that in pancreatic body or tail tumors.For SBRT in pancreatic cancer the distance between the tumor and the luminal organs such as the intestine and the stomach are fundamental.The use of spacers between the tumor and critical organs has been proposed to decrease the possibility of side effects [32].The most important studies of SBRT in pancreatic adenocarcinoma are summarized in Table 1 [20-22,33-44]including information of local control,doses and toxicities.

Table 1Studies of SBRT in pancreatic adenocarcinoma.
SBRT in local relapses
CRT has been used for the treatment of unresectable local relapses.Conventional radiotherapy appears to have insufficient local control due to limited tolerance of surrounding healthy organs.Habermehl et al.[45]analyzed 41 patients treated with CRT after local relapse.Local control at 1 year was 60% with a median OS of 16 months.In addition,about 50% of the patients had grade 3 toxicity.Wilkowski et al.[46]included 18 patients treated with chemotherapy and CRT,local control at 1 year was 70% and median OS was 14 months,with grade 3 toxicity for 50% of the patients.Nakamura et al.[47]included 30 patients treated with conventional radiotherapy,reporting 1-year OS,local control,and PFS of 69%,67%,and 32%,respectively.Median survival was 15.9 months,grade 3 gastrointestinal toxicity was observed in 7% of patients,with hematologic toxicity greater than or equal to grade 3 in 60%of patients.
The role of SBRT has also been studied in unresectable local relapses or after CRT.The study by Comito et al.[48]also included 31 patients treated with 45 Gy in 6 fractions.The median local recurrence was 14 months,median follow-up was 12 months,freedom from local progression was 91% and 82% at 1 and 2 years,median PFS was 9 months and median OS was 18 months.No grade 3 or higher toxicity was described.The study by Koong et al.reported the results of SBRT treatment for prior CRT treated patients,demonstrating it to be a feasible option with good local control and acceptable toxicity,especially in fractionated scheme [49].Wild et al.demonstrated a median survival of 8.8 months and a local PFS of 62% at 1 year in 15 patients [50].Local recurrences after>12 months of CRT are the most appropriate for re-irradiation.Overall grade 3 toxicity was 6%-8% [49–51].
Failure patterns after SBRT
Patterns of failure after neoadjuvant therapy with SBRT and chemotherapy have been studied.An autopsy study of operated patients showed 70%-80% local relapse exclusively or in combination with metastasis [52].Katz et al.[53]in their study described 13% local recurrence in resected patients treated with CRT.Dholakia et al.[54]evaluated 202 patients treated with or without radiotherapy;45% of the cases (90 patients) developed local failure.The authors generated a map of recurrences to evaluate the relationship with the superior mesenteric artery and the celiac trunk.Perivascular recurrences in resected pancreatic cancer are related to perineural spread by the autonomic nerves within the mesenteric vessels.The biology of neurotropism in pancreatic cancer is well documented [55,56].Pancreatic cancer has a high prevalence of perineural invasion approaching 100%.The authors conclude that an asymmetric expansion in treatment volumes of 1 to 3 cm should be used to cover this area of recurrence.However,there is variability among the radiotherapy scheme,dose,fractionation and treatment volumes and therefore,it is still not standardized.
Future prospects
SBRT is a radiotherapy technique that allows high doses of radiation to be delivered in a tumor-targeted manner.This characteristic makes it possible to limit the doses received by the surrounding healthy organs.The use of SBRT in cancer is becoming increasingly widespread in many locations;however,its role in pancreatic cancer is even more relevant.Radiotherapy in pancreatic cancer,due to its anatomical location,is not easy.Patients receiving conventional radiotherapy for pancreatic cancer have significant side effects due to the proximity of the healthy organs around this gland.The duodenum is located around the head of the pancreas,the site most affected by pancreatic adenocarcinoma.This means that conventional radiotherapy techniques do not allow the dose to the tumor to be increased,since the same dose would be received by the surrounding healthy organs.This is the first advantage of SBRT;thanks to the conformation of the technique,it allows high doses to be administered to the tumor while minimizing as much as possible the doses received by the duodenum or the stomach.For this reason,it is also possible to increase the dose intensity of each session and reduce the number of sessions,which has an impact on the quality of life of patients and facilitates the management of waiting lists in radiation oncology departments.
One of the main problems in the development of this technique is the low incidence of this tumor in the population,which means that recruitment for clinical trials is very slow and many trials are closed for this reason.There are no phase III studies.Another problem is the lack of human and technical resources for the development of the technique;it is a complex technique that requires training for its development and maintenance.In addition,the optimal dose and response evaluation systems are not yet fully defined.Systems are being investigated to separate the duodenum from the pancreatic head and further increase the dose to the tumor.
SBRT in the abdominal area is undergoing a major revolution.It is possible that SBRT will become the standard in pancreatic cancer patients who are candidates for radiotherapy,leaving CRT in the background.
In addition,the role of new drugs and their combination with SBRT are being studied,using the power of ablative doses on the immune system enhanced by immunotherapy drugs.This is likely to improve both local and systemic control of the disease.
The 5-year survival of pancreatic cancer is less than 20%.Some of the resectable patients progress in a short time,which makes us wonder if SBRT could be an alternative to surgery,with no hospital stay,no surgical risks,no comorbidities and no postoperative complications.It is therefore essential that this treatment be part of the therapeutic arsenal in resectable and unresectable disease,as neoadjuvant,in local relapse and even in adjuvant.
Conclusion
SBRT can be presented as an effective alternative for patients with pancreatic cancer,supported by clinical practice guidelines as it has demonstrated good tolerance and good disease control.SBRT opens a possibility of improving outcomes for these patients,both in neoadjuvant treatment and with radical intent.
Acknowledgments
None.
CRediT authorship contribution statement
Carolina de la Pinta:Conceptualization,Data curation,Formal analysis,Methodology,Writing– original draft,Writing– review &editing,
Funding
None.
Ethical approval
Not needed.
Competing interest
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- Recent advances in promising drugs for primary prevention of gastroesophageal variceal bleeding with cirrhotic portal hypertension
- Application of ultrasonography-elastography score to suspect porto-sinusoidal vascular disease in patients with portal vein thrombosis
- Polydatin ameliorates hepatic ischemia-reperfusion injury by modulating macrophage polarization
- Hypomethylation of glycine dehydrogenase promoter in peripheral blood mononuclear cells is a new diagnostic marker of hepatitis B virus-associated hepatocellular carcinoma
- AGK2 pre-treatment protects against thioacetamide-induced acute liver failure via regulating the MFN2-PERK axis and ferroptosis signaling pathway
- Circulating RNA ZFR promotes hepatocellular carcinoma cell proliferation and epithelial-mesenchymal transition process through miR-624–3p/WEE1 axis