Early systemic anticoagulation reduces hospital readmission in acute necrotizing pancreatitis patients: A retrospective cohort study
2024-03-04WenJianMaoJingZhouGuoFuZhangFaXiChenJingZhuZhangBaiQiangLiLuKeWeiQinLi
Wen-Jian Mao ,Jing Zhou ,Guo-Fu Zhang ,Fa-Xi Chen ,Jing-Zhu Zhang ,Bai-Qiang Li ,Lu Ke,c,Wei-Qin Li,c,∗
a Department of Critical Care Medicine, Jinling Hospital, Nanjing Medical University, Nanjing 210002, China
b Department of Critical Care Medicine, Jinling Hospital, Medical School of Nanjing University, Nanjing 210002, China
c National Institute of Healthcare Data Science, Nanjing University, Nanjing 210010, China
Keywords: Anticoagulation Splanchnic venous thrombosis Acute necrotizing pancreatitis Readmission Long-term outcomes
ABSTRACT Background: Early systemic anticoagulation (SAC) is a common practice in acute necrotizing pancreatitis(ANP),and its impact on in-hospital clinical outcomes had been assessed.However,whether it affects long-term outcomes is unknown.This study aimed to evaluate the effect of SAC on 90-day readmission and other long-term outcomes in ANP patients.Methods: During January 2013 and December 2018,ANP patients admitted within 7 days from the onset of abdominal pain were screened.The primary outcome was 90-day readmission after discharge.Cox proportional-hazards regression model and mediation analysis were used to define the relationship between early SAC and 90-day readmission.Results: A total of 241 ANP patients were enrolled,of whom 143 received early SAC during their hospitalization and 98 did not.Patients who received early SAC experienced a lower incidence of splanchnic venous thrombosis (SVT) [risk ratio (RR)=0.40,95% CI: 0.26-0.60,P < 0.01]and lower 90-day readmission with an RR of 0.61 (95% CI: 0.41-0.91,P=0.02) than those who did not.For the quality of life,patients who received early SAC had a significantly higher score in the subscale of vitality (P=0.03)while the other subscales were all comparable between the two groups.Multivariable Cox regression model showed that early SAC was an independent protective factor for 90-day readmission after adjusting for potential confounders with a hazard ratio of 0.57 (95% CI: 0.34-0.96,P=0.04).Mediation analysis showed that SVT mediated 37.0% of the early SAC-90-day readmission causality.Conclusions: The application of early SAC may reduce the risk of 90-day readmission in the survivors of ANP patients,and reduced SVT incidence might be the primary contributor.
Introduction
Acute pancreatitis (AP) is a common cause of hospitalization,with annual global prevalence ranging from 8 to 50 per 100 000 populations [1].About 5% to 20% of AP patients develop acute necrotizing pancreatitis (ANP),which can lead to local complications such as acute necrotizing collection (ANC),infected pancreatic necrosis (IPN),or gastric outlet obstruction,resulting in a prolonged disease course,poorer prognosis and increased rate of readmission after discharge [2,3].Readmission after the index discharge has become a significant healthcare concern in AP patients for a long time,with readmission rates ranging from 16.5% to 29% in previous studies [3–6].Therapies aiming to reduce readmission may improve the life quality of the discharged patients and decrease the burden on the healthcare system.
Splanchnic venous thrombosis (SVT),a common complication of ANP,mainly affects the portal vein (PV),splenic vein (SplV),and superior mesenteric vein (SMV) [7–9].It is associated with poorer clinical outcomes,prolonged hospital duration,and a lower quality of life [10,11].Furthermore,in patients with pancreatic exocrine cancer,cirrhosis,or solid organ transplant recipients [12–14],SVT has been linked to an increased risk of readmission,but no study in AP patients has been published yet.Early systemic anticoagulation (SAC) has been shown to reduce the incidence of SVT and improve clinical outcomes without increasing the risk of bleeding [15].However,its impact on long-term outcomes,like readmission in ANP patients,is unknown.
In this retrospective cohort study,we aimed to assess the effect of early SAC on readmission and other long-term events in ANP patients.
Methods
Ethics statement
This study was conducted using an electronic database (Acute Pancreatitis Database,AP Database).The establishment of the AP Database was approved by the Review Committee of Jinling Hospital (No: 2019NZKY-003-01).Routine informed consent was obtained for data collection,storage,and academic use from all patients or next of kin during hospitalization.
Study design and participants
Using the data extracted from the AP Database,a retrospective cohort study was conducted to evaluate the effect of early SAC on long-term events in ANP patients.Clinical data during hospitalization and follow-data in the AP Database were prospectively collected.Follow-up was implemented through telephone.From January 2013 to December 2018,patients with a primary diagnosis of AP complicated by pancreatic necrosis admitted to the Center of Severe Acute Pancreatitis,Jinling Hospital within 7 days from the onset of the disease were screened.Pancreatic necrosis was diagnosed according to the characteristic findings of AP on contrast-enhanced computed tomography (CECT): lack of pancreatic parenchymal and/or presence of peripancreatic necrosis [16].Patients with a length of hospitalization of more than 7 days were included.Patients who met the following criteria were excluded:(1) younger than 18 years or older than 70 years,(2) with precipitating factors for thrombosis (trauma,pregnancy,liver cirrhosis,intra-abdominal infections,pancreatic cancer,chronic pancreatitis),(3) with suspected active bleeding at admission,(4) with end-stage chronic disease,or (5) died during the index hospitalization.
Anticoagulation management in different periods
The majority of patients admitted between January 2013 and December 2014 did not receive early anticoagulant medication due to concerns of the risk of pancreatic/peripancreatic hemorrhage.From June 2015 to December 2018,the detrimental effects of deep venous thrombosis,SVT,and pulmonary embolism were better understood,and the risk of bleeding was reassessed.Therefore,most patients received early SAC at the treating physician’s discretion.The period from January to May 2015 was a transition phase during which the practice gradually altered.All the enrolled patients were managed by the same treating team throughout the entire study period in light of the international guidelines [17].
Definition of early systemic anticoagulation
Early SAC was defined when low-molecular-weight heparin(LMWH) (410 0,5000,820 0 or 1000 0 IU) or argatroban (10 or 20 mg) was initiated at the early phase of AP (<7 days from onset of abdominal pain) and administered daily for at least 7 consecutive days after admission.The dosage of anticoagulants was decided by the treating physician depending on the body weight of the patients and the estimated risk of bleeding.No other anticoagulants or dose regimens were used during the study period.To monitor the coagulation status,we used routine indices like prothrombin time (PT),activated partial thromboplastin time (APTT),international normalized ratio (INR),and thromboelastogram (TEG)to ensure the safety of anticoagulation therapy.Once the risk of bleeding outweighed the potential benefits of anticoagulation,anticoagulant drugs would be withdrawn at the treating physician’s discretion.
Study outcome measures
The primary outcome was 90-day readmission,defined as unplanned readmission to the hospital within 90 days of discharge from the index admission.Readmission within 72 h of discharge was counted as the same admission.
Secondary outcomes were other post-discharge events,including 30-day readmission,1-year return to work,quality of life evaluated by the 36-item Short-Form Health Survey (SF-36) at the last follow-up,new-onset diabetes mellitus,steatorrhea and mortality during the one-year follow-up.
Data collection and definitions
Data were extracted from the AP Database,including age,sex,body mass index,pre-existing chronic diseases,etiology of AP,severity,and clinical outcomes during the index hospitalization.The definitions of clinical outcomes,including SVT,SVT-related complications,organ failure,and bleeding,were detailed in the previous study [15].Besides,the diagnosis of IPN was made when one or more of the following criteria were present: gas bubbles within pancreatic/peripancreatic necrosis on CT;a positive culture from pancreatic and/or peripancreatic necrosis obtained by fineneedle aspiration,catheter drainage,or necrosectomy according to the latest guidelines [16].The gastrointestinal fistula was defined as pathological communications that connect any portion of the gastrointestinal tract with the necrotic cavity,the peritoneal space,the retroperitoneal areas,or another internal organ based on fistulography,digestive endoscopy,or operative findings [18].
All survivors were contacted by phone during the one-year follow-up period once every three months.Quality of life assessment was implemented using remote questionnaire interviews.The questionnaire included SF-36 and a record of return to work at follow-up.Readmission,new-onset diabetes mellitus,steatorrhea,and all-cause mortality were recorded.
Statistical analysis
Continuous data were reported as means and standard deviations or as medians and interquartile ranges as appropriate,depending on their normality.The normality of data was determined by Kolmogorov-Smirnov tests.Student’st-test or Mann-WhitneyUtest was adopted to compare continuous variables.Categorical data were expressed as frequencies and percentages.The comparison of categorical data between the two groups was performed using Chisquare test or Fisher’s exact test.
The role of early SAC in reducing 90-day readmission was evaluated by the Kaplan-Meier method and was compared using the log-rank test.Cox proportional-hazards regression model was employed to analyze potential risk factors for primary outcome (P<0.2) with three priori variables [age,sex and acute physiology and chronic health evaluation II (APACHE II) score at admission]as covariates.The hazard ratio (HR) and its 95% confidence interval (CI) were calculated.In addition,to help account for the nonrandomized treatment administration of early SAC,we used propensity-score methods to reduce confounding effects.The individual propensities for receipt of early SAC treatment were estimated using multivariable logistic regression model that included the same covariates as the Cox regression model.Associations between early SAC use and 90-day readmission were then estimated by multivariable Cox regression models using three propensity-score methods,including inverse probability weighting,propensity-score matching,and adding the propensity score as an extra covariate.
As for the mediation analysis,we used a bootstrapping resampling with 1000 resamples to assess the indirect effects of SVT on early SAC and 90-day readmission.Point estimates and 95% CIs were estimated for indirect and direct effects.The proportion of the effect of the independent variable on the dependent variable that went through the mediator was estimated for mediation.
Statistical tests were two-sided,andPvalues<0.05 were deemed significant unless otherwise stated.All statistical analyses were done in the SPSS 26.0 software (SPSS Inc.,Chicago,IL,USA) and the R 4.1.1 software (Lucent Technologies,Inc.,Murray Hill,New Jersey,USA).
Results
Characteristics of the study population
A total of 241 patients were enrolled for analysis with a median age of 42 years,66.8% male and 39.8% hyperlipidemia AP.Among them,143 patients received early SAC during hospitalization,while 98 did not (Fig.1).Table 1 shows the demographic and baseline clinical characteristics of these patients.The two groups were largely balanced in terms of demographic and clinical characteristics except for types of antibiotics used and renal failure at admission (Table 1).

Table 1Demographic and clinical characteristics in patients with early systemic anticoagulation.
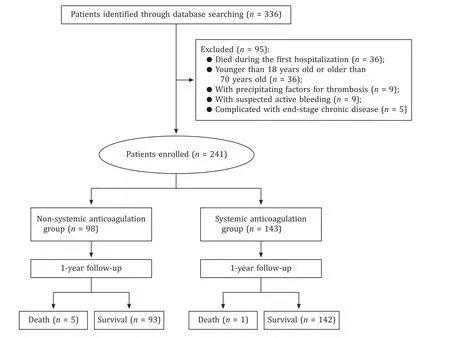
Fig.1. Flow chart.
Clinical outcomes during the index hospitalization are shown in Table S1.Compared to non-SAC patients,the incidence of SVT was lower in patients who received early SAC (18.2% vs.45.9%) with a risk ratio (RR) of 0.40 (95% CI: 0.26-0.60,P<0.01).SVT-related complications,including persistent ascites,enteral nutrition intolerance,and variceal bleeding,were comparable between groups.Other complications,including IPN,gastrointestinal fistula,abdominal bleeding and new-onset organ failure,were also comparable(Table S1).
Post-discharge events and life quality
During the 1-year follow-up,the patients who received SAC had a lower 90-day readmission rate (22.4% vs.36.7%) with a RR of 0.61(95% CI: 0.41-0.91,P=0.02).Moreover,the incidence of 30-day readmission,1-year return to work,new-onset diabetes mellitus and steatorrhea were not significantly different between the two groups (Table 2).

Table 2Long-term clinical outcomes of the study patients.
For the quality of life,SF-36 results were obtained in 44 patients (44.9%) in the non-SAC group and 81 patients (56.6%) in the early SAC group.Patients who received early SAC had a significantly higher score in the subscale of vitality (P=0.03),while the other subscales were all comparable between the two groups(Fig.2).
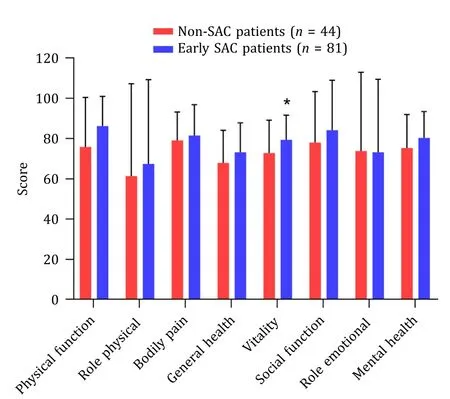
Fig.2. Quality of life measured by the SF-36 questionnaire.∗: P < 0.05,compared with non-SAC patients.Role physical denotes physical health problems with work or other regular daily activities.Bodily pain denotes the severity and frequency of bodily pain during the past 4 weeks.Role emotional denotes emotional health problems with work or other regular daily activities.
The primary reasons for 90-day readmission are shown in Table S2.In patients who received early SAC,persistent fever due to suspected infection (31.3%) was the most frequent one.In comparison,aggravation of abdominal distension (44.4%) was the most common in non-SAC patients.The distribution of primary reasons for 90-day readmission was significantly different between the two groups (overallP=0.04).Moreover,12 patients (12.2%) in the non-SAC group had new-onset organ failure at readmission,while 14 patients (9.8%) in the SAC group had that (Table S3).
Role of early SAC in 90-day readmission
The Kaplan-Meier curves for the cumulative incidence of readmission within 90 days after discharge are shown in Fig.3.The probability of readmission occurrence was significantly lower in patients who received early SAC (log-rankP=0.023).In multivariable Cox regression analysis adjusted for age,sex,APACHE II score at admission,pre-existing hypertension,renal failure,respiratory failure at admission and use of antibiotics,early SAC remained a significant factor affecting 90-day readmission (HR=0.57,95% CI:0.34-0.96,P=0.04) (Table 3).Additional multivariable propensityscore analyses yielded similar results (Table S4),and the balances of the covariates after propensity score matching or inverse probability weighting are shown in Fig.S1.

Table 3Multivariable Cox regression in predicting late readmission during 90 days after discharge.

Fig.3. Kaplan-Meier curves of 90-day readmission in the early SAC and non-SAC patients.SAC: systemic anticoagulation.
The result of mediation analysis showed that SVT mediated 37.0% of the early SAC-90-day readmission causality (mediation effect=-0.05;95% CI:-0.10 to-0.01,P=0.02) (Fig.S2).
Discussion
In the present study,our data suggested that the use of early SAC was associated with a lower risk of 90-day readmission in a cohort of ANP patients.The main reason might be attributed to the reduced SVT,resulting in a lower incidence of post-discharge abdominal distension aggravation,a typical symptom of SVT.
SVT is prevalent in ANP patients,with a frequency of up to 50%,mainly due to peripancreatic inflammation involvement of the vessels [9,19].SVT-related symptoms may significantly affect shortterm outcomes,but their impact on long-term events after discharge has not been thoroughly studied.In a retrospective study published in 2021,Robbins et al.demonstrated that 6.5% of AP patients who developed venous thromboembolic events (pulmonary embolism,deep vein thrombosis,or mesenteric vessel thrombosis)had more readmissions [20],but the relationship between SVT and readmission was not assessed separately.Furthermore,SVT was frequently reported as one of the risk factors for readmission in various diseases [13,14,21].In this study,we found that early SAC was associated with decreased 90-day readmission,and SVT acted as a mediating effect factor between them,implying that the potential benefit of early SAC in ANP patients might be mediated by reducing SVT.
In current clinical guidelines of AP,SAC was not recommended during the acute phase concerning the risk of bleeding,though its efficacy and safety had been reported in several studies [15,22,23].As shown in our previous study,early SAC could reduce the incidence of SVT and its related symptoms during the index hospitalization [24],including variceal bleeding,persistent ascites and enteral nutrition (EN) intolerance.In the present study,aggravation of abdominal distension (44.4%) was the most frequent reason for 90-day readmission,and abdominal discomfort was a typical self-reported symptom of SVT patients caused by various diseases [25,26].The results demonstrated that SVT-related consequences might be a major contributor to readmission in ANP patients,which is in line with the results of the mediation analysis.Moreover,although there are more patients in the SAC group readmitted due to new-onset organ failure as the primary reason,the overall incidence at readmission was comparable between the two groups,suggesting that SAC may not be associated with postdischarge organ failure.
For the quality of life,though only half of the studied patients completed the SF-36 health survey,we found that patients who received early SAC had a significantly higher score in the subscale of vitality,which is similar to the result of a meta-analysis in patients after AP episodes [27].The vitality domain of the SF-36 is used to assess whether the patients are fatigued,which is associated with the degree of ascites and abdominal pain in cirrhosis and postoperative patients [28–30].To our knowledge,the association between vitality and SVT has not been reported in previous studies,and the lower vitality might partly result from SVT-related symptoms,potentially leading to malnutrition or weakness after discharge.
Hospital readmission represents a significant burden to the individual patient and the health care system,and some might be preventable.This study found that readmission (28.2%) within 90 days of hospital discharge among ANP patients is common,whereas data from the previous studies revealed an even greater rate of unplanned readmission (up to 70%) among them [31,32],though their time to readmission was not given.Future prospective studies are needed to verify the benefits of early SAC in ANP,with readmission rate,abdominal discomfort and quality of life included as outcome metrics.Moreover,all necrotizing pancreatitis cases reported in this study were caused by non-medical etiologies.Because of the differences in pathogenesis,whether AP patients caused by iatrogenic etiologies like endoscopic ultrasoundguided interventions [33]or diagnostic procedures [34]could benefit from early SAC without safety problems can not be demonstrated by our results.
There were some limitations in our research.First,it was a single-center retrospective cohort research.Furthermore,changes in general treatment over time in our center were likely to affect the results,and we did not have a uniform protocol for initiating,monitoring,or withdrawing anticoagulants during the study period,both of which may introduce bias.Moreover,a unique feature of this cohort is that hypertriglyceridemia-associated AP accounts for approximately 40% of the study subjects,which is common in Chinese AP cohorts [35].Although the etiology distribution did not differ between patients who received early SAC or not,this feature may limit the generalizability of the observed results.Last,treatment and selection variability cannot be avoided,as the duration and intensity of SAC are determined by the treating physician.A randomized controlled trial with rigorous eligibility criteria and a pre-determined SAC regimen is therefore justified to confirm our findings.
The application of early SAC is associated with reduced incidence of readmission and improved quality of life in ANP patients and the potential benefit of early SAC might be mediated by reducing the incidence of SVT.A future randomized trial with sufficient power is warranted to confirm our findings.
Acknowledgments
None.
CRediT authorship contribution statement
Wen-Jian Mao:Data curation,Formal analysis,Validation,Writing– original draft.Jing Zhou:Data curation,Funding acquisition.Guo-Fu Zhang:Data curation,Validation.Fa-Xi Chen:Data curation.Jing-Zhu Zhang:Data curation.Bai-Qiang Li:Conceptualization,Supervision,Writing– review &editing.Lu Ke:Conceptual-ization,Funding acquisition,Methodology,Supervision,Writing–review &editing.Wei-Qin Li:Conceptualization,Supervision,Writing– review &editing.
Funding
This study was supported by grants from the National Natural Science Foundation of China (82070665 and 81900592).
Ethical approval
This study was conducted using an electronic database (Acute Pancreatitis Database,AP Database).The establishment of the AP Database was approved by the Review Committee of Jinling Hospital (No: 2019NZKY-003-01).Written informed consent was obtained from all participants.
Competing interest
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Supplementary materials
Supplementary material associated with this article can be found,in the online version,at doi: 10.1016/j.hbpd.2023.04.003.
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- Recent advances in promising drugs for primary prevention of gastroesophageal variceal bleeding with cirrhotic portal hypertension
- Stereotactic body radiotherapy in pancreatic adenocarcinoma
- Application of ultrasonography-elastography score to suspect porto-sinusoidal vascular disease in patients with portal vein thrombosis
- Polydatin ameliorates hepatic ischemia-reperfusion injury by modulating macrophage polarization
- Hypomethylation of glycine dehydrogenase promoter in peripheral blood mononuclear cells is a new diagnostic marker of hepatitis B virus-associated hepatocellular carcinoma
- AGK2 pre-treatment protects against thioacetamide-induced acute liver failure via regulating the MFN2-PERK axis and ferroptosis signaling pathway