Low skeletal muscle mass and high visceral adiposity are associated with recurrence of acute cholecystitis after conservative management:A propensity score-matched cohort study
2024-03-04YudaiKoyaMihihikoShiataYukiMarunoYoshitakaSakamotoShinjiOeKoihiroMiyagawaYuihiHonmaMasaruHarada
Yudai Koya ,Mihihiko Shiata ,Yuki Maruno a, ,Yoshitaka Sakamoto ,Shinji Oe ,Koihiro Miyagawa ,Yuihi Honma ,Masaru Harada
a Department of Gastroenterology, Kyushu Rosai Hospital, Moji Medical Center, 3-1 Higashiminatomachi, Moji-ku, Kitakyushu 801-8502, Japan
b Third Department of Internal Medicine, School of Medicine, University of Occupational and Environmental Health, Kitakyushu 807-8555, Japan
c Department of Surgery, Kyushu Rosai Hospital Moji Medical Center, Kitakyushu 801-8502, Japan
Keywords: Acute cholecystitis Low skeletal muscle mass Recurrent acute cholecystitis Sarcopenia Visceral adiposity
ABSTRACT Background: Recurrent acute cholecystitis (RAC) can occur after non-surgical treatment for acute cholecystitis (AC),and can be more severe in comparison to the first episode of AC.Low skeletal muscle mass or adiposity have various effects in several diseases.We aimed to clarify the relationship between RAC and body parameters.Methods: Patients with AC who were treated at our hospital between January 2011 and March 2022 were enrolled.The psoas muscle mass and adipose tissue area at the third lumbar level were measured using computed tomography at the first episode of AC.The areas were divided by height to obtain the psoas muscle mass index (PMI) and subcutaneous/visceral adipose tissue index (SATI/VATI).According to median VATI,SATI and PMI values by sex,patients were divided into the high and low PMI groups.We performed propensity score matching to eliminate the baseline differences between the high PMI and low PMI groups and analyzed the cumulative incidence and predictors of RAC.Results: The entire cohort was divided into the high PMI (n=81) and low PMI (n=80) groups.In the propensity score-matched cohort there were 57 patients in each group.In Kaplan–Meier analysis,the low PMI group and the high VATI group had a significantly higher cumulative incidence of RAC than their counterparts (log-rank P=0.001 and 0.015,respectively).In a multivariate Cox regression analysis,the hazard ratios of low PMI and low VATI for RAC were 5.250 (95% confidence interval 1.083–25.450,P=0.039) and 0.158 (95% confidence interval: 0.026-0.937,P=0.042),respectively.Conclusions: Low skeletal muscle mass and high visceral adiposity were independent risk factors for RAC.
Introduction
Acute cholecystitis (AC) is a common disease encountered in various clinical settings with an estimated prevalence of 20% in patients with symptomatic gallstones [1].Age (50s to 60s),female sex,obesity,pregnancy or fertility,and drugs (fibrate,ceftriaxone,hormone preparations,and gallbladder motility inhibitors) are risk factors for gallstone disease [2,3].According to the updated Tokyo Guideline 2018 (TG18),treatment of AC should be decided according to the grade of severity [4].Although early laparoscopic cholecystectomy is recommended for grade I (mild) [5],conservative managements are often selected when considering the age,general condition,and comorbidities.Unless cholecystectomy is performed,there is a risk of recurrent AC (RAC),and RAC can be more severe and fatal than the first AC episode [6].Numerous studies have investigated the risk factors for gallstone disease and AC.However,the risk of RAC is not well understood.Age,disease severity,patient morbidity,previous antibiotic treatment duration,and history or presence of other biliary diseases are thought to be predictors of RAC [6–9].
Sarcopenia is characterized by the progressive and systemic depletion of skeletal muscle mass and strength,leading to disability,decreased quality of life,and a poor prognosis [10].According to the revised diagnostic criteria for sarcopenia,muscle strength is the main parameter.However,a loss of skeletal muscle mass is still required for a definitive diagnosis [11].The psoas muscle mass index (PMI) is an established and versatile method for evaluating skeletal muscle mass [12].Low PMI is reportedly an independent risk factor for recurrent biliary obstruction after self-expandable metallic stent placement in patients with malignant biliary obstruction [13].The mechanism seems to be an increase of sludge or debris inside the stent caused by sarcopenia-induced gallbladder motility impairment [14].Therefore,we assumed that RAC may also be precipitated by the impairment of gallbladder motility in patients with low skeletal muscle mass.
Obesity,especially visceral obesity,is strongly associated with an increased risk of AC or gallstone disease [15,16].A simultaneous evaluation of skeletal muscle mass and obesity is imperative in patients with AC;however,the relationship between these parameters and RAC remains unclear.
This study investigated the relationship between RAC and body composition on computed tomography (CT) and assessed the impact of body composition on RAC after non-surgical treatments.
Methods
Study design and subjects
This single-center retrospective cohort study was approved by the Ethics Committee of Kyushu Rosai Hospital Moji Medical Center (No: 04-01;date of approval: June 2,2022).This study was conducted in compliance with the principles of theDeclarationofHelsinki.The need for informed consent was waived due to the retrospective nature of the study.All patients with AC who were seen at our hospital between January 2011 and March 2022 and who had received non-surgical treatment for AC were included in this study.AC was diagnosed according to TG18 [4].The exclusion criteria were as follows: (1) AC with gallbladder carcinoma;(2) RAC during the first admission;(3) RAC due to percutaneous transhepatic gallbladder drainage (PTGBD) tube obstruction;(4) RAC due to high-fat diet;and (5) incomplete data.
Body composition evaluation, index calculation, and grouping
Body indices were calculated using abdominal CT images obtained during the first AC episode.Bilateral psoas muscle mass and visceral and subcutaneous adipose tissue masses at the third lumbar level were identified on CT images.The psoas muscle area(cm2) was measured using manual tracing.The visceral and subcutaneous adipose tissue areas (cm2) at the same level were measured using the Volume Analyzer Synapse VINCENT 3 image system (Fujifilm Medical,Tokyo,Japan).Fat was quantified in the range of-200 to-50 HU.The areas were divided by the squaredheight (m2).Subsequently,the visceral adipose tissue index (VATI),subcutaneous adipose tissue index (SATI),and PMI (cm2/m2) were calculated [17].According to the median VATI,SATI,and PMI values for each sex,the patients were divided into the low and high groups for each index.
Clinical factors
All clinical data were obtained by reviewing medical records.Clinical factors,such as age,sex,severity of AC according to the TG18 [4],American Society of Anesthesiologists Physical Status(ASA-PS) classification [18],age-adjusted Charlson comorbidity index (aCCI) [19],comorbidities,initial treatment and laboratory data,coexistence of common bile duct stones,gallstones,and the administration of antilipidemic agents were investigated at the first AC episode.Since most patients were accompanied by an excess of upper normal limits of laboratory data including inflammatory responses and hepatobiliary enzymes,we adopted each median values as cut-off values and incorporated into statistics.The rule applied to all laboratory data.Thirty-day mortality,days of fasting,parenteral antibiotics,and length of hospital stay were also assessed.Changes in the severity,treatment,and observational days were compared between the first AC episode and RAC.
Drainage procedure and antibiotics therapy
After making an AC diagnosis and evaluating severity grade of AC according to TG18,conservative management were selected in patients with surgically high risk and in patients who desired nonsurgical treatments.The conservative managements include intravenous antibiotics therapy and gallbladder drainage.Antibiotics were in all patients with AC,with or without drainage,and primarily included tazobactam/piperacillin,sulbactam/cefoperazone,and meropenem.PTGBD was performed using 18-to 21-gauge needles under local anesthesia.If necessary,a 7-Fr PTGBD tube was inserted and aspiration was performed.Transpapillary drainage of the gallbladder was performed using endoscopic retrograde cholangiopancreatography,and an internal or external 5-to 6-Fr stent was inserted into the gallbladder.Patients who received transpapillary drainage,and who received both percutaneous transhepatic and transpapillary drainage were categorized as other treatment group in tables,considering its small number.
Outcome measures and definitions
The occurrence of RAC was an event of interest.RAC was defined as a new episode of AC occurring after the clinical resolution of the symptoms with normal laboratory values during the first AC admission [6].All patients were observed from the day of remission of the first AC episode until the following time points: (1) onset of RAC;(2) day of elective cholecystectomy;or (3) last day of survival or death without RAC.The end of follow-up was July 19,2022.
Statistical analysis
Baseline characteristics at the first AC episode were compared between the high and low PMI groups.The Chi-square test was used to compare categorical variables.Continuous variables with a normal distribution were expressed as mean ± standard deviation and were compared using Student’st-test;those without a normal distribution were expressed as median with ranges and were compared using Mann–WhitneyUtest.We conducted propensity score matching to reduce the differences in clinical factors at baseline between the high PMI and low PMI groups.Using binomial logistic regression analysis,the propensity scores were estimated for patients with low PMI values.Variables used in the model included age,sex,initial treatment,body mass index (BMI),coexistence of common bile duct (CBD) stones,and administration of antilipidemic agents.We performed caliper matching of propensity scores.Pairs on the propensity score logit were matched within the standard deviation range of 0.2.The cumulative incidence of RAC was analyzed in each of the divided index groups using the Kaplan–Meier method and compared using a logrank test.Hazard ratio (HR) and 95% confidence interval (CI) for RAC were determined using univariate and multivariate Cox regression analyses.Each continuous variable was categorized into 2 groups based on the median value.Variables withPvalues<0.2 in univariate analysis were included in multivariate analysis.All analyses were performed using EZR (Saitama Medical Center,Jichi Medical University,Saitama,Japan),which was a graphical user interface for R (The R Foundation for Statistical Computing,Vienna,Austria) [20].Pvalues<0.05 were considered statistically significant.
Results
Baseline characteristics of the entire and propensity score-matched cohorts
Among 216 patients with AC who received conservative management,161 who met the eligibility criteria were included in the present study (Fig.1).The baseline characteristics of the patients during the first AC episode are shown in Table 1.The cut-off values for PMI,VATI,and SATI were separately estimated for men and women based on the median of each group.The cut-off values for PMI,VATI,and SATI were 4.98,62.2,and 33.9 cm2/m2,respectively,in men,and 4.01,51.6,and 59.8 cm2/m2,respectively,in women.There was 81 patients in the high PMI group and 80 patients in the low PMI group.After propensity score matching,no significant differences were observed in the baseline characteristics of the high PMI and low PMI groups,except for the occurrence of RAC (Table 1).In the entire and propensity score-matched cohorts,RAC was significantly more common in the low PMI group than in the high PMI group (P<0.001).
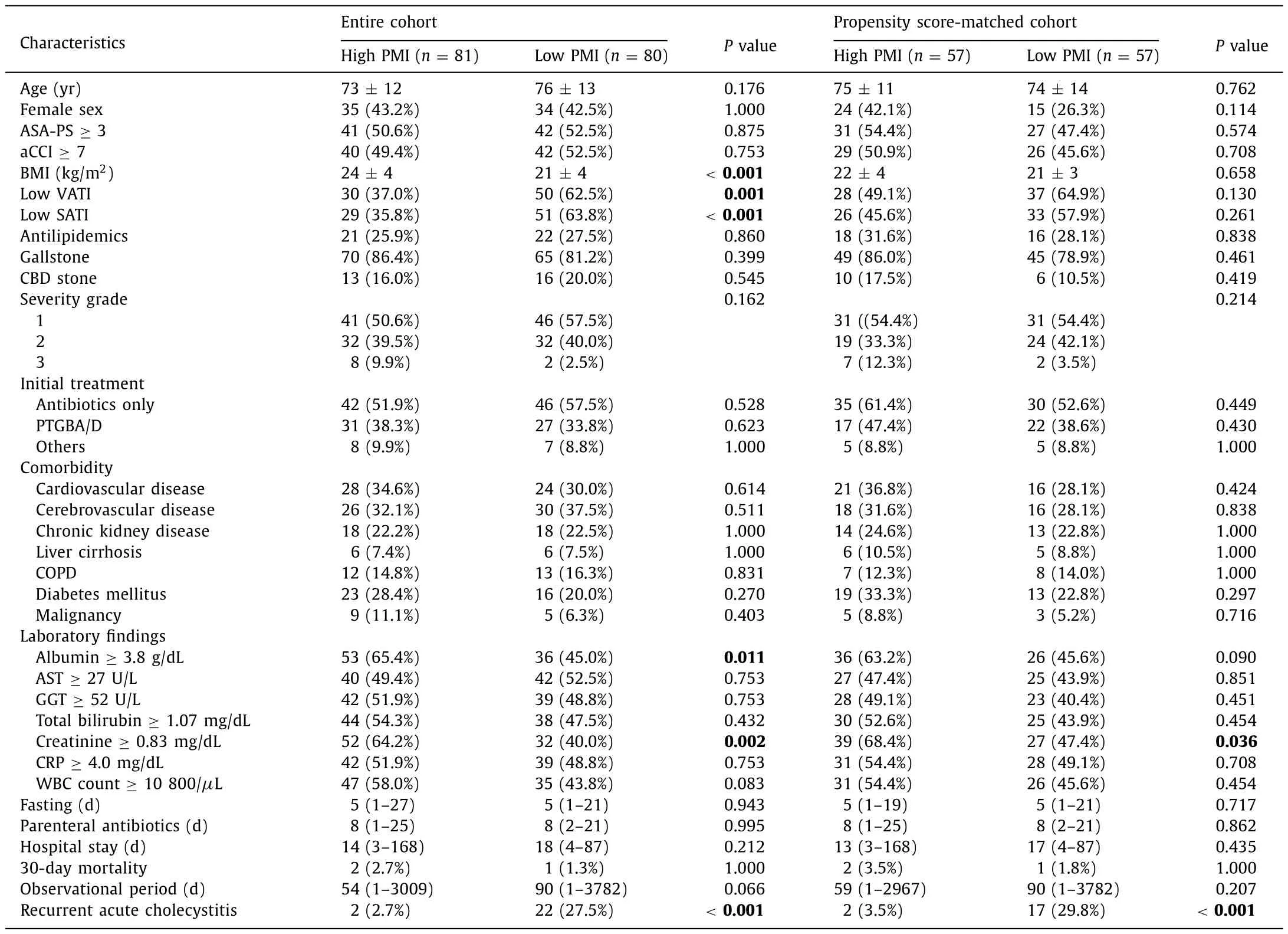
Table 1Baseline characteristics at first episode of acute cholecystitis.
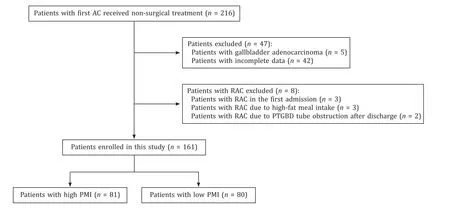
Fig.1. Flow chart of patient inclusion.AC: acute cholecystitis;PMI: psoas muscle mass index;PTGBD: percutaneous transhepatic gallbladder drainage;RAC: recurrent acute cholecystitis.
Cumulative incidence of RAC in the propensity score-matched cohort
RAC was observed in 19 (16.7%) patients in the propensity score-matched cohort.The median time-to-RAC was 90.5 days.In the Kaplan–Meier analysis,the 60-,180-,and 360-day cumulative incident rates of RAC were 2.0%,2.0%,and 2.0%,respectively in the high PMI group,and 9.4%,29.6%,and 37.0%,respectively,in the low PMI group (log-rankP=0.001) (Fig.2 A).A high incidence of RAC was also observed in the high VATI group,in which the 60-,180-,and 360-day cumulative incident rates were 12.9%,27.8%,and 32.6%,respectively.The 60-,180-,and 360-day cumulative incident rates in the low VATI group were 0,9.9%,and 14.2%,respectively(log-rankP=0.015) (Fig.2 B).Neither BMI (Fig.2 C) nor SATI (not presented) was significantly associated with RAC occurrence.
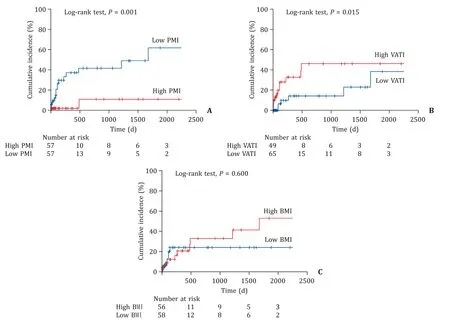
Fig.2. The cumulative incidence of RAC in the propensity score-matched cohort (Kaplan–Meier analysis).A: The cumulative incidence of RAC in the high (red line) and low(blue line) PMI groups;B: the cumulative incidence of RAC in the high (red line) and low (blue line) VATI groups;C: the cumulative incidence of RAC in the high (red line)and the low (blue line) BMI groups.BMI: body mass index;PMI: psoas muscle mass index;RAC: recurrent acute cholecystitis;VATI: visceral adipose tissue index.
Risk factors for RAC in the Cox regression analysis
We used univariate Cox regression analysis to identify factors associated with RAC,and thePvalues for sex,BMI,PMI,VATI,SATI,severity,and serum albumin were all<0.2 (Table 2).These factors were included in the multivariate models.Multivariate analysis revealed that low PMI was an independent predictor of RAC(HR=5.250,95% CI: 1.083–25.450,P=0.039).A low VATI was independently associated with a low risk of RAC (HR=0.158,95%CI: 0.026–0.937,P=0.042) (Table 2).
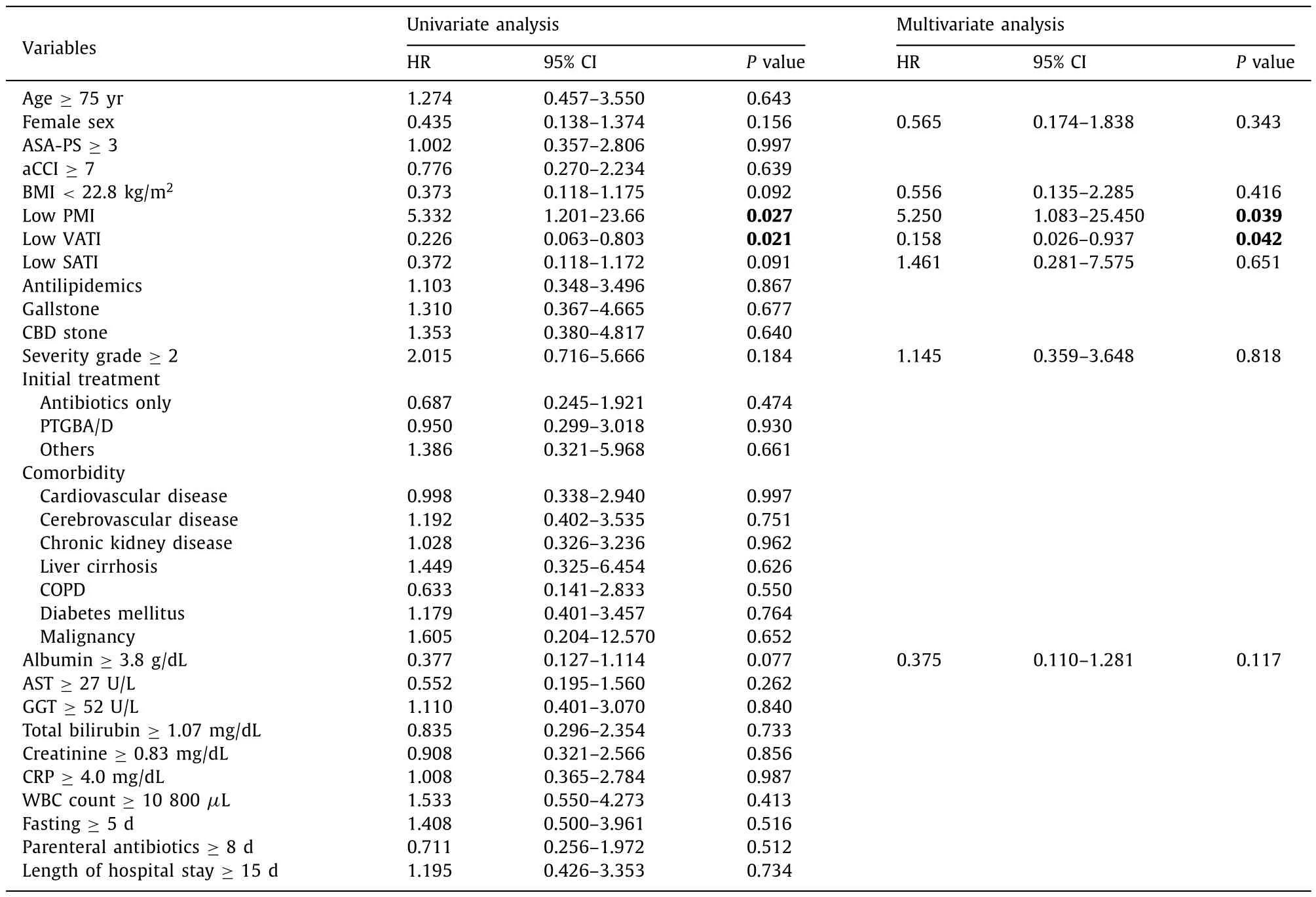
Table 2Cox regression analysis of baseline factors associated with recurrent acute cholecystitis in the propensity score-matched cohort.
Characteristics of RAC
A comparison between the first AC episode and RAC is shown in Table 3.RAC was significantly more severe than the first AC episode (P=0.003).Among the nine patients with severe RAC,four developed pericholecystic abscess or biliary peritonitis with severe organopathy,and two patients died within 30 days due to RAC.No differences were observed in the duration of fasting,antibiotic treatment,or hospital stay.Cholecystectomy was performed in 3 patients (12.5%) with RAC.
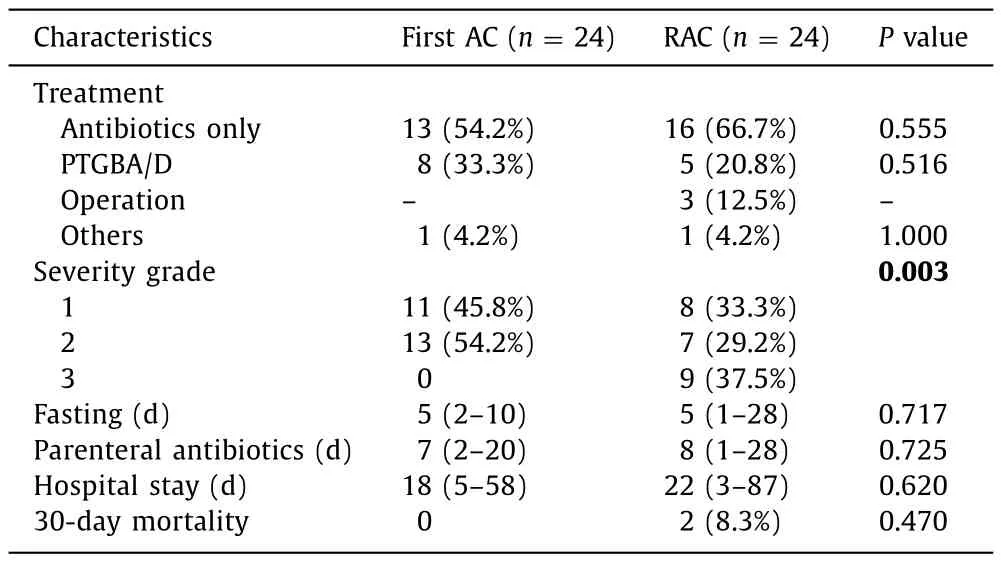
Table 3Comparison of the characteristics of RAC and the first AC episode.
Discussion
Recent improvements in health conditions have extended life expectation,leading to an increase in the aging population.Although performing cholecystectomy in patients with AC prevents further episodes of gallstone-related diseases,including RAC,conservative management outcomes for AC in high-risk older patients are reportedly similar to cholecystectomy in terms of mortality and cumulative major complications [21].Conservative treatments were chosen as the first-line therapy for high-risk older patients with AC.
The risk of RAC was maintained in these patients.The incident rate of RAC in patients waiting for index cholecystectomy is approximately 2.5%–22% [22,23].The incidence of RAC in the present study was 14.9%,which was comparable to that reported in previous studies.RAC is more severe than the first AC episode [6],which is also seen in the present study.Although there are no differences in the mortality,fasting duration,antibiotic treatment,or length of hospital stay,the prevention of RAC is important because exacerbation of the severity can lead to a poor prognosis.
Among 541 healthy living donors for liver transplantation,Hamaguchi et al.proposed PMI cut-off values (6.36 cm2/m2in men and 3.92 cm2/m2in women) as diagnostic criteria for low skeletal muscle mass [12].Applying this cut-off values to the present study,especially in men,majority of patients were classified into the low PMI group.In the present study,78% of patients were over 65 years old having several comorbidities,which suggests that most of patients already had a primary and secondary sarcopenia.Therefore,we had to define original cut-off values of PMI in these populations.
This study is the first to establish that low skeletal muscle mass and high visceral adiposity are independent risk factors for RAC.Low skeletal muscle mass is a major component of frailty,and frail patients have low physical activity.Additionally,frailty is associated with impaired gallbladder motility [14].The impairment may be attributable to decreased gallbladder sensitivity to cholecystokinin owing to the reduction in gallbladder cholecystokinin receptors,thereby resulting in the increase of gallstone formation [24].Furthermore,plasma cholecystokinin levels are relatively increased in patients with sarcopenia due to a reduction in cholecystokinin receptors [14,25].Plasma cholecystokinin elevation induces loss of appetite and accelerates sarcopenia and gallbladder contraction impairment.RAC could be induced by decreased gallbladder motility and increased prevalence of gallstones in patients with sarcopenia;however,gallstone disease was not an independent risk factor for RAC in the present study.
Propensity score matching was performed by considering each variable,including BMI.VATI,but not BMI or SATI,was significantly associated with RAC occurrence.VATI therefore is a newfound risk factor for RAC.Sekine et al.reported that abdominal visceral fat accumulation,but not subcutaneous fat accumulation,was associated with an increased risk of gallstone disease,even in patients with a BMI<25 kg/m2[15].Additionally,cholecystokinin response sensitivity might be decreased due to insulin resistance-induced hyperinsulinemia.Visceral adiposity is a strong determinant of insulin resistance,resulting in gallbladder dysmotility and enhanced gallstone formation [15,16].Visceral obesity and metabolic syndrome also induce acalculous “steatocholecystitis” in addition to an increased incidence of gallstone disease [16].They lead to fatty infiltration and enhanced inflammation of the gallbladder wall,which results in an abnormal wall structure and dysmotility [16,26].Gallbladder dysmotility owing to the loss of membrane cholecystokinin-receptor function is caused by increased membrane cholesterol content [27].Low skeletal muscle mass and high visceral adiposity may decrease the quantity and quality of cholecystokinin receptors,which also induces gallbladder dysmotility,resulting in RAC,irrespective of the presence or absence of gallstone disease.The findings of the present study suggest that patients with low skeletal muscle mass and high visceral adiposity have the highest risk of developing RAC.Poggiogalle et al.reported that sarcopenic obesity was associated with an increased impairment of insulin sensitivity and glycemic control when compared to patients with sarcopenia or obesity alone [28].Skeletal muscle plays a key role in insulin-mediated glucose disposal and myokine secretion,and thus,muscle loss can impair insulin sensitivity [29].Although the mechanisms of insulin resistance due to low skeletal muscle mass differ from those of high visceral adiposity,the co-occurrence of both conditions may lead to the onset of strong insulin resistance,which can eventually lead to crucial gallbladder dysmotility.As these mechanisms are not fully understood yet,further investigation is required.
Diabetes mellitus was not an independent risk factor for RAC in the present study,although insulin resistance leads to gallbladder dysmotility.Diabetes is significantly associated with the development of gallstone diseases,especially in female patients [30].In our propensity score-matched cohort,the majority of participants (65%) were male,which might have affected our results.
The present study has some limitations.First,it was a singlecenter study and the sample size was small especially in propensity score-matched cohort.As it may lack credibility of our results,an accumulation of cases and further investigations will be required.Furthermore,elderly male patients accounted for a large percentage of the study population.Second,although loss of muscle quantity is an important component of sarcopenia,muscle strength (i.e.,grip strength) is presently the most reliable measure of muscle function [11].Because the present study was retrospective in nature,we could not assess the muscle strength.Third,for the same reason,we could not evaluate serum cholesterol or cholecystokinin levels and insulin resistance,which could have helped validate our hypothesis on RAC onset.Prospective studies with larger cohorts are required to validate our results.
In conclusion,low skeletal muscle mass and high visceral adiposity are independent risk factors for RAC.Careful evaluation of a patient’s body composition is useful for developing risk stratification strategies and providing patients with personalized nutritional and lifestyle interventions.In addition,as a fundamental treatment,cholecystectomy should be aggressively considered to prevent the future development of severe and life-threatening RAC in patients with low skeletal muscle mass and high visceral adiposity.
Acknowledgments
None.
CRediT authorship contribution statement
Yudai Koya:Conceptualization,Data curation,Formal analysis,Writing– original draft,Writing– review &editing.Michihiko Shibata:Conceptualization,Data curation,Methodology,Software,Supervision,Writing– review &editing.Yuki Maruno:Data curation.Yoshitaka Sakamoto:Data curation,Writing– review &editing.Shinji Oe:Writing– review &editing.Koichiro Miyagawa:Writing– review &editing.Yuichi Honma:Writing– review &editing.Masaru Harada:Supervision,Writing– review &editing.
Funding
None.
Ethical approval
This study was approved by the Ethics Committee of Kyushu Rosai Hospital Moji Medical Center (No: 04-01;date of approval:June 2,2022).This study was conducted in compliance with the principles of theDeclarationofHelsinki.
Competing interest
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- Recent advances in promising drugs for primary prevention of gastroesophageal variceal bleeding with cirrhotic portal hypertension
- Stereotactic body radiotherapy in pancreatic adenocarcinoma
- Application of ultrasonography-elastography score to suspect porto-sinusoidal vascular disease in patients with portal vein thrombosis
- Polydatin ameliorates hepatic ischemia-reperfusion injury by modulating macrophage polarization
- Hypomethylation of glycine dehydrogenase promoter in peripheral blood mononuclear cells is a new diagnostic marker of hepatitis B virus-associated hepatocellular carcinoma
- AGK2 pre-treatment protects against thioacetamide-induced acute liver failure via regulating the MFN2-PERK axis and ferroptosis signaling pathway