Clinical observation of kidney-tonifying and mindcalming acupuncture therapy in the treatment of perimenopausal insomnia
2024-02-27YANGWenjia杨文佳YUXintong于心同ZHAONa赵娜XIEChen谢晨LIJinjin李金金GAOXiaolin高晓林FUCong付聪CHENYunfei陈云飞
YANG Wenjia (杨文佳), YU Xintong (于心同), ZHAO Na (赵娜), XIE Chen (谢晨), LI Jinjin (李金金), GAO Xiaolin (高晓林),FU Cong (付聪),4,5, CHEN Yunfei (陈云飞)
1 Yueyang Hospital of Integrated Traditional Chinese and Western Medicine, Shanghai University of Traditional Chinese Medicine,Shanghai 200437, China
2 Shanghai Research Institute of Acupuncture and Meridian, Shanghai University of Traditional Chinese Medicine, Shanghai 200030,China
3 Shanghai Fourth People’s Hospital Affiliated Tongji University, Shanghai 200434, China
4 Huashan Hospital, Fudan University, Shanghai 200040, China
5 Sleep and Wake Disorders’ Center of Fudan University, Shanghai 200040, China
Abstract Objective: To observe the effects of kidney-tonifying and mind-calming acupuncture therapy on sleep, mood, sex hormone levels, and traditional Chinese medicine (TCM) symptoms in patients with perimenopausal insomnia (PMI).
Keywords: Acupuncture Therapy; Kidney-tonifying and Mind-calming; Insomnia; Anxiety; Depression; Perimenopause;Female
Perimenopause is a period from two years before menopause to one year after menopause[1].Perimenopausal women may have a series of symptoms due to the gradual decline of ovarian function, and insomnia is one of the most common clinical symptoms[2].Perimenopausal insomnia (PMI) seriously affects the quality of life of perimenopausal women.Studies show that the incidence of PMI in China accounts for 69.39%, and it is one of the three chief complaints of perimenopausal women[3].At present,menopausal hormone therapy (MHT) and sedatives and hypnotics are commonly used in the clinical treatment of PMI, but there are certain adverse reactions.For example, MHT may increase the risk of gynecological cancer[4-5].Sedatives and hypnotics have problems such as tolerance, dependence and withdrawal, residual daytime sedation, risk of recurrent insomnia, memory and cognitive impairments, and motor incoordinationrelated falls in the aged[6].Therefore, there is an urgent need to find effective and safe treatments for PMI.
Clinical studies have confirmed that acupuncture has a significant effect on PMI[7-8].Our previous clinical research results also showed that acupuncture could significantly improve the clinical symptoms of PMI patients without adverse reactions[9].On the basis of previous research, with the principle of “treating from the kidney and treating both the tip and root”, we selected Shenshu (BL23), Taixi (KI3), Baihui (GV20), and Anmian (Extra) to treat PMI, and observed the effects of kidney-tonifying and mind-calming acupuncture on sleep, mood, sex hormone levels, and traditional Chinese medicine (TCM) symptoms in patients with PMI.
1 Clinical Materials
1.1 Diagnostic criteria
1.1.1 Diagnostic criteria in Western medicine
The diagnostic criteria for insomnia in the third edition of theInternational Classification of SleepDisorders(ICSD-3)[10]were used in conjunction with the staging criteria for perimenopause issued by the Stages of Reproductive Aging Workshop (STRAW)[11].
1.1.2 Diagnostic criteria for TCM symptoms
Referred to the diagnostic criteria for TCM pattern of kidney Yin deficiency established in theGuiding Principles for Clinical Study of New Chinese Medicines[12].
1.2 Inclusion criteria
Female, aged 40-60 years; in accordance with the above Western medicine diagnostic criteria and TCM symptom diagnostic criteria; had not received acupuncture treatments; informed consent was obtained.
1.3 Exclusion criteria
Patients who used sex hormone drugs in the latest 3 months; with severe mental disorders; with severe cardiac or cerebral complications; pregnant or lactating women; were participating in other clinical trials.
1.4 Statistical analysis
The SPSS version 26.0 software was used for data analysis.The measurement data were in accordance with normal distribution and expressed as mean ±standard deviation (±s).Thet-test was used for comparisons between groups, and repeated measures analysis of variance was used for comparisons between multiple time points within the group.Count data were expressed as frequencies or rates, and comparisons between groups were analyzed using the Chi-square test.P<0.05 was considered statistically significant.
1.5 General data
A total of 90 PMI subjects were included in this study,and all of them were patients who visited the Outpatient Department of Acupuncture of Yueyang Hospital of Integrated Traditional Chinese and Western Medicine, Shanghai University of Traditional Chinese Medicine between December 2018 and December 2021.This study was approved by the Ethics Committee of Yueyang Hospital of Integrated Traditional Chinese and Western Medicine, Shanghai University of Traditional Chinese Medicine (Approval No.2015-020).The patients were randomly divided into a control group and a treatment group by the random number table method, with 45 cases in each group.During randomization, the generation of the random number table, the inclusion of subjects, and the evaluation of the scales were completed independently by different researchers.In the treatment group, the youngest was 40 years old, and the oldest was 60.The shortest course of disease was 6 months, and the longest was 21 months.In the control group, the youngest was 40 years old, and the oldest was 59.The disease duration ranged from 5 months to 19 months.There was no significant difference in the general data between the two groups (P>0.05), showing comparability.See Table 1.
During the trial, 2 cases withdrew, and 43 cases completed the trial in the treatment group, while 45 cases completed the trial in the control group.A total of 88 cases were finally included in the statistical analysis.The flow of the trial is shown in Figure 1.
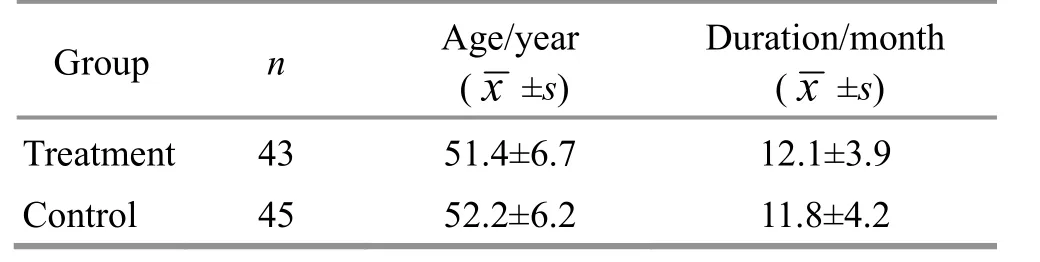
Table 1 Comparison of general data between the two groups
2 Treatment Methods
2.1 Treatment group
The treatment group was treated with acupuncture based on the principles of kidney-tonifying and mindcalming.
Points: Baihui (GV20), bilateral Shenshu (BL23), Taixi(KI3), and Anmian (Extra)[13].
Methods:The patient took a sitting position on the treatment bed.After local skin disinfection of the points,disposable sterile acupuncture needles of 0.25 mm in diameter and 40 mm in length were used for needling.Shenshu (BL23) was inserted 10-15 mm at an angle of 15° toward the spine, and the patient was assisted to lie down slowly by holding the handle of the needle after insertion; Baihui (GV20) was inserted subcutaneously by a depth of 10-15 mm; Taixi (KI3) and Anmian (Extra)were inserted perpendicularly by a depth of 10-15 mm,and the positioning of the points is shown in Figure 2.After the needles were inserted to obtain the needling sensation (Deqi), the balanced reinforcing and reducing manipulation was performed.The needles were retained for 30 min.The patient was treated 3 times per week for 4 weeks in total.
2.2 Control group
The control group was treated with sham acupuncture by shallow needling at sham points[14].
Sham points: Sham Baihui (GV20) and bilateral sham Shenshu (BL23), sham Taixi (KI3), and sham Anmian(Extra) were taken.The position of sham Shenshu (BL23)was 1 Cun below and beside Shenshu (BL23).The sham Taixi (KI3) was positioned 1 Cun above and 0.5 Cun beside Taixi (KI3).The sham Baihui (GV20) was positioned at the midpoint between the right and posterior Sishencong (EX-HN1).The sham Anmian (Extra)was 1 Cun below Anmian (Extra).The location of sham points is shown in Figure 2.
Methods: The patient was in a sitting position on the treatment bed.After local skin disinfection, sterile acupuncture needles of 0.25 mm in diameter and 40 mm in length were used to stimulate the sham points.The sham Shenshu (BL23) was inserted 1-2 mm at an angle of 15° toward the spine, and the patient was assisted to lie down slowly by holding the handle of the needle after insertion; sham Baihui (GV20) was inserted subcutaneously by a depth of 1-2 mm; sham Taixi (KI3)and Anmian (Extra) were inserted perpendicularly by a depth of 1-2 mm.No manipulation was performed after needle insertion to avoid needling sensation (Deqi).The treatment was given 3 times a week for 4 weeks.

Figure 2 Localization of points and sham points
3 Outcomes Observation
3.1 Observation items
3.1.1 Primary outcome measures
Pittsburgh sleep quality index (PSQI) scale[15]was used for the subjective evaluation of patients’ sleep quality; the higher the score, the worse the sleep quality.
Insomnia severity index (ISI) scale[16]was mainly used to evaluate the nature and severity of insomnia and its impact on the daytime function of patients.The more severe the insomnia, the higher the score.
The two scales were evaluated before treatment,after treatment, and at 1-month follow-up.
3.1.2 Secondary outcome measures
Beck depression inventory (BDI) was used to evaluate the depression of subjects[17].Generally, the total score of BDI greater than or equal to 15 points is used as the judgment of positive depression.
Beck anxiety inventory (BAI) was used to evaluate the anxiety of subjects[18].Generally, the total score of BAI greater than or equal to 45 points is used as the judgment of positive anxiety.
TCM symptom scale was used to evaluate the TCM symptoms of patients.It consists of 7 parts, including 2 main symptoms, 4 secondary symptoms, tongue manifestations, and pulse conditions.No symptoms,scored 0 points; 1 point, if the symptoms occur rarely and can be relieved spontaneously; 2 points, if the symptoms can be controlled and relieved quickly after taking medicine; symptoms occur frequently and severely affect normal work and life, 3 points.
The above scales were evaluated before treatment,after treatment, and at 1-month follow-up.
The serum sex hormone levels of estradiol (E2),follicle-stimulating hormone (FSH), and luteinizing hormone (LH) were detected by the chemiluminescence method before and after treatment.
3.2 Results
3.2.1 Comparison of the PSQI score between the two groups at different time points
There was no statistically significant difference in the PSQI score between the two groups before treatment(P>0.05).The PSQI score of all subjects showed a time effect with the progression of the treatment (P<0.05),indicating that the PSQI score changed significantly with time.The comparison of PSQI score in both two groups showed a group effect (P<0.05), indicating that different treatment methods could significantly affect the PSQI score of patients.There was an interaction effect between group and time (P<0.05), indicating that the changing trend of PSQI score was different due to different treatment methods over time.
The PSQI score of the treatment group after intervention and at the 1-month follow-up was significantly lower than that before treatment (P<0.05),and the scores at the two time points were significantly different from those of the control group (P<0.05).In the control group, the PSQI score after treatment was significantly lower than that before treatment (P<0.05),but there was no significant difference in PSQI score at 1-month follow-up compared with that before treatment (P>0.05).See Table 2 for details.
3.2.2 Comparison of the ISI score between the two groups at different time points
There was no statistically significant difference in the ISI score between the two groups before treatment(P>0.05).The ISI score of all subjects showed a time effect with the progression of treatment (P<0.05),indicating that the ISI score would change significantly with time.There was a group effect in the overall comparison of ISI score in the two groups (P<0.05),indicating that different treatment methods could significantly affect the ISI score of patients.There was an interaction effect between group and time (P<0.05),indicating that the changing trend of ISI score over time would be different due to different treatment methods.
The ISI score of the treatment group after intervention and at the 1-month follow-up was significantly lower than that before treatment (P<0.05), and the scores at the two time points were significantly different from those of the control group (P<0.05).There was no statistically significant difference in the ISI score before treatment, after treatment, and at 1-month follow-up in the control group (P>0.05).See Table 3 for details.
3.2.3 Comparison of the BDI score between the two groups at different time points
There was no statistically significant difference in the BDI score between the two groups before treatment(P>0.05).The BDI score of all subjects showed a time effect with the treatment process (P<0.05), indicating that the BDI score would change significantly with time.There was a group effect in the overall comparison of BDI score in the two groups (P<0.05), indicating that different treatment methods could significantly affect the BDI score of patients.There was an interaction effect between group and time (P<0.05), indicating that the changing trend of BDI score over time would be different due to different treatment methods.
The BDI score of the treatment group after treatment and at the 1-month follow-up was significantly lower than that before treatment (P<0.05), and the score at each time point was significantly different from that of the control group (P<0.05).In the control group, there was no statistically significant difference in the BDI score before treatment, after treatment, and at 1-month follow-up (P>0.05).See Table 4 for details.
Table 2 Results of the repeated measures analysis of variance of the PSQI score in the two groups ( ±s) Unit: point

Table 2 Results of the repeated measures analysis of variance of the PSQI score in the two groups ( ±s) Unit: point
Note: PSQI=Pittsburgh sleep quality index; compared with the same group before treatment, 1) P<0.05; compared with the control group at the same time point, 2) P<0.05.
Group n Before treatment After treatment 1-month follow-up Treatment 43 17.35±2.11 13.70±3.021)2) 13.81±1.941)2)Control 45 17.40±2.10 16.31±1.471) 16.58±1.84 Intervention F=12.417, P<0.001 Time F=37.038, P<0.001 Intervention * Time interaction F=40.310, P<0.001
Table 3 Results of the repeated measures analysis of variance of the ISI score in the two groups ( ±s) Unit: point
Note: ISI=Insomnia severity index; compared with the same group before treatment, 1) P<0.05; compared with the control group at the same time point, 2) P<0.05.
Group n Before treatment After treatment 1-month follow-up Treatment 43 22.30±3.48 13.95±3.221)2) 14.35±4.041)2)Control 45 22.82±3.83 21.64±3.28 21.66±3.34 Intervention F=28.796, P<0.001 Time F=51.109, P<0.001 Intervention * Time interaction F=94.369, P<0.001
Table 4 Results of the repeated measures analysis of variance of the BDI score in the two groups ( ±s) Unit: point
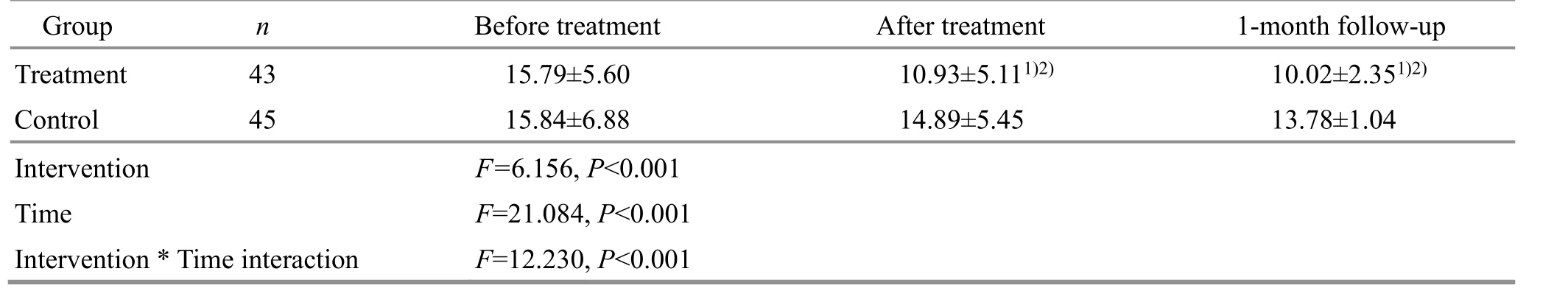
Table 4 Results of the repeated measures analysis of variance of the BDI score in the two groups ( ±s) Unit: point
Note: BDI=Beck depression inventory; compared with the same group before treatment, 1) P<0.05; compared with the control group at the same time point, 2) P<0.05.
Group n Before treatment After treatment 1-month follow-up Treatment 43 15.79±5.60 10.93±5.111)2) 10.02±2.351)2)Control 45 15.84±6.88 14.89±5.45 13.78±1.04 Intervention F=6.156, P<0.001 Time F=21.084, P<0.001 Intervention * Time interaction F=12.230, P<0.001
3.2.4 Comparison of the BAI score between the two groups at different time points
There was no significant difference in the BAI score between the two groups before treatment (P>0.05).The BAI score of all subjects showed a time effect(P<0.05), indicating that the BAI score would change with the treatment process significantly with time.The overall comparison of BAI score in the two groups showed a group effect (P<0.05), indicating that different treatment methods could significantly affect the BAI score of patients.There was an interaction effect between group and time (P<0.05), indicating that the changing trend of BAI score over time was different due to different treatment methods.
The BAI score of the treatment group after treatment and at the 1-month follow-up was significantly lower than that before treatment (P<0.05),and there was a significant difference between the treatment group and the control group at each time point (P<0.05).In the control group, there was no significant difference in the BAI score before treatment,after treatment, and at 1-month follow-up (P>0.05).See Table 5 for details.
3.2.5 Comparison of the TCM symptom scale score between the two groups at different time points
There was no statistically significant difference in the TCM symptom scale score between the two groups before treatment (P>0.05).There was a time effect in the comparison of the TCM symptom scale score over the treatment process (P<0.05), indicating that TCM symptom scale score would change significantly with time.The overall comparison of TCM symptom scale score in the two groups showed a group effect (P<0.05),indicating that different treatment methods could significantly affect the TCM symptom scale score.There was an interaction effect between group and time(P<0.05), indicating that the changing trend of TCM symptom scale score over time would be different due to the different treatment methods.
The TCM symptom scale score after treatment and at the 1-month follow-up in the treatment group was significantly lower than that before treatment (P<0.05),and the scores at the two time points were significantly different from those in the control group (P<0.05).There was no statistically significant difference in the TCM symptom scale score before treatment, after treatment, and at 1-month follow-up in the control group (P>0.05).See Table 6 for details.
3.2.6 Comparison of the serum sex hormone levels between the two groups before and after treatment Before treatment, there were no statistically significant differences in the serum LH, FSH, and E2levels between the two groups (P>0.05).After treatment, the serum E2level in the treatment group was significantly higher than that before treatment(P<0.05), and the difference was statistically significant compared with the control group (P<0.05).There was no significant difference in E2before and after treatment in the control group (P>0.05).After treatment, there was no significant change in the serum LH and FSH levels in either group (P>0.05), and there was no significant difference between the two groups(P>0.05).See Table 7 for details.
3.2.7 Safety evaluation
During the treatment, there were no cases of dizziness, broken needles, or infection in the two groups.
Table 5 Results of the repeated measures analysis of variance of the BAI score in the two groups ( ±s) Unit: point

Table 5 Results of the repeated measures analysis of variance of the BAI score in the two groups ( ±s) Unit: point
Note: BAI=Beck anxiety inventory; compared with the same group before treatment, 1) P<0.05; compared with the control group,2) P<0.05.
Group n Before treatment After treatment 1-month follow-up Treatment 43 images/BZ_57_597_1345_601_1346.png32.02±7.87 25.88±3.861)2) 24.81±3.691)2)Control 45 33.82±10.40 30.96±4.67 32.13±4.01 Intervention F=3.842, P<0.001 Time F=12.407, P<0.001 Intervention * Time interaction F=26.944, P=0.025
Unit: point
Table 6 Results of the repeated measures analysis of variance of the TCM symptom scale score in the two groups ( ±s)
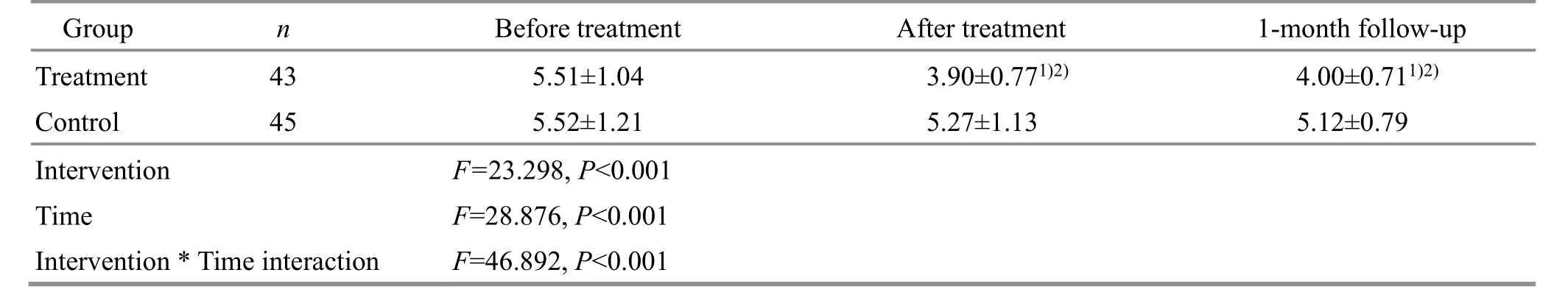
Table 6 Results of the repeated measures analysis of variance of the TCM symptom scale score in the two groups ( ±s)
Note: Compared with the same group before treatment, 1) P<0.05; compared with the control group, 2) P<0.05.
Group n Before treatment After treatment 1-month follow-up Treatment 43 5.51±1.04 3.90±0.771)2) 4.00±0.711)2)Control 45 5.52±1.21 5.27±1.13 5.12±0.79 Intervention F=23.298, P<0.001 Time F=28.876, P<0.001 Intervention * Time interaction F=46.892, P<0.001
Table 7 Comparison of serum sex hormones before and after treatment in the two groups ( ±s)
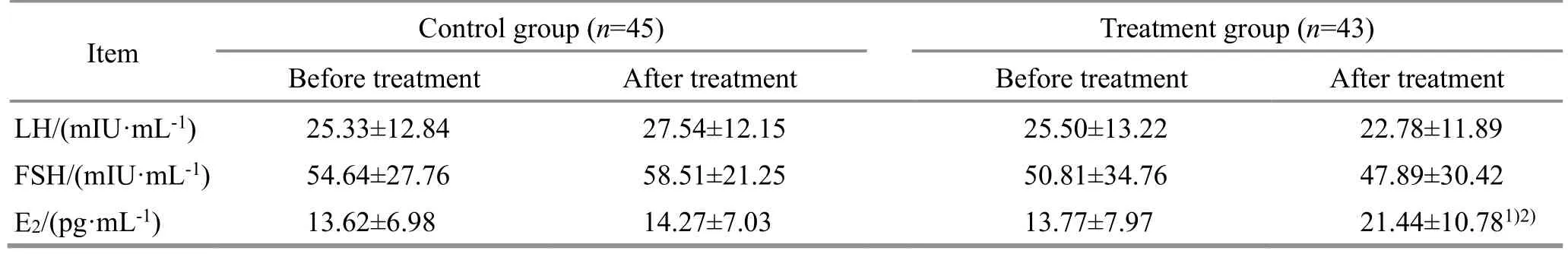
Table 7 Comparison of serum sex hormones before and after treatment in the two groups ( ±s)
Note: LH=Luteinizing hormone; FSH=Follicle-stimulating hormone; E2=Estradiol; compared with the same group before treatment,1) P<0.05; compared with the control group, 2) P<0.05.
Item Control group (n=45) Treatment group (n=43)Before treatment After treatment Before treatment After treatment LH/(mIU·mL-1) 25.33±12.84 27.54±12.15 25.50±13.22 22.78±11.89 FSH/(mIU·mL-1) 54.64±27.76 58.51±21.25 50.81±34.76 47.89±30.42 E2/(pg·mL-1) 13.62±6.98 14.27±7.03 13.77±7.97 21.44±10.781)2)
4 Discussion
PMI belongs to the categories of “symptoms before and after menopause” and “insomnia” in TCM.When a woman reaches the perimenopausal period, her kidney essence gradually fails, her Tian Gui is insufficient, and the Thoroughfare Vessel and Conception Vessel are feeble, resulting in insufficient essence and blood and irregular menstruation.And women consume more blood throughout their life, which is the state that“Yin is often insufficient, and Yang is often in excess”[19].Therefore, the mechanism of this disease is mostly deficiency of kidney Yin, and Yin and Yang are imbalanced in the body, which triggers the dysfunction of organs in the whole body, resulting in a variety of symptoms, including insomnia[20-21].In this study, the treatment principle is to tonify the kidney and calm the mind, and Shenshu (BL23), Taixi (KI3), Baihui (GV20),and Anmian (Extra) were selected and given acupuncture treatment.Shenshu (BL23) is the back-Shu point of the kidney, and Tian Gui is hidden in the kidney,so Shenshu (BL23) can secure the innate essence[22].At the same time, the Bladder Meridian enters the brain and is closely related to the brain marrow, so acupuncture at Shenshu (BL23) can regulate brain function and help to calm the mind[23].Taixi (KI3) is the Shu-stream point and Yuan-primary point of the Kidney Meridian and can replenish kidney Yin[24].Baihui (GV20)is located at the top of the summit and is mainly used to treat spirit diseases.It is at the center of the head and can effectively regulate the brain and spirit functions,thereby can treat insomnia[25].Anmian (Extra) is an extra point that can regulate the operation of meridian Qi in the Yin Heel Vessel and Yang Heel Vessel, and it is one of the special points for the treatment of insomnia[26].Shenshu (BL23), Taixi (KI3), Baihui (GV20),and Anmian (Extra) are used together to treat both the symptoms and the root cause of insomnia, and they work together to tonify the kidney and calm the mind.
Modern medicine believes that due to ovarian failure,the level of estrogen in perimenopausal women will decrease sharply, which leads to a decrease in the regulation function of estrogen in the central nervous system, and thus insomnia happens[2].E2is the major form of estrogen.The E2level decreases rapidly during perimenopause and thus leads to several changes in the brain that have an impact on sleep, mood, and cognition[27].Studies have found that E2levels are inversely related to sleep problems, and the decreased E2is associated with difficulty falling asleep and multiple awakenings[28-29].Perimenopausal women’s sleep changes are often characterized by subjective complaints such as difficulty falling asleep, difficulty maintaining asleep, and inability to resume sleep after sleep interruption, which can lead to severe daytime symptoms, including inattention and mood disturbances[30].Insomnia is one of the sources of perimenopausal distress in women and has a significant impact on patients’ quality of life, mood, productivity,and physical health[31-32].This sleep disorder is strongly associated with an increased risk of cardiovascular diseases, depression, diabetes, and neurobehavioral disorders[33-34].At the same time, decreased ovarian estrogen secretion is also a high-risk factor for emotional disorders[35].Perimenopause is a window of vulnerability to the development of depressive symptoms and major depressive episodes[36-38].The incidence of perimenopausal depressive symptoms is high[39-40].It has been clinically confirmed that estrogen therapy can improve perimenopausal emotional disorders[41].In addition, animal experiments have also confirmed that estrogen treatment can improve the symptoms of depression and anxiety in perimenopausal rat models[42].These have revealed a close relationship between estrogen and mood disorders[43].
This study aims to evaluate the clinical efficacy of kidney-tonifying and mind-calming acupuncture in the treatment of PMI from the aspects of sex hormone levels, sleep, mood, and TCM symptoms.The results showed that kidney-tonifying and mind-calming acupuncture could significantly reduce the PSQI score and ISI score of patients with PMI and improve the symptoms of insomnia.It can reduce the TCM symptom scale score and improve the TCM symptoms of patients.It can reduce the scores of anxiety and depression scales and improve the mood of patients.E2can activate sleep-promoting neurons in the hypothalamus,the sleep center, through E2receptors, and decreased E2reduces the activation of sleep-promoting neurons,leading to the occurrence of insomnia[44-46].The results of this study showed that acupuncture therapy could increase the serum E2level in patients with PMI.It is suggested that kidney-tonifying and mind-calming acupuncture therapy may improve the sleep, mood,and TCM symptoms of PMI patients with kidney Yin deficiency by improving the regulation function of E2in the sleep center.The control group was treated with sham acupuncture.The results showed that sham acupuncture could reduce the PSQI score of the subjects to a certain extent after treatment, but the PSQI score of the treatment group was significantly lower than that of the control group, suggesting that sham acupuncture had a certain improvement effect on insomnia symptoms in patients with PMI, but the effect of real acupuncture was better and lasting.
In conclusion, the results of this study indicate that kidney-tonifying and mind-calming acupuncture therapy can improve sleep quality, mood, and TCM symptoms, increase the serum E2level, and have a significant clinical effect on PMI patients with kidney Yin deficiency.However, the number of cases included in this study was small.In the future, the sample size will be increased, and multi-center large-sample randomized controlled trials will be carried out to reduce the influence of sample differences on the results, so as to further explore the mechanism of acupuncture in improving PMI.
Conflict of Interest
The authors declare that there is no potential conflict of interest in this article.
Acknowledgments
This work was supported by the Project of Science and Technology Commission of Shanghai Municipality (上海市科学技术委员会项目, No.21Y11923800); Projects of Shanghai Municipal Health Commission (上海市卫生健康委员会项目, No.202140422, No.2022QN067); Shanghai Clinical Research Center for Acupuncture and Moxibustion(上海市针灸临床医学研究中心, No.20MC1920500).
Statement of Informed Consent
Informed consent was obtained from all individual participants.
Received: 5 February 2023/Accepted: 18 May 2023
猜你喜欢
杂志排行
Journal of Acupuncture and Tuina Science的其它文章
- Efficacy observation of long-time needle retaining at Baihui (GV20) combined with multidirectional pointtoward-point needle insertion with needle shaking at Fengchi (GB20) for cervical vertigo
- Efficacy of electroacupuncture on the recovery of gastrointestinal function after laparoscopic cholecystectomy: a systematic review
- Fascia is the “sensor” for the coupling response of manipulative therapies
- Clinical study of electroacupuncture improving sleep electroencephalogram and event-related potential in patients with somatoform disorders
- Effects of warming triple needling plus Chinese medication on inflammatory responses and daily functioning ability in knee osteoarthritis patients
- Clinical study of electroacupuncture combined with exercise therapy in improving the balance function of patients with knee osteoarthritis