Percutaneous antegrade management of large proximal ureteral stones using non-papillary puncture
2024-02-25ArmnTsturynAngelisPeteinrisConstntinosAdmouKonstntinosPgonisLusineMusheghynAnstsiosNtsosTheofnisVrettosEvngelosLitsikosPngiotisKllidonis
Armn Tsturyn,Angelis Peteinris,Constntinos Admou ,Konstntinos Pgonis ,Lusine Musheghyn ,Anstsios Ntsos ,Theofnis Vrettos,Evngelos Litsikos,d,Pngiotis Kllidonis
a Department of Urology,University of Patras,Patras,Greece
b Gerald and Patricia Turpanjian School of Public Health,American University of Armenia,Yerevan,Armenia
c Department of Anesthesiology and ICU,University of Patras,Patras,Greece
d Department of Urology,Medical University of Vienna,Vienna,Austria
KEYWORDS Antegrade percutaneous nephrolithotomy;Proximal ureteral stone;Non-papillary puncture;Large ureteral stone;Prone percutaneous nephrolithotomy
Abstract Objective: To evaluate the feasibility and the safety of medial non-papillary percutaneous nephrolithotomy (npPCNL) for the management of large proximal ureteral stones.Methods: We evaluated prospectively collected data of 37 patients with large proximal ureteral stones more than 1.5 cm in diameter treated by prone npPCNL.Depending on stone size,in-toto stone removal or lithotripsy using the Lithoclast® Trilogy (EMS Medical,Nyon,Switzerland) was performed.Perioperative parameters including operative time (from start of puncture to the skin suturing),stone extraction time(from the first insertion of the nephroscope to the extraction of all stone fragments),and the stone-free rate were evaluated.Results: Twenty-one males and 16 females underwent npPCNL for the management of large upper ureteral calculi.The median age and stone size of treated patients were 58 (interquartile range [IQR]: 51-69) years and 19.3 (IQR: 18.0-22.0) mm,respectively.The median operative time and stone extraction time were 25 (IQR: 21-29) min and 8 (IQR: 7-10) min,respectively.One case (2.7%) of postoperative bleeding and two cases (5.4%) of prolonged fever were managed conservatively.The stone-free rate at a 1-month follow-up was 94.6%.Conclusion: The npPCNL provides a straight route to the ureteropelvic junction and proximal ureter.Approaching from a dilated portion of the ureter under low irrigation pressure with larger diameter instruments results in effective and safe stone extraction within a few minutes.
1.Introduction
The management of patients with large proximal ureteral stones is still demanding [1]and the approach of choice appears to depend on the urologist expertise and type of the available treatment device [2].Retrograde ureteroscopic lithotripsy is generally the preferred surgical method for most cases due to its lower morbidity.Its success rate decreases in patients with stones larger than 1 cm in diameter [3].The treatment can become even more challenging when the impaction of the stone into the ureteral wall is present [1].Thus,the disintegration of large stones may be complicated by the creation of many residual fragments,prolongation of the surgery,risk of injury of the ureteral wall,and subsequent development of ureteral stenosis [4].
Percutaneous antegrade ureterolithotripsy (PAUL) is an effective,minimally invasive option to treat large upper ureteral stones,with reported stone-free rates (SFRs) between 85% and 100%[3,5,6].Several studies have demonstrated the superiority of PAUL over retrograde ureterolithotripsy and laparoscopic ureterolithotomy in terms of SFR and duration of the surgery [2,6].Despite its promising outcomes,the PAUL approach can be associated with a variety of postoperative complications such as bleeding,infectious complications,and injury of adjacent organs[7].
To establish proper access to the upper ureter,middle or upper calyceal punctures have been used [8,9].Nevertheless,the complex structure of pelvicalyceal anatomy may obscure and limit the manipulation in the upper ureter requiring the use of flexible instruments.In contrast,medial non-papillary puncture allows direct access to the renal pelvis[10]and may facilitate faster and easier lithotripsy.
The current article aimed to evaluate the feasibility and the safety of medial non-papillary percutaneous nephrolithotomy (npPCNL) for the management of large proximal ureteral stones.
2.Patients and methods
2.1.Study design and study population
We conducted a retrospective cohort study using an institutionally (University General Hospital of Patras) approved prospective database for registration of percutaneous nephrolithotomy (PCNL) cases to evaluate perioperative parameters of patients undergoing prone standard (30 Fr)npPCNL for the antegrade management of large proximal ureteral stones larger than or equal to 1.5 cm in diameter.Patients treated between June 2018 and January 2021 were included.Exclusion criteria included the presence of concomitant ipsilateral large renal stones (≥5 mm in diameter),antegrade ureterolithotripsy through mini-PCNL tract (<22 Fr),partial or complete staghorn stones,anatomical abnormalities (malrotated kidney,polycystic kidney,or horseshoe kidney),and prior history of PCNL or open renal surgery.Written consents were obtained from all the patients.The study has been carried out in accordance with the ethical standards,and approved by the ethical committee of University of Patras (ethical approval number 536/06.01.2021).
2.2.Surgical technique and postoperative follow-up
All procedures were performed by two experienced surgeons with the expertise of more than 50 PCNL cases per year.After induction of general anesthesia,an open-end ureteral catheter was introduced and a retrograde pyelography was performed in a lithotomy position.The patient was then placed in a prone position and a medial nonpapillary biplanar fluoroscopic-guided puncture was performed (Fig.1).The latter is the preferred standard treatment technique of percutaneous access at our department.

Figure 1 Percutaneous antegrade management of large upper ureteral stones.(A)Fluoroscopic image showing a 2.3 cm stone in the upper ureter (stone was shown with the arrow head);(B) Fluoroscopic image showing a medial non-papillary percutaneous nephrolithotomy puncture;(C) Immediate fluoroscopic image following non-papillary percutaneous nephrolithotomy showing the complete clearance of the stone;(D)Extracted stone pieces.
A one-step dilation with balloon dilator (NephroMax,Boston Scientific,Marlborough,Massachusetts,USA) or a two-step dilation with Amplatz dilators (Amplatz renal dilator set,COOK Medical,Bloomington,Indiana,USA) to the size of 30 Fr outer sheath was performed over the stiff guidewire.The site of the puncture was decided on intraoperative fluoroscopic images with the C-arm at 0°and 30°considering the anatomy to have easier and straight access to the ureteropelvic junction and upper ureter.The pelvis and the medial calyceal groups were the preferred puncture sites.A detailed description of the puncture and tract dilation technique was described elsewhere [10].
For smaller stones and stone fragments of less than 1 cm,subjectively assessed by the endoscopic image of the nephroscope,anin-totostone removal was performed(Fig.1).Otherwise,the Lithoclast®Trilogy (EMS Medical,Nyon,Switzerland)was used to achieve lithotripsy.A longer PCNL sheath(Cook Medical,Bloomington,Indiana,USA)and a longer nephroscope (Karl Storz,Tuttlingen,Germany)were used in cases when longer tracts were needed.An antegrade flexible ureteroscopy (digital Xc 8.5 Fr,Karl Storz,Tuttlingen,Germany) was performed if antegrade stone migration to the ureter was suspected or for stones that could not be reached with the rigid nephroscope.A 24 Fr Malecot tale tube (Cook Medical,Bloomington,Indiana,USA) or a 20 Fr balloon nephrostomy tube (Cook Medical,Bloomington,Indiana,USA) together with a double-J stent was placed at the end of the procedure.The nephrostomy tubes were routinely removed on postoperative Day 2 or Day 3.The removal of the double-J stent was scheduled at 2-4 weeks following the procedure.
2.3.Study variables and statistical analysis
Patient demographics and stone characteristics including age,gender,body mass index,American Society of Anesthesiologists score,cumulative stone size,and perioperative parameters were recorded.The Clavien-Dindo classification was used to grade the postoperative complications [11].The continuous drop of hemoglobin with or without a need for blood transfusion was reported clinically significant.Patients were documented to develop infectious complications when a body temperature of more than 38.0°C was observed.
The perioperative parameters including operative time(from the start of puncture to the skin suturing) and stone extraction time(from the first insertion of the nephroscope to the extraction of all stone fragments) were evaluated.For multiple ureteral stones and uretero-pelvic junction stones,the sum of the largest diameters of all stones was calculated.The SFR was defined as the absence of any fragments on non-contrast-enhanced CT evaluated at 1 month following the surgery.All patients underwent additional follow-up imaging with ultrasound at 6 months after the surgery.
Statistical analyses were performed using SPSS v.21.0(IBM SPSS Statistics,Armonk,NY,USA).Medians and interquartile ranges (IQRs) were used to describe continuous variables and proportions for categorical variables.
3.Results
Patient demographics and stone characteristics are shown in Table 1.Twenty-one males and 16 females underwent npPCNL for the management of large upper ureteral calculi.The median age and body mass index of treated patients were 58 (IQR: 51-69) years and 27.4 (IQR:25.5-29.6)kg/m2,respectively.The median operative time was 25 (IQR: 21-29) min.With a median stone size of 19.3(IQR: 18.0-22.0) mm,a median of 8 (IQR: 7-10) min was required to reach complete extraction of all stone fragments.In six patients,the removal of ureteral stone was accompanied by the extraction of small renal stones of less than 5 mm from the lower calyx.The stone fragmentation was required in 30 (81.1%) patients,whilein-totostone extraction was achieved in 7 (18.9%) patients.In 8 (21.6%)patients,antegrade flexible ureteroscopy was performed due to a suspected migration of a stone fragment.A successful irrigation-assisted expulsion of the stone fragment into the urinary bladder was achieved in three patients,whereas no stones were revealed in five patients.Postoperative bleeding and prolonged fever (Grade II complications) were observed in 1 (2.7%) and 2 (5.4%) patients,respectively.All complications were managed conservatively and patients were discharged on postoperative Day 2 or Day 3.The SFR at 1-month follow-up was 94.6%(Table 1).No moderate or severe hydronephrosis requiring any additional treatment,or signs of residual stone fragments or stricture at the stone site were observed at the 6-month follow-up investigation.
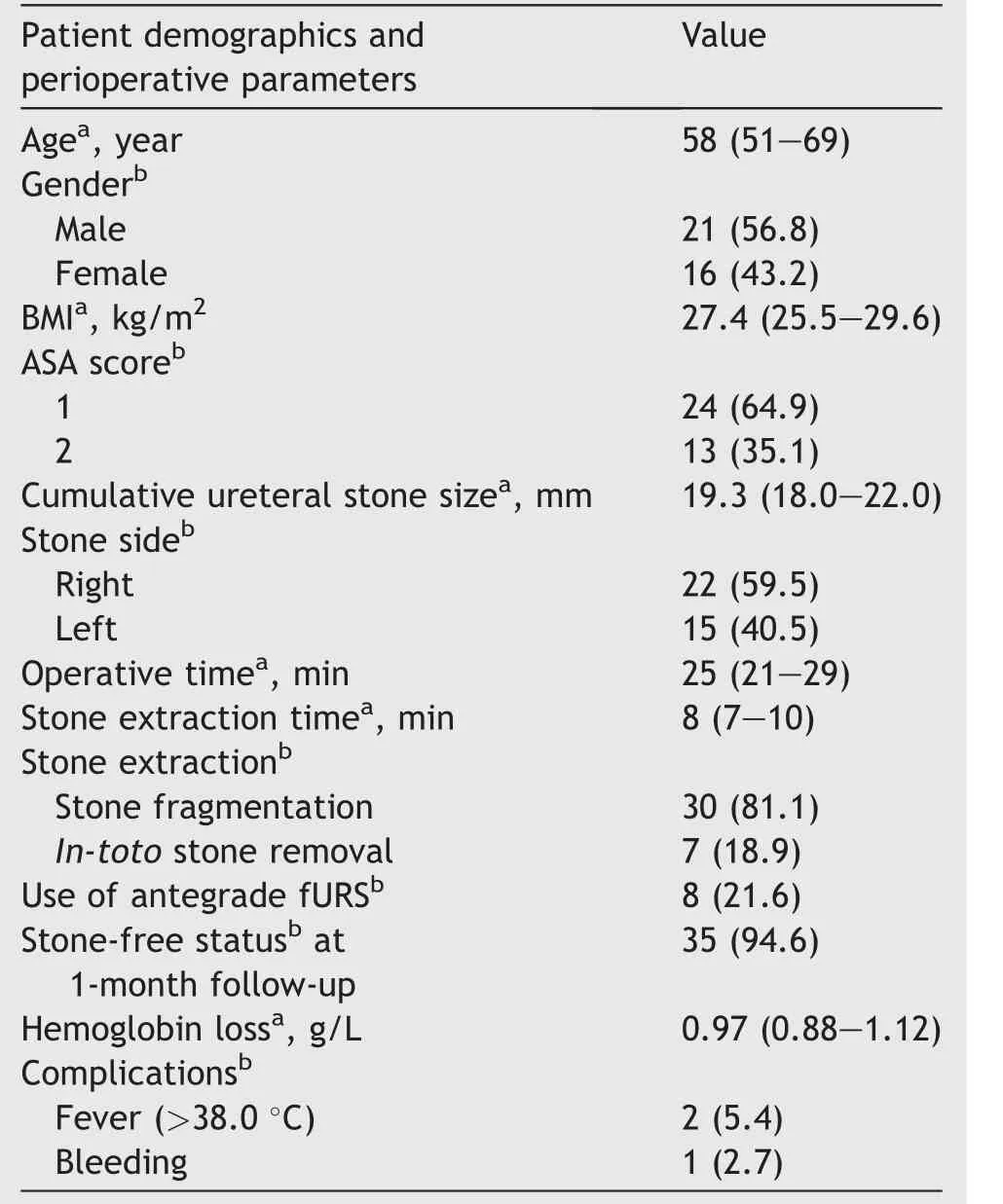
Table 1 Patient demographics and perioperative parameters (n=37).
4.Discussion
In the current study,we reported our initial data of patients with large proximal ureteral stones treated with prone npPCNL.We performed standard PCNL with an outer sheath diameter of 30 Fr,in order to ensure low intrarenal pressure and achieve fast evacuation of the generated fragments.Most of our patients (35 out of 37) were stone-free at 1-month follow-up.The proposed technique was associated with short overall operative and stone extraction time.Postoperative Grade II complications occurred only in 8.1% of the whole cohort.
The optimal treatment of proximal ureteral stones is thought to be a matter of debate.The current European Association of Urology guidelines on proximal ureteral stones larger than 1 cm recommend a ureterorenoscopy(URS) lithotripsy and shock wave lithotripsy as a first-and second-line therapy,respectively [12].The role of PAUL as a therapeutic option is less studied.It is considered an option in selected cases,such as impacted upper ureteral stones causing dilation of the pelvicalyceal system [5].Nevertheless,some of its advantages mainly the high SFR and short operative time,make this approach an appealing choice for proximal ureteral stones.
The PAUL may carry an additional risk of developing postoperative complications compared to retrograde URS.Similar to the standard PCNL,the kidney puncture and dilation of up to 30 Fr may pose a risk for developing different complications [7].According to the Clinical Research Office of the Endourological Society global study,postoperative fever is the most often observed complication with occurrence rate of 10.5%,followed by bleeding with 7.8%[13].However,the most recent systematic review and meta-analysis comparing antegrade and retrograde ureterolithotripsy did not reveal statistically significant differences in the overall complication rates between the two techniques [1].Although the bleeding rate was higher in patients treated with the antegrade approach,it did not significantly affect the rate of blood transfusion.
While the PAUL may possess potential morbidity for the patient,it remains a highly effective treatment modality for proximal ureteral stones with a reported SFR of up to 100% [2,9,14,15].The PAUL can be also an optimal option for patients failing initial treatment with shock wave lithotripsy and retrograde URS [16].In a comparative study,Topaloglu et al.[16]demonstrated 100% SFR at 1-month follow-up in 37 patients utilizing 30 Fr middle calyceal tract dilation.The described complications were hemoglobin decrease (mean: 1.6 g/dL) and the postoperative fever occurring in four patients.Our results are in line with the available literature.Similar to best practices,we were able to show a 100% success rate with only two complications developing in three (8.1%) patients.
In our opinion,an important factor to advocate the performance of PAUL is its short duration of the surgery,and fast disintegration and evacuation of stone fragments.As such,the total median operative time was only 25 min and only a median of 8 min was required to clear stone fragments.While similar shorter operative time was reported with PAUL compared to retrograde URS [8,15],the duration of our surgeries was significantly shorter.A possible explanation for these differences can be the site of the puncture and tract dilation.The reported studies so far included patients undergoing papillary middle and upper calyceal punctures [2,3,5,8,9,14-16].However,in our cohort,a medial non-papillary puncture was performed overpassing the calyces and the difficult angles thereof.The abovementioned allowed direct access to the pelvis and proximal ureter,as well as eliminated any “torquing” of the renal intraparenchymal structures with the rigid scope.The latter is believed to be the commonest cause of perioperative bleeding [17].
Having the nephroscope and the percutaneous tract in a straight line with the ureter and stones makes the removal of large stone pieces possible without fear of damage or rupture to the kidney parenchyma.Besides,working from a dilated portion of the ureter allows the surgeon to pull stones for the narrowed,inflamed ureteral area.As such,safe fragmentation of stones can be achieved with no risk for ureteral wall perforation,described as the primary risk factor for the development of postoperative ureteral stenosis [18].The recent systemic review and meta-analysis of 12 randomized controlled trials reported a statistically significant lower rate of ureteral injury in patients undergoing PCNL compared to ureterolithotripsy for large proximal ureteral stones [19].Nonetheless,the stricture rate of the affected ureters was not statistically different[19].In our cohort,with a minimum follow-up period of 6 months,no ureteral stricture has been developed in any of the patients.
It can be argued that the non-papillary puncture is not the standard of care and the approach might be associated with the increased risk of bleeding complications.The basis for those beliefs comes from anatomical studies of Sampaio et al.[20-22]reporting a significantly higher risk of vessel injury when a non-fornical puncture was undertaken.Nevertheless,the clinical studies on non-papillary punctures have demonstrated their comparable safety and efficiency for standard and mini-PCNL including complex renal stones with multiple PCNL tracts [23-26].
Our study had several limitations.In our cohort,all patients were operated in the prone position.Whether npPCNL can be safely applied to a supine position should be further evaluated.Other criticisms can be the low number of patients,the absence of any comparison group,and its retrospective nature.Although we performed a postoperative follow-up imaging at 6-month,we acknowledge that a longer follow-up examination exceeding 1-year would have been more accurate to evaluate the development of ureteral strictures.Future studies with a larger sample size comparing our technique with a retrograde URS,as well as with a papillary PAUL technique are warranted.Finally,the retrospective nature of our study may represent an additional limitation.Nevertheless,we believe that our standardized protocols for data collection and recording minimize the latter bias.
Notwithstanding the aforementioned limitations,our preliminary results studied the feasibility of performing npPCNL for proximal large ureteral stones for the first time demonstrating a high efficiency and safety profile.
5.Conclusion
The npPCNL provides a straight route to the ureteropelvic junction and proximal ureter.Approaching from a dilated portion of the ureter under low irrigation pressure with larger diameter instruments results in effective and safe stone extraction within a few minutes.
Author contributions
Study concept and design: Arman Tsaturyan,Evangelos Liatsikos,Panagiotis Kallidonis.
Data acquisition: Arman Tsaturyan,Constantinos Adamou,Konstantinos Pagonis.
Data analysis: Lusine Musheghyan,Theofanis Vrettos.
Drafting of manuscript: Arman Tsaturyan,Angelis Peteinaris,Anastasios Natsos.
Critical revision of the manuscript: Constantinos Adamou,Konstantinos Pagonis,Lusine Musheghyan,Theofanis Vrettos,Evangelos Liatsikos,Panagiotis Kallidonis.
Conflicts of interest
The authors declare no conflict of interest.
Appendix A.Supplementary data
A video abstract is available online at https://doi.org/10.1016/j.ajur.2022.01.006.
杂志排行
Asian Journal of Urology的其它文章
- Transurethral resection of bladder tumor:A systematic review of simulator-based training courses and curricula
- Etiology and management of urethral calculi:A systematic review of contemporary series
- Oncologic outcomes with and without amniotic membranes in robotic-assisted radical prostatectomy: A propensity score matched analysis
- Single nucleotide polymorphism within chromosome 8q24 is associated with prostate cancer development in Saudi Arabia
- The risk of prostate cancer on incidental finding of an avid prostate uptake on 2-deoxy-2-[ 18F]fluoro-D-glucose positron emission tomography/computed tomography for non-prostate cancer-related pathology:A single centre retrospective study
- Prevention of thromboembolic events after radical prostatectomy in patients with hereditary thrombophilia due to a factor V Leiden mutation by multidisciplinary coagulation management
