The risk of prostate cancer on incidental finding of an avid prostate uptake on 2-deoxy-2-[ 18F]fluoro-D-glucose positron emission tomography/computed tomography for non-prostate cancer-related pathology:A single centre retrospective study
2024-02-25AnthonyFrnklinTroyGinuzzoBoonKuDviWongLouisMcEwnJmsWltrsRchlEslrMtthwRobrtsGoffCoughlinJohnYxly
Anthony Frnklin,Troy Ginuzzo,Boon Ku,Dvi Wong,Louis McEwn,Jms Wltrs,Rchl Eslr,,Mtthw J.Robrts,Goff Coughlin,John W.Yxly,,*
a Department of Urology,The Wesley Hospital,Brisbane,QLD,Australia
b Wesley Medical Research,Brisbane,QLD,Australia
c School of Medicine,The University of Queensland,Brisbane,QLD,Australia
d Department of Radiology,Wesley Medical Imaging,Brisbane,QLD,Australia
e Department of Urology,Royal Brisbane and Women’s Hospital,Brisbane,QLD,Australia
KEYWORDS Prostate cancer;Position emission tomography;Multiparametric magnetic resonance imaging;Prostate biopsy
Abstract Objective: To review the risk of prostate cancer(PCa) in men with incidentally reported increased intraprostatic uptake at 2-deoxy-2-[ 18F]fluoro-D-glucose positron emission tomography/computed tomography ( 18F-FDG PET/CT) ordered at Department of Urology,The Wesley Hospital,Brisbane,QLD,Australia for non-PCa related pathology.Methods: Retrospective analysis of consecutive men between August 2014 and August 2019 presenting to a single institution for 18F-FDG PET/CT for non-prostate related conditions was conducted.Men were classified as benign,indeterminate,or malignant depending of the results of prostate-specific antigen (PSA),PSA velocity,biopsy histopathology,and three-Tesla(3 T) multiparametric MRI (mpMRI) Prostate Imaging Reporting and Data System score,or gallium-68-prostate-specific membrane antigen ( 68Ga-PSMA) PET/CT results.Results: Three percent(273/9122)of men demonstrated 18F-FDG avidity within the prostate.Eighty-five percent (231/273) were further investigated,including with PSA tests (227/231,98.3%),3 T mpMRI(68/231,29.4%), 68Ga-PSMA PET/CT (33/231,14.3%),and prostate biopsy(57/231,24.7%).Results were considered benign in 130/231 (56.3%),indeterminate in 31/231(13.4%),and malignant in 70/231 (30.3%).PCa was identified in 51/57(89.5%)of the men who proceeded to biopsy,including 26/27(96.3%)men with Prostate Imaging Reporting and Data System scores 4-5 mpMRI and six men with a positive 68Ga-PSMA PET/CT.The most common Gleason score on biopsy was greater than or equal to 4+5(14/51,27.5%). 68Ga-PSMA PET/CT was concordant with the 18F-FDG findings in 26/33(78.8%).All 13 men with a positive concordant 18F-FDG,3 T mpMRI,and 68Ga-PSMA PET/CT had PCa on biopsy.There was no statistically significant difference in the 18F-FDG maximum standardized uptake value between the benign or malignant groups(5.7 vs.6.1;p=0.580).Conclusion: In this study,after an incidental finding of an avid intraprostatic lesion on 18F-FDG PET/CT,70 of the 231 cases(30.3%;0.8% of the entire cohort)had results consistent with PCa,most commonly as Gleason score greater than or equal to 4+5 disease.Unless there is limited life expectancy due to competing medical co-morbidity,men with an incidental finding of intraprostatic uptake on 18F-FDG should be further investigated using principles of PCa detection.
1.Introduction
Within oncology,2-deoxy-2-[18F]fluoro-D-glucose (18F-FDG)is the most commonly used radiotracer for positron emission tomography/computed tomography (PET/CT) imaging[1].18F-FDG is taken up by high-glucose-using cells,which can be physiologic,inflammatory,or malignancy in aetiology.Within malignant cells,this is due to shifted energy production from mitochondrial respiration to glucose metabolism,a near-universal phenomenon known as the Warburg effect [2].18F-FDG PET/CT is commonly utilised for the staging and restaging of various non-prostate malignancies[3].Clinicians can be faced with the challenge of interpreting foci of increased18F-FDG uptake in unexpected locations including the prostate [4].Multiple studies have shown a lack of clinical utility of18F-FDG PET/CT in the evaluation of men with prostate cancer(PCa) [5,6].This is because PCa does not undergo aerobic glycolysis,but instead relies on metabolism of lipids and other energetic molecules [7].However,use of18F-FDG PET/CT has been shown to detect additional disease and improve patient selection for radioligand therapy in castrate-resistant disease [8,9].
For primary tumours,incidental prostate18F-FDG uptake is relatively uncommon,reported to be 1.8% according to a systematic review with meta-analysis of 47 925 patients[10].Of the 121 men who proceeded to biopsy,62% were diagnosed with PCa.Current publications present conflicting findings with regards to the significance and appropriate workup of men with incidental18F-FDG uptake within the prostate.The significance of finding an incidental avid prostate area on18F-FDG PET/CT and a decision to further investigate is balanced against the prognosis of the primary condition.
The aim of this study was to review a contemporary cohort of men with incidental18F-FDG intraprostatic uptake on PET/CT at our institution and review what urological workup was performed to differentiate between a benign or malignant intraprostatic18F-FDG focus.We also aimed to examine the significance of the18F-FDG PET/CT intensity and the findings on subsequent analysis with a three-Tesla(3 T) multiparametric MRI (mpMRI) and analyse concordance with gallium-68 prostate-specific membrane antigen(68Ga-PSMA) PET/CT and finally the histological results of men who proceeded with prostate biopsy.
2.Patients and methods
2.1.Methods
Ethics approval was obtained for this retrospective study from the UnitingCare Health Human Research Ethics Committee(study reference:2019.32.310)and the requirement to obtain informed consent was waived.We reviewed the images of consecutive patients at the Wesley Hospital,Brisbane,QLD,Australia noted to have incidental prostatic avidity,on18F-FDG PET/CT scans with intravenous contrast-enhanced CT performed for oncologic purposes or medical conditions not related to prostate disease between August 2014 and August 2019.The results of prostate investigations were collected from July 2013 until June 2021.
2.2.Patients
During the study period,16 768 patients including 9122 men underwent18F-FDG PET/CT scans at our institution.No retrospective review of the18F-FDG was performed,with the decision to review patient files based on the original18F-FDG PET/CT report of a suspicious avid focus within the prostate.Men were included for analysis if the18F-FDG avid area within the prostate was described as statements including abnormal,focal intense,suspicious,or prostate investigation suggested.The men with incidental uptake within the prostate on18F-FDG PET/CT had their charts reviewed for investigations relating to PCa including prostate-specific antigen(PSA)levels,3 T mpMRI,68Ga-PSMA PET/CT,or transperineal prostate biopsy(TPBx).If men had more than one18F-FDG PET/CT scan during the study period,incidental prostate findings were only included once.The avid18F-FDG area was classified as benign,indeterminate,or malignant based on subsequent investigations as outlined in Fig.1.
2.3.Outcome classification
Men were classified as malignant if a TPBx confirmed cancer.Men who did not have histopathological confirmation were considered most likely malignant if a 3 T mpMRI Prostate Imaging Reporting and Data System(PIRADS)4-5 lesion was concordant with either an avid lesion on68Ga-PSMA PET/CT,or associated with PSA of more than 20 μg/L[11,12].Men without a 3 T mpMRI or68Ga-PSMA PET/CTscan were classified as malignant if they were commenced on androgen deprivation therapy by their clinician for a clinical diagnosis of PCa[13],or the PSA was persistently greater than 20 μg/L and increasing,or associated with a PSA doubling time(PSADT)of less than 3 years[14].
Men were classified as benign if a TPBx was negative for malignancy.In men without a TPBx,they were also classified as most likely benign if the PSA was less than 2 μg/L,or 2-<3 μg/L associated with a negative 3 T mpMRI(PIRADS 1-2),negative68Ga-PSMA PET/CT,and/or a PSADT greater than 3 years.If the PSA was between 3 μg/L and<10 μg/L without further investigations,this group was categorised as benign if the PSADT is greater than 5 years.The remaining men were classified as an indeterminate-risk of PCa.
For men without further urological investigations of the intraprostatic18F-FDG avid area,the ordering physician was contacted to confirm that further prostate investigation was not performed due to the poor prognosis of the primary condition.
2.4.Imaging modalities
All men underwent18F-FDG PET/CT scans with either the Philips Ingenuity camera (Philips Healthcare,Best,the Nederland) with 128-slice CT or the GE Discovery MI (GE Healthcare,Waukesha WI,USA) with a 128 slice inlay scans.The Philips camera uses time of flight and GE has both time of flight and filtered back projection.The minimum uptake time was 45-60 min following administration of an average injected dose of 300 MBq18F-FDG using 3-4 min frames over 12-13 frames (head,neck,chest,abdomen,and pelvis) with low dose CT for attenuation correction and anatomical localisation scanners within our hospital.The68Ga-PSMA PET/CT scans were performed on the above-described scanner protocol with an average injected tracer dose of 200 MBq of Glu-NH-CO-NH-Lys(Ahx)-HBEDCC.All men had a maximum standardized uptake value(SUVmax)reported.

Figure 1 Flow diagram of distribution of groups by definitions. 18F-FDG,2-deoxy-2-[ 18F]fluoro-D-glucose;PET/CT,positron emission tomography/computed tomography;PSA,prostate-specific antigen;mpMRI,multiparametric MRI; 68Ga-PSMA,Gallium-68 prostate-specific membrane antigen;TPBx,transperineal prostate biopsy;PSADT,PSA doubling time;PIRADS,Prostate Imaging Reporting and Data System;ADT,androgen deprivation therapy;3 T,three-Tesla.
All patients’3 T mpMRI scans included T2 weighted,diffusion weighted (b1400) and Gadolinium contrast-enhanced image sequence,and T1 weighted images (Skyra;Siemens healthcare,Erlingen,Germany).All mpMRI scans were performed prior to the TPBx as per the protocol at our hospital for many years.The images were reported using PIRADS version 1 and subsequently version 2 by experienced radiologists,with Wesley Medical Imaging reporting between 180 mpMRI and 200 mpMRI prostate scans per month.The second read was performed by the treating urological surgeon and discussed at the uro-radiology multidiscipline meeting if there was discordance between the findings.If no TPBx was performed,men were only considered for assessment as malignant if they hadatleasttwoofthefollowingabnormalities:an abnormal 3 T mpMRI,68Ga-PSMA PET/CT,and/or very high PSA(>20 μg/L).
2.5.Histopathological analysis
On cognitive fusion TPBx histology,the location and number of biopsy cores taken in each case and the number of cores positive for carcinoma were recorded [15].The extent of cancer in each core was given as a percentage,cancer length in millimetres,or both.A Gleason score was recorded for each core.During the study period,the Gleason score reflected the changes in cancer grading based on the grading criteria of the modified Gleason grading system[16]and the 2014 International Society of Urological Pathology grading system [17].
The prostatectomy specimens were handled according to established protocols at the uropathology centre.Prior to sectioning,each prostate gland was weighed and measured.The prostate gland was sectioned and embedded in its entirety.The body of the prostate was sectioned at 3-4 mm intervals in a transverse plane perpendicular to the rectal surface.
2.6.Statistical analysis
Descriptive statistics were performed using Microsoft Excel Professional Plus 2013 (Windows 10 Enterprise;Microsoft,Redmond,WA,USA) and IBM SPSS version 25 (IBM,Armonk,NY,USA).The Mann-WhitneyU-test was undertaken to determine if the SUVmaxbetween benign and malignant groups was statistically significant,with a significantp-value set at less than 0.05.
3.Results
3.1.Screening results of patient population
Of the 9122 men who underwent18F-FDG PET/CT for oncologic purposes not related to prostate disease at our institution between August 2014 and August 2019,273 (3.0%) men were identified as having incidental focal intraprostatic18F-FDG avidity within the prostate gland and had no known history of PCa.The median age was 74(range 32-97) years.The median PSA was 3.6 μg/L (range 0.07-100.0 μg/L,interquartile range [IQR]1.3-7.3 μg/L).The most common indications for18F-FDG PET/CT were lymphoma (69/273,25.3%),lung cancer (67/273,24.5%),and colorectal cancer (43/273,15.8%).
3.2.Follow-up investigations for PCa
Two-hundred and thirty-one(231/273;84.6%) men had PCa investigations within 1 year of their18F-FDG PET/CT as seen in Table 1 (median follow-up 3.6 years,range 1.0-6.1 years).The majority of the cohort had PSA results available(227/231,98.3%).A 3 T mpMRI was performed in 29.4%(68/231)men,including four men without an accompanying PSA level.A68Ga-PSMA PET/CT scan was performed in 14.3% (33/231) men and a TPBx of the prostate in 24.7%(57/231) men.The median number of TPBx biopsy cores was 21(range 16-31),including cognitively guided biopsies of the18F-FDG avid area.The median number of positive cores was 9 (range 4-14).The median time between18F-FDG PET/CT and first subsequent PCa-related investigation was 12 weeks.Of the 57 men that proceeded with prostate biopsy,35 were investigated with a pre-biopsy mpMRI,of which 27 had a PIRADS 4-5 lesion.The treating physicians confirmed 42 men were not investigated for their abnormal18F-FDG PET/CT prostate avidity because of the poor prognosis of their primary malignancy,the long-term outcome of which would not be altered by a diagnosis or treatment of PCa.
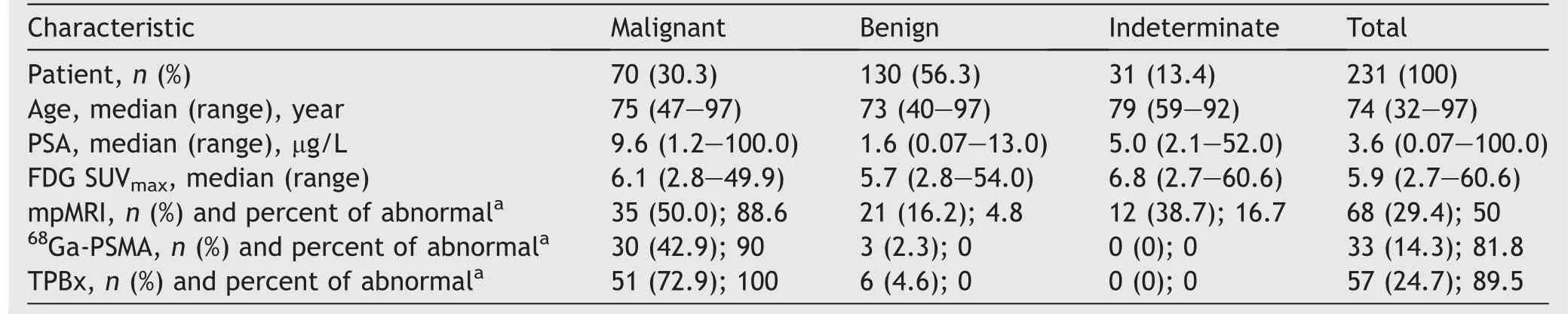
Table 1 Summary of outcomes between groups (n=231).
3.3.Cancer classification
Overall,30.3%(70/231) men met inclusion criteria for PCa.The median age was 75(range 47-97)years and the median PSA was 9.6(range 1.2-100.0)μg/L.The median SUVmaxon18F-FDG PET/CT was 6.1 (range 2.8-49.9,IQR 4.6-8.3),with 87.1% (61/70) demonstrating focal peripheral zone avidity.TPBx was performed in 57 men,of which 51(89.5%)were diagnosed with prostate adenocarcinoma.Six of the 22 (27.3%) men with a PSA greater than 20 μg/L proceeded to biopsy,all of which were positive for malignancy.Among 227 men with available PSA results,98 had a PSA of less than 3.0 μg/L and 28 proceeded to further investigations with either prostate biopsy,mpMRI,and/or PSMA.Only 6.1% (6/98) of men with low PSA were proven to have PCa following prostate biopsy.Ductal carcinoma in addition to adenocarcinoma was identified in 3.9% (2/51)participants,one at prostate biopsy,and another found on robotic-assisted laparoscopic radical prostatectomy (RALP)histology.The median Gleason score was 4+3;however,Gleason score ≥4+5 was the most frequently diagnosis (14/51,27.5%).During the follow-up period,15 men underwent RALP with all histopathology demonstrating Gleason score ≥3+4 PCa (median Gleason score 4+3) and most being localised to the prostate (median pT2,range pT2-pT3b).
Of the 27.1% (19/70)men considered malignant who did not undergo TPBx,36.8%(7/19)had an abnormal 3 T mpMRI,68Ga-PSMA PET/CT,and/or very high PSA (>20 μg/L)(2+criteria required).About 57.1% (4/7) men with an abnormal 3 T mpMRI demonstrated PIRADS 5 lesions;85.7% (6/7) also had an abnormal concordant68Ga-PSMA PET/CT;and all but one(6/7,85.7%)had a PSA greater than 20 μg/L.
Of the 17.1% (12/70) remaining men considered likely malignant,50.0% (6/12) had a persistent PSA of greater than 20 μg/L.One commenced androgen deprivation therapy for a clinically malignant prostate and the remaining five had a median PSADT of 1.0 (range 0.2-2.9) years.A 95-year-old gentleman had a PSA of 100 μg/L and a further five men with a PSA between 10 μg/L and 20 μg/L (median 15.0 μg/L) had a median PSADT of 1.1 years.
3.3.1.Clinically significant PCa
Of the 51 men with biopsy proven PCa,84.3% (43/51) had Gleason score ≥3+4 PCa.Gleason score ≥4+5 PCa was most frequently diagnosed (14/51,27.5%),followed by Gleason score 3+4 (13/51,25.5%) PCa,and then Gleason score 4+3 (10/51 19.6%) PCa.We did not find a correlation between the SUVmaxon18F-FDG PET/CT and the Gleason score on TPBx (r=¯0.0961,p=0.48,Table 2).Twenty-three (23/51,45.1%) men were treated with either a RALP (15/51,29.4%),radiation therapy (7/51,13.7%),or focal therapy with NanoKnife irreversible electroporation(1/51,2.0%).Five (5/51,9.8%) men were managed with androgen deprivation therapy.Of the 125 men aged over 75 years,22 were proceeded to biopsy.Only two were benign;two had low-grade disease;and 18 (18/22,81.8%) had Gleason score of greater than or equal to 3+4 prostate adenocarcinoma.

Table 2 Relationship between SUVmax on FDG PET and Gleason score on biopsy.
3.3.2.Benign classification
About 56.3% (130/231) men were classified as benign according to our classification.On average,they were 2 years younger than men with PCa(median 73 years,range 40-97 years;p=0.0114),and had a lower median PSA (median 1.6 μg/L,range 0.07-13.0 μg/L;p<0.001)and more central zone avidity (57/130,43.8%,p<0.001).The median18F-FDG SUVmaxwas 5.7 (range 2.8-54.0,IQR 4.4-8.4),which was not statistically different to the malignant group(median SUVmax6.1) (p=0.580).
About 4.6% (6/130) men had benign histology on TPBx and 56.2% (73/130) men had very low PSA (<2.0 μg/L).There were an additional 10.0% (13/130) men who had a PSA between 2 μg/L and 3 μg/L of whom 10 had a PSADT of greater than 3 years and three had a low risk 3 T mpMRI(PIRADS 1-2).Of 130 men,38 (29.2%) men with a PSA between 3 μg/L and 10 μg/L had long PSADT of greater than 5 years and were therefore considered most likely benign,or at low risk of a clinically significant malignancy.
3.3.3.Indeterminate for malignancy
Totally 13.4% (31/231) men were unable to be categorised into benign or malignant groups and were therefore classified as indeterminate.The median PSA was 5.0 (range 2.1-52.0)μg/L.About 9.7%(3/31)men with a PSA of greater than 20 μg/L had no further urological investigations;38.7%(12/31)had 3 T mpMRI scans performed in this cohort,of which 83.3%(10/12)were normal(PIRADS 1-2).Two had abnormal high-risk PIRADS 5 lesions,but unfortunately,there was insufficient further supporting PSA data or other investigations to meet our malignant or benign criteria.
For men with only PSA data(19/31,61.3%),10.5%(2/19)had low PSA values (2-3 μg/L) with PSADT (less than 3 years).There were 63.2% (12/19) men with PSA values between 3 μg/L and 10 μg/L (median 5.8 μg/L,range 3.2-9.2 μg/L) who had a median PSADT of 2.6 (range 1.3-4.6) years.
3.4.Correlative imaging
3.4.1.Outcomes with 68GA-PSMA PET/CT
About 14.3% (33/231) men had both a68Ga-PSMA PET/CT and a18F-FDG PET/CT scan:90.9%(30/33)were classified as malignant based on a positive biopsy (24/30,80.0%),PIRADS 5 mpMRI (3/30,10.0%),or a PSA of greater than 20 μg/L (3/30,10.0%).The median SUVmaxon68Ga-PSMA PET/CT of the men with PCa was 8.4 (range 1.5-37.9)compared to 2.7 (range 2.4-3.4) for those men without PCa.The68Ga-PSMA PET/CT was positive in 84.8% (28/33)men and 78.8% (26/33) had lesions concordant with the18F-FDG PET/CT findings.Prostate biopsies were performed in 75.8% (25/33),of which 96.0% (24/25) confirmed PCa,with Gleason score of greater than or equal to 4+5 being the most common (7/25,28.0%) histological diagnosis.Five of the thirty-three men who had both PET/CT had a negative68Ga-PSMA PET/CT study.Of these five men,four underwent TPBx of which 75.0% (3/4) confirmed PCa.Six of the 231 (2.6%)18F-FDG scans had evidence suggestive of likely prostate metastatic disease based on bony metastatic distribution classical for PCa.Three of the six men also underwent PSMA PET,which all demonstrated disease concordant with18F-FDG PET/CT,as well as additional metastatic disease identified with one man on PSMA compared to18F-FDG PET/CT.
3.4.2.Outcomes with 3 T mpMRI
The 3 T mpMRI was performed in 64.9% (37/57) men who proceeded to prostate biopsy.All 15 PIRADS 5 on 3 T mpMRI and 91.7% (11/12) PIRADS 4 scans had biopsy proven PCa.However,62.5%(5/8)of PIRADS less than or equal to 3 were also positive on prostate biopsy.About 90.9% (30/33) of mpMRIs demonstrating PIRADS 4-5 lesions were concordant with their18F-FDG findings.
3.4.3.Outcomes with both 68Ga-PSMA PET/CT and 3 T mpMRI
Both68Ga-PSMA PET/CT and 3 T mpMRI were performed in 10.0% (23/231) men,of which 69.6% (16/23) were concordant.TPBx was performed in 81.2% (13/16) men and all 13 were positive for PCa,with a positive predictive value of 100% for the combination of18F-FDG,3 T mpMRI,and68Ga-PSMA PET/CT.The concordance between the18F-FDG PET/CT scan and subsequent urological specific investigations are outlined in Table 3.
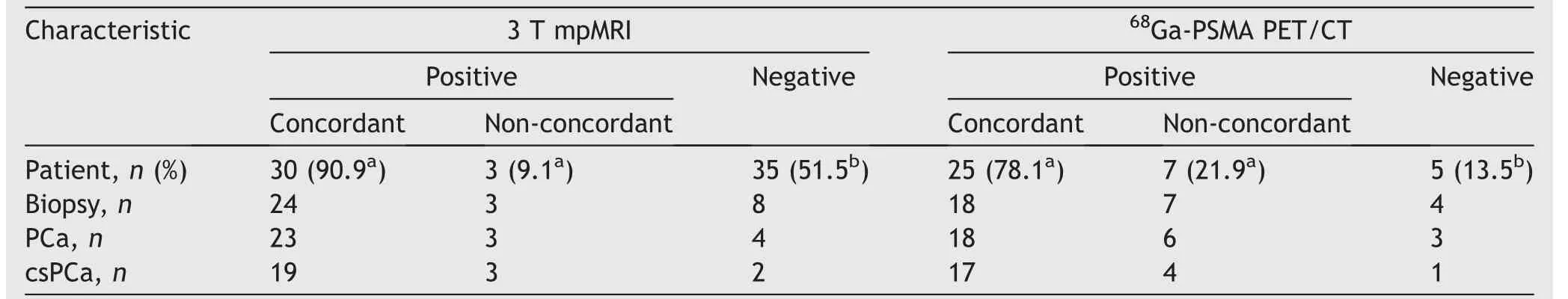
Table 3 Concordance between prostate findings on 18F-FDG,mpMRI,and 68Ga-PSMA PET/CT.
4.Discussion
We identified an incidental intraprostatic avid area in 3% of the 9122 men who were investigated,which is similar to other series [3,4,18].Malignancy was confirmed on biopsy or highly likely based on a combination of 3 T mpMRI,PSA,and68Ga-PSMA PET/CT in 30.3%(70/231),or 0.8%(70/9122)of the entire cohort.These are consistent with the findings of Reesink et al.[19]on cysto-prostatectomy of 43 men with incidental intraprostatic18F-FDG PET/CT avid lesions on PET/CT identified following investigation of bladder cancer.The most common histological diagnosis was high-grade Gleason score of greater than or equal to 4+5 adenocarcinoma.68Ga-PSMA PET/CT was concordant with the18F-FDG PET/CT findings in 78.8%.The PSA levels were predictably higher in the malignant cohort (9.6 μg/Lvs.1.6 μg/L),but there was no statistically significant difference between the SUVmaxof the malignant and benign groups in this primary diagnostic setting.When a 3 T mpMRI scan identifies a PIRADS 4-5 lesion,or a68Ga-PSMA PET/CT identifies a suspicious and concordant avid lesion,there is a very high probability of PCa on biopsy(91.7%-100.0%)[20].
In the systematic review and meta-analysis of 444 men by Bertagna et al.[10],the risk of malignancy was estimated at 17%,increasing to 65% in the 121 men that proceeded to prostate biopsy.In one of the largest published multicentre series of 280 men with incidental prostate uptake,PCa was identified on biopsy in 55.6% (35/63) [21].We found a higher risk of PCa on biopsy(89.5%,51/57)than other publications,which may represent different physician indications for biopsy,particularly in the era of 3 T mpMRI and68Ga-PSMA PET/CT.
In our cohort,high-grade Gleason score of greater than or equal to 4+5 cancer was identified in 27.5% of patients.This is higher than the 16% of men with high-grade cancer diagnosed on TPBx [22],or on radical prostatectomy histology(16.8%)at our institution [23].These suggest that FDG positive cancer could be associated with a higher-grade malignancy;therefore,the finding of an incidental intraprostatic FDG avid area should be investigated.In men with PCa,18F-FDG PET/CT intraprostatic uptake has been associated with higher grade prostate malignancy[1,24,25],higher risk of post-surgery progression [26],and also progression to metastatic castrate resistant PCa [27].In men with high-grade Gleason score(≥8)cancer,intraprostatic18F-FDG uptake with the SUVmaxof greater than 4.6 is associated with twice the risk of biochemical recurrence following surgery[1].However,in the incidental primary diagnostic setting,the significance of intraprostatic18F-FDG PET/CT uptake remains uncertain,and the ability of the SUVmaxto differentiate between benign and malignant is not robust[4-6].In the series by Hwang et al.[5],65.2% (120/184) men had further evaluation and TPBx was performed in 31.7% (38/120).PCa was identified in 19.2% (23/120) of the evaluated men,including 60.5% (23/38) who proceeded with biopsy.There was no statistical difference in the SUVmaxin the cancer group compared to the benign group(mean 5.7 [standard deviation,SD 5.1]vs.4.8 [SD 2.7],p=0.37).In our series,we also found no difference in the18F-FDG SUVmaxbetween men classified as malignant versus benign (median 6.1 [IQR 4.6-8.3]vs.5.7 [IQR 4.4-8.4],p=0.58).Therefore,in the diagnostic setting there is no useful18F-FDG SUVmaxthat can be recommended to triage which men will require a prostate biopsy.
Of those who did not proceed to biopsy,there was varying repeat18F-FDG PET/CT undertaken including many(68.8%) with PSA less than 1 μg/L demonstrated ongoing intraprostatic avidity.This is suggestive that many men display non-malignant causes for FDG avidity within the prostate,which is in keeping with our cohort where 70% were not classified as malignant.It is very unlikely that these changes reflect intraprostatic metastases related to the primary malignancy due to its rarity and none of the patients biopsied in our study had non-primary prostate malignancy.
There is lack of international consensus regarding what PSA level correlates with benign pathology.Our criteria of a PSA less than 2 μg/L is based on nomogram data showing that approximately 90% of men with a PSA of less than 2 μg/L had benign histology on prostate biopsies [28].PCa on biopsy of men with incidental18F-FDG uptake with a PSA of less than 2.5 μg/L was identified in only 3.8% in the biopsy series of 99 men by Kwon et al.[3].Minamimoto et al.[29]evaluated the outcome of a 12-core systematic TPBx in 50 men with18F-FDG avid prostate lesions.PCa was diagnosed in 25 (50.0%),with the highest odds ratio for PCa diagnosis at a PSA cut-off at 12.0 (odds ratio 10.77,95% confidence interval 2.78-48.78)μg/L and a PSA of less than 2 μg/L highly unlikely to be associated with finding PCa in a18F-FDG avid intraprostatic lesion.When considering a traditional PSA cut-off for investigation of less than 3.0 ug/L,of the 28 men investigated,21.4% (6/28)had biopsy proven PCa,and only 3.6%(1/28)had a high-grade PCa.Therefore,if the PSA is less than 3.0 ug/L,it would seem appropriate to avoid any further investigation unless there are risk factors such as family history,concerning PSA velocity,abnormal digital rectal examination,or other clinical factors.
Using a 3 T mpMRI alone to establish the diagnosis of PCa without histological confirmation in an18F-FDG PET/CT avid area is contentious.However,in the PSA screening population,PCa was diagnosed in 73.0%-85.0% and 92.0%-95.2% of men with a 3 T mpMRI of PIRADS 4 and 5,respectively,at our institution [15].In a small series comparing the whole gland histological sector analysis of 17 men,the combination of incidental18F-FDG PET/CT prostate uptake and abnormal mpMRI had a positive predictive valve for malignancy of 0.83 [30].Our results showed that 96.3%(26/27) men with a PIRADS 4-5 mpMRI that proceeded to biopsy had PCa.In our current series,we also required a high PSA or abnormal68Ga-PSMA PET/CT to accompany the PIRADS 4-5 lesion before considering the18F-FDG PET/CT avid lesion as likely to be malignant.Recently the PRIMARY study has demonstrated that 97% of cases were mpMRI and68Ga-PSMA PET/CT positive,and that PCa was identified at biopsy [20].
The limitations of the study include the retrospective data collection and inconsistencies due to the large cohort(biopsy confirmation,clinical staging,and clinical information such as immune or testosterone suppression and urological history).We were unable to reliably determine the18F-FDG PET/CT indications (e.g.,primary investigation of non-prostate pathology and treatment response)or perform blinded image review.It is possible but unlikely that FDG uptake in men considered benign due to PSA less than 2.0 ug/L could be due to high-grade (e.g.,ductal variant is very rare) [31].Furthermore,15.4% of men suspected to have PCa were not confirmed,likely due to treating physician discretion (e.g.,poor life expectancy not warranting a diagnosis).While lack of histological diagnosis is a limitation,abnormal mpMRI result was used for cancer classification,without biopsy,due to the high performance of mpMRI for PIRADS 4 (73%-85%) and PIRADS 5 (89.8%-90.5%) findings in our institution,also providing confidence in the T3 rate (8/68,11.8%) [15].Similarly,68Ga-PSMA PET/CT was used due to high concordance with significant cancer,enhanced in combination with mpMRI (97.9% of all clinically significant index lesions according to prostatectomy histology) [32].Conversely,the potential for false positive cancer classification with the imaging criteria is offset by the indeterminate classification where underlying PCa may be present.Finally,we included PSADT as a criterion as it is a dynamic model of prostate tumour biology which,when low (<3 years),is predictive of aggressive disease[14,33,34]and,when high (>4 years),is associated with a low-risk progression on active surveillance [35].However,PSADT is limited by unclear accuracy in predicting untreated PCa progression [36]and diagnosis [37].
5.Conclusion
In view of our findings,it is recommended that men with incidental18F-FDG PET/CT intraprostatic uptake be referred for further urological investigation including a digital rectal examination and a PSA test,providing their primary malignancy does not limit short-to intermediate-term life expectancy.If further investigation is required,our results show that a combination of an avid18F-FDG PET/CT with a concordant68Ga-PSMA PET/CT and a PIRADS 4-5 on 3 T mpMRI is associated with a 100% probability of a histological diagnosis of PCa.This finding requires further prospective evaluation with larger patient cohorts.
Author contributions
Study concept and design: Anthony Franklin,John W.Yaxley,Troy Gianduzzo.
Data acquisition:Anthony Franklin,David Wong,Boon Kua,Geoff Coughlin.
Data analysis: Anthony Franklin,John W.Yaxley,Matthew J.Roberts.
Drafting of manuscript: Anthony Franklin,John Yaxley,Troy Gianduzzo,Matthew J.Roberts,Rachel Esler,Louise McEwan,James Walters.
Critical revision of the manuscript: Anthony Franklin,Troy Gianduzzo,Boon Kua,David Wong,Louise McEwan,James Walters,Rachel Esler,Matthew J.Roberts,Geoff Coughlin,John W.Yaxley.
Conflicts of interest
The authors declare no conflict of interest.
杂志排行
Asian Journal of Urology的其它文章
- Transurethral resection of bladder tumor:A systematic review of simulator-based training courses and curricula
- Etiology and management of urethral calculi:A systematic review of contemporary series
- Oncologic outcomes with and without amniotic membranes in robotic-assisted radical prostatectomy: A propensity score matched analysis
- Single nucleotide polymorphism within chromosome 8q24 is associated with prostate cancer development in Saudi Arabia
- Prevention of thromboembolic events after radical prostatectomy in patients with hereditary thrombophilia due to a factor V Leiden mutation by multidisciplinary coagulation management
- Transurethral prostate surgery in prostate cancer patients: A population-based comparative analysis of complication and mortality rates
