Does local vaginal estrogen after tension-free transobturator vaginal tape reduce overactive bladder symptoms in postmenopausal women? A prospective randomized,controlled study
2024-02-25SmerMhmoudMorsyDliFroukSrHssnAhmedYehiAdelzizHusseinAlyHussein
Smer Mhmoud Morsy,Dli Frouk ,Sr Hssn ,Ahmed Yehi Adelziz ,Hussein Aly Hussein
a Urology Department,Kasr Al Ainy Hospital,Cairo University,Cairo,Egypt
b Obstetrics and Gynecology Department,Kasr Al Ainy Hospital,Cairo University,Cairo,Egypt
KEYWORDS Stress urinary incontinence;Estrogen;Midurethral sling;Overactive bladder symptom
Abstract Objective: We aimed to evaluate the efficacy of topical estrogen after transvaginal tension-free vaginal tape-obturator (TVT-O) in the treatment of de novo overactive bladder symptoms that appear after surgery.Methods: This is a prospective randomized controlled study performed in the Urology and Gynecology Departments,Kasr Al Ainy Hospital,Cairo University,Cairo,Egypt.Two hundred and ten postmenopausal females presenting during the period between January 2017 and November 2020 with stress urinary incontinence were included in the study.Patients were divided into two groups,105 patients in Group A (treatment group) and 105 patients in Group B(control group).Patients in Group A underwent transvaginal TVT-O followed by local vaginal estrogen treatment for 6 months,while patients in Group B underwent transvaginal TVT-O only.The study included any postmenopausal female with urodynamic stress urinary incontinence.All patients had to fulfill a 3-day bladder diary,overactive bladder symptoms score,urine analysis,urodynamic study,and post-voiding residual urine measurement by abdominal ultrasound preoperatively and at 3-month and 6-month follow-ups.Results: At 6-month follow-up,daytime frequency was reduced to 8% in Group A (increased to 21% in Group B)with a statistically significant difference between both groups(p=0.009).At 6-month follow-up,nocturia was 8% in Group A (11% in Group B) with no statistically significant difference between both groups(p=0.469).There was a statistically significant difference between both groups as regards to urinary urgency at 6-month follow-up(p=0.024).There was a statistically significant difference in postoperative wound healing events as regards to cure,hyperemia,gapping,and wound infection 1 week after intervention between both groups (p=0.008).No local or systemic side-effects were reported from local estrogen use.Conclusion: Local vaginal estrogen treatment given to postmenopausal patients after midurethral sling procedures can reduce the symptoms of daytime frequency and urinary urgency.Long-term follow-up is needed.
1.Introduction
During the menopausal period,estrogen deficiency results in weakness in pelvic floor muscles and increases the complaint of stress urinary incontinence (SUI).It is a common bladder control abnormality encountered during the menopausal period [1].Through the control of collagen synthesis and breakdown,estrogen receptors play a role in the supportive mechanism of the pelvis[2].The supporting connective tissue of pelvic organs is estrogen responsive[3].Epidemiologic studies confirm that menopause is a direct cause for the development of pelvic floor disorders[4].Moreover,with increasing age during menopausal period,bladder dysfunctions develop,which results in the decrease of bladder capacity.Depending on the decrease in estrogen level,the decrease of the tonus of sphincters and the closing capacity of the urethral lumen are associated with the decrease of urethra length and hypermobility in case of stress [5].
Anti-incontinence treatments as mid-urethral sling(MUS) and tension-free vaginal tape (TVT) are both efficient surgical treatment options [6].MUSs have widely been considered as the corner stone in the management of SUI [7].Curative rates in women undergoing transobturator repair reach 62%-98%.After 5 years,the curative rates range from 43% to 92% with a transobturator approach [8].
Despite the success of these procedures for treatment of SUI [9],they do not always cure urge symptoms [6].In addition,the incidences ofde novourgency and urgency urinary incontinence (UUI) are reported around 15% and 30%,respectively [10].This could be explained by many hypotheses.First,despite the fact that these slings are theoretically tension-free,the fixed mesh may have undesirable effects on the mobility of the urethra and the dynamics of voiding in a way that could affect voiding and storage symptoms [11].Second,after using transvaginal ultrasound,it was found that postoperative UUI and daytime frequency were more likely to be associated with those slings positioned more distally than those placed at the mid-urethra [12].Our main aim was to evaluate the efficacy of topical estrogen after transvaginal TVT-obturator (TVT-O) in the treatment ofde novooveractive bladder (OAB) symptoms that appear after surgery.
2.Patients and methods
2.1.Study design
This is a study performed in Urology and Gynecology Departments,Kasr Al Ainy Hospital,Cairo University,Cairo,Egypt.After full explanation of the study protocol,the patients gave the written informed consents.Local Ethics Committee approved the study protocol (approval number I17009).The sample size was estimated based on evidence from Liapis et al.[6]study using the comparisons of the incidences of daytime frequency and nocturia in estrogentreated group and the non-estrogen-treated group as primary outcomes.Power and sample size program was used to calculate the sample size.Assuming 80% power,0.05 level of significance,the proportion of daytime frequency and nocturia in non-estrogen-treated group was 8.7 and 4.4 compared to 4.3 and 2.2 in the estrogen-treated group,respectively,and with ratio of equal size (ratio: 1:1).The minimum required sample size to detect statistical significance difference was 142 participants (71 in each group).Finally,105 patients in each arm were included in our study for expected dropout.
2.2.Study population
Postmenopausal females presenting during the period between January 2017 and November 2020 with SUI to our urology and gynecology clinics were recorded to call them for their interventions.Patients were randomly assigned to estrogen-treated group (Group A,treatment group) and non-estrogen-treated group(Group B,control group)using a computer-generated random number generator with a 1:1 ratio done by an independent statistician.Patients in Group A underwent TVT-O followed by local vaginal estrogen treatment for 6 months,while patients in Group B underwent TVT-O only.Exclusion criteria were mixed urinary incontinence,UUI,cystocele more than Grade 2,neurological abnormalities,any detrusor overactivity,diabetics,and recurrent vaginal surgeries.
2.3.Measurements
All patients were asked to fulfill 3-day bladder diary.We considered OAB symptoms if mean urgency episodes were equal to or more than 2,frequency equal to or more than 8 per 24 h and/or nocturia episodes more than once at night.OAB symptom score is a symptom assessment questionnaire that aims to quantify OAB symptoms into a single score.Daytime frequency was given 2 points;nighttime frequency was given 3 points;urinary urgency was given 5 points;and UUI was given 5 points.The total scores range from 0 to 15 points,with higher scores indicating higher symptom severity [13].Treatment of any urinary tract infection was detected by urine analysis: urodynamic study (uroflow,filling,and voiding cystometry),post-voiding residual urine measurement by abdominal ultrasound preoperatively and at 3-and 6-month follow-ups.The patients were considered postmenopausal if menstruation had stopped for 1 year or more.Our primary outcomes were to assess the incidences ofde novoOAB symptoms (daytime frequency,nocturia,urinary urgency,and UUI)after TVT-O and evaluate the efficacy of local estrogen use in reducing these symptoms.The secondary outcomes were to assess any urodynamic changes and possible drug adverse events.Subjective cure of SUI was defined as the absence of any leakage with coughing,sneezing,or exerting any strenuous effort;and as regards the objective cure rate,the patient was considered cured with negative stress test during follow-up examination.
2.4.Intervention
The TVT-O was done under spinal anesthesia.The patients in Group A were instructed to use estrogen cream (Premarin,Pfizer,Cairo,Egypt),0.625 mg vaginally,once daily for 2 weeks,and then twice weekly for 6 months.We assessed patients’compliance by asking them to make follow-up visit to our clinic once the cream pack was empty to record new data.Group B patients had the TVT-O procedure only.We reviewed the patients at 3-month follow-up and again at 6-month follow-up.
2.5.Statistical analysis
The SPSS version 21 (SPSS Inc.,Armonk,NY,USA) was used for data analysis.Quantitative variables were described as mean and standard deviation (SD),and median and interquartile range,while qualitative variables were described as number and percentage.The Chi-square test was used to compare qualitative variables between groups.Fisher exact test was used when one expected cell or more are less than 5 in count.Mann-Whitney test was used instead of unpairedt-test in non-parametric data (SD>30% mean) to compare quantitative variables between groups.Wilcoxon test was used instead of pairedt-test in non-parametric variables(SD>30% mean) to compare paired quantitative variables between pre-estrogen and post-estrogen treatment.McNemar-Bowker test was used to compare paired qualitative variables between pre-and post-treatment.Thepvalue of <0.05 is statistically significant.
3.Results
All the follow-up period was planned to end by March 2021.In Group A,three patients missed follow-ups and two patients were diagnosed with vaginal moniliasis and they discontinued estrogen treatment.In Group B,five patients missed their follow-ups.Therefore,100 patients in each group continued to follow up till the end of our study(Fig.1).
The demographic data were similar for both groups with a statistically insignificant difference(Table 1).The median age of the patients was 59.5 (interquartile range:55.0-65.0)years for Group A and 58.0(interquartile range:55.0-65.0) years for Group B.In Group A,97% were multipara and 3% nullipara while in Group B,all the patients were multiparas.In both groups,patients with grades I and II prolapse (according to Pelvic Organ Prolapse Quantification classification system) were almost equal.

Table 1 The patients’ pretreatment clinical data with intraoperative and postoperative events.
There were no statistically significant intraoperative complications (p=0.237) or significant postoperative hemorrhage (p=1.000) between both groups.Only one patient needed a blood transfusion in Group A.Four cases of intraoperative vaginal bleeding were in Group A and one case was in Group B.There were no patients had to be operated on again during the 6-month period.There were no cases of tape erosion or bladder perforation.
There was a statistically significant difference in postoperative wound healing events as regards to cure,hyperemia,gapping,and wound infection 1 week after intervention between both groups (p=0.008).At 6-month follow-up,the subjective cure rate was 92% in Group A and 91% in Group B (Table 2).In Group A,6% of patients had urodynamic SUI and 2% had mixed incontinence with the predominance of SUI and in Group B,5% of patients had urodynamic SUI stress and 4% had mixed incontinence with the predominance of SUI,but the differences were not statistically significant.
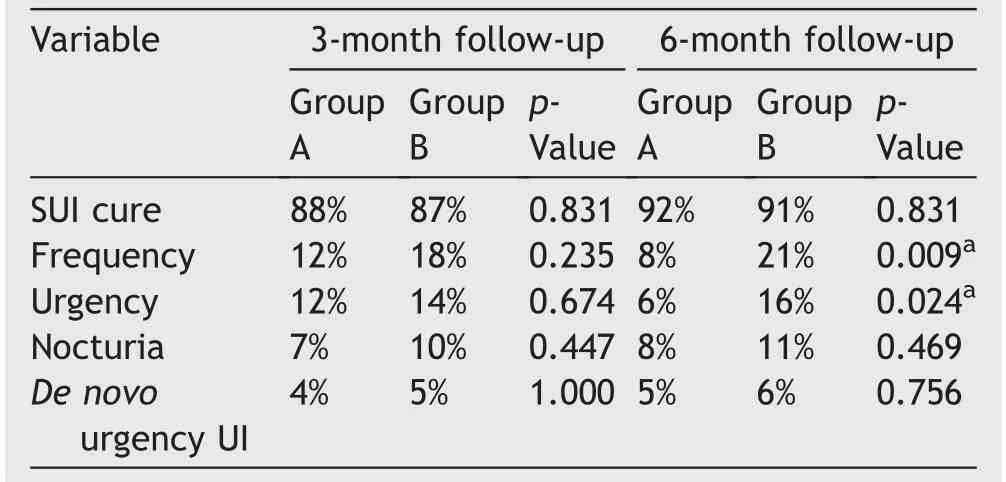
Table 2 Clinical changes at 3-month and 6-month follow-ups.
Daytime frequency,which was present in 22% in Group A,was improved to 12% at 3-month follow-up,while in Group B,the initial frequency was in 12% of the patients and increased up to 18% at 3-month follow-up;the frequencies at 3-month follow-up between Group A and Group B were not statistically significant (p=0.235) (Table 2).At 6-month follow-up,daytime frequency was reduced to 8% in Group A(mean±SD of frequency episodes:1.06±3.85),and increased to 21% in Group B (mean±SD of frequency episodes:3.67±7.12) with a highly statistically significant difference between both groups (p=0.009) (Tables 2 and 3).

Figure 1 Participants’ flow diagram.SUI,stress urinary incontinence;TVT-O,tension-free vaginal tape-obturator.Group A,TVT-O and estrogen;Group B,TVT-O only.
Nocturia which was present preoperatively in 13% of Group A (mean±SD of nocturia episodes: 0.60±1.70) was improved to 7% at 3-month follow-up,meanwhile no change in Group B at 3-month follow-up,with no statistically significant difference between both groups (p=0.447).At 6-month follow-up,nocturia was 8% in Group A (11% in Group B) with no statistically significant difference between both groups (p=0.469).There was no statistically significant difference between both groups as regards to urinary urgency at 3-month follow-up (p=0.674),while there was a high statistically significant difference at 6-month follow-up between both groups (p=0.024)(Table 2).Preoperative mean urgency episodes in Groups A and B were 0.70 (SD 1.93) and 0.60 (SD 1.82),respectively.At 6-month follow-up,mean urinary urgency episodes in Groups A and B were 0.40 (SD 1.36) and 0.93 (SD 2.32),respectively (Table 3).De novoUUI appeared in five patients in Group A and six patients in Group B with no statistically significant difference (p=1.000).
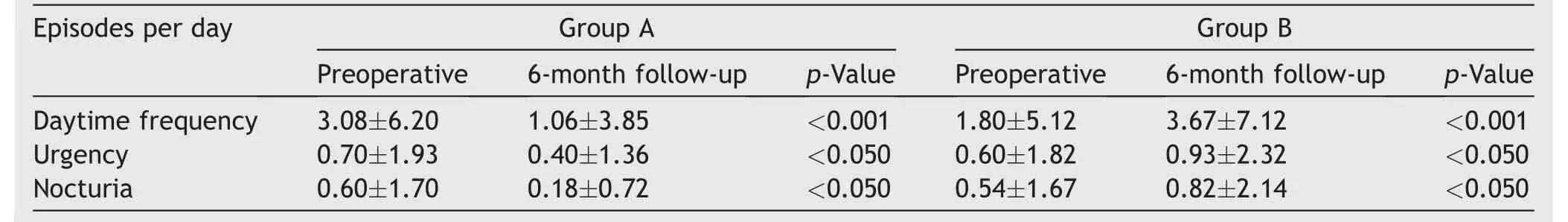
Table 3 Preoperative and 6-month follow-up clinical findings.
As regards to the OAB symptoms score,there was a statistically significant improvement in the score at 6-month follow-up (p=0.015,preoperativelyvs.at 6-month follow-up) in Group A,and in Group B there was a deterioration in OAB symptom score at 6-month follow-up which was statistically significant (p<0.001,preoperativelyvs.at 6-month follow-up) (Table 4).Also,we found that 22 patients in Group A had OAB symptoms preoperatively and after 6-month follow-up after surgery,only 13 patients had persistent OAB symptoms (59.1%),meanwhile in Group B OAB symptoms were present in 12 patients preoperatively that deteriorated to be present in a total of 30 patients (increased by 150%).

Table 4 OAB symptom score preoperatively and at 6-month follow-up.
There was no statistically significant change between both groups as regards to urodynamic findings such as maximal cystometric capacity,maximum flow rate,or detrusor pressure change at maximum flow (Table 5) or post-voiding residual urine.No local or systemic side effects were reported from local estrogen use.Seven patients,two in Group A and five in Group B who developed a urinary tract infection during the follow-up period,were treated with proper antibiotics according to urine culture and sensitivity.
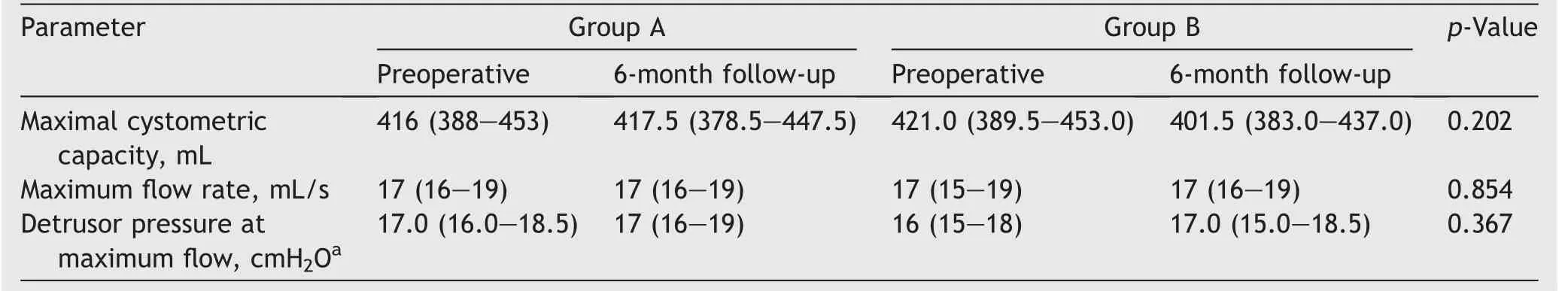
Table 5 Preoperative and 6-month follow-up urodynamic findings.
4.Discussion
TVT has been proven to be safe and highly effective and has become a standard treatment for SUI [14,15].However,Giberti et al.[16]found rate of the postoperative urinary urge of 14.8%,while Delorme[17]reported it was 6.25%,and Marcelissen and Van Kerrebroeck[10]reported that in their review the incidences ofde novourgency and UUI reported were around 15% and 30%,respectively.
Our main concern was persistent OAB symptoms after MUS and the appearance ofde novosymptoms after cure of SUI in absence of any postoperative dysfunctional voiding;few studies reported the use of topical estrogen after MUS to assess the efficacy of reducing persistent orde novosymptoms.All these data justified our postoperative use of topical vaginal estrogen for 6 months.In our study,daytime frequency and urinary urgency improved at 6-month follow-up after surgery,and they are statistically significant between both groups at 6-month follow-up after surgery(p=0.009 andp=0.024,respectively).During the immediate postoperative period,there was a statistically significant difference in postoperative wound healing events as regards to cure,gapping,hyperemia,and wound infection 1 week after intervention between both groups(p=0.008).
Estrogen affects collagen synthesis and collagen metabolism in the lower genital tract [18].The systemic collagenase activity may alter urogenital atrophic changes in women.This may cause SUI as well as urogenital prolapse[19].UUI in particular is more prevalent after menopause,and its prevalence increases with increasing years of estrogen deficiency [18].Estrogen affects detrusor function through direct action on detrusor muscarinic receptors[20].However,de novoor persistent daytime frequency or urinary urgency may be attributed to the compensatory detrusor overactivity in a trial to overcome the sling mechanical obstruction.Local irritation caused by the tape itself may also be an additional mechanism [6].All these reasons may explain the improvement in OAB symptoms in estrogen-treated group which we thought primarily was as a result of the restoration of urogenital atrophic changes that result from estrogen deficiency in postmenopausal women.Dramatic improvement of urgency and daytime frequency in our study may omit the placebo effect from estrogen use.
Cardozo et al.[21]randomized 110 postmenopausal patients to use topical vaginal estradiol.They concluded a minor improvement in sensory urgency symptoms with vaginal estradiol tablets.The recommendation of National Institute for Clinical Excellence guidelines on urinary incontinence [22]in females is to use vaginal estrogens in postmenopausal women with OAB and urogenital atrophy.Tseng et al.[23]in a randomized comparative study in 2009 reported that a combination of vaginal estrogen cream and tolterodine was a potential therapy for postmenopausal women with OAB symptoms.
Weber et al.[24]in 2015 did a systematic search in MEDLINE,EMBASE,the Cochrane Central Register of Controlled Trials,and the non-MEDLINE subset of PubMed for local estrogens and vaginal atrophy,urinary incontinence and OAB symptoms,and pelvic organ prolapse.They concluded that topical estrogen administration is effective for the treatment of vaginal atrophy and decreasing complaints of OAB symptoms and urinary incontinence.The International Urogynecology Association Research and Development Committee [25]in 2020 announced that vaginal estrogen treatment has more beneficial effects on symptoms and signs of vaginal atrophy including burning sensation,dyspareunia,and urinary incontinence symptoms.
Studies were done on women with idiopathic OAB symptoms urgency with or without UUI.Our population target was postmenopausal females with urodynamic pure SUI which differs from previous studies populations.Only two studies have the same target populations as our study.
Our findings are similar to Liapis et al.[6](Table 6);in their prospective randomized study,which included 183 female patients having the TVT-O procedure for urodynamic proved SUI,92 patients were in estrogen group,and 91 patients were in the non-estrogen group.The incidences of urinary urgency and daytime frequency were 3% and 2% in the treatment group and 12% and 10% in the control group,respectively;meanwhile in our study,the incidences of urgency and frequency were 6% and 8% in the treatment group and 16% and 21% in the control group,respectively.They concluded that vaginal estrogen treatment could be offered to postmenopausal patients after a TVT-O procedure having the symptoms of daytime frequency and urinary urgency,with no effect on urodynamic parameters.In addition to that,our study showed there was a statistically significant difference in postoperative wound healing (Table 1).In addition,our study included more details as regards clinical findings including the mean number of the daytime frequency episodes,urgency,and nocturia episodes preoperatively and at 6-month follow-up.
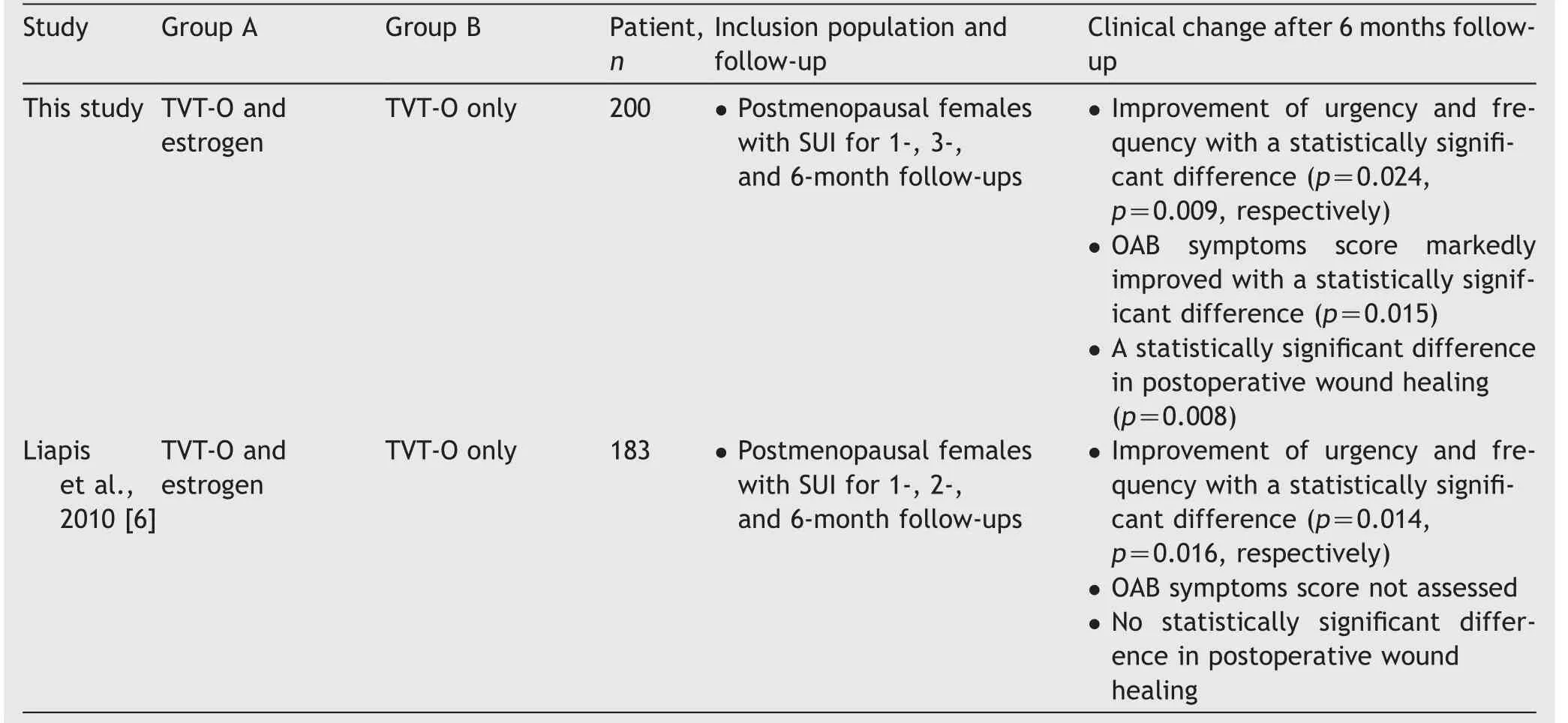
Table 6 Comparison between this study and the study by Liapis et al.[6].
Zullo et al.[26]in 2005 reported a significant reduction of urinary urgency by vaginal estriol therapy at 6-month follow-up assessment;the incidence of urgency was 4% in the estriol group and 29% in the non-estriol group.Our study has a larger sample size and showed significant improvement clinically and statistically in urinary urgency (at 6-month follow-up,the incidence of urgency was 6% in the estrogen group and 16% in the non-estrogen group) and daytime frequency was reduced to 8% in estrogen group(mean±SD of frequency episodes in Group A: 1.06±3.85)meanwhile increased to 21% in Group B (mean±SD of frequency episodes in Group B: 3.67±7.12).In our study,no local or systemic side-effects were reported from local estrogen use.
One of the strongest points in our study is that it is a prospective randomized controlled study with a large sample size compared to previous studies.Another strong point was that our target population was postmenopausal women with definite urogenital atrophic changes as a result of estrogen deficiency (median age: 59.5 [interquartile range: 55.0-65.0]years for the estrogen group and 58.0 [interquartile range: 55.0-65.0]years for the non-estrogen group).Our recommendation is the need to evaluate if there is a role for topical vaginal estrogen after MUS in the premenopausal women with persistent orde novourinary urgency and daytime frequency symptoms and if there are side effects from its use in premenopausal period.Another recommendation is the need for a long-term follow-up more than 6 months to evaluate if there are any drug side effects and what will happen if the drug is discontinued.
5.Conclusion
Local vaginal estrogen treatment given to postmenopausal patients after MUS procedures can reduce the symptoms of daytime frequency and urinary urgency.Long-term follow-up is needed.
Author contributions
Studyconcept and design: Samer Mahmoud Morsy.
Data acquisition: Dalia Farouk.
Data analysis: Hussein Aly Hussein.
Drafting of manuscript: Samer Mahmoud Morsy.
Critical revision of the manuscript: Sara Hassan,Ahmed Yehia Abdelaziz.
Conflicts of interest
The authors declare no conflict of interest.
杂志排行
Asian Journal of Urology的其它文章
- Transurethral resection of bladder tumor:A systematic review of simulator-based training courses and curricula
- Etiology and management of urethral calculi:A systematic review of contemporary series
- Oncologic outcomes with and without amniotic membranes in robotic-assisted radical prostatectomy: A propensity score matched analysis
- Single nucleotide polymorphism within chromosome 8q24 is associated with prostate cancer development in Saudi Arabia
- The risk of prostate cancer on incidental finding of an avid prostate uptake on 2-deoxy-2-[ 18F]fluoro-D-glucose positron emission tomography/computed tomography for non-prostate cancer-related pathology:A single centre retrospective study
- Prevention of thromboembolic events after radical prostatectomy in patients with hereditary thrombophilia due to a factor V Leiden mutation by multidisciplinary coagulation management
