Defining minimal invasive surgical therapy for benign prostatic obstruction surgery:Perspectives from a global knowledge,attitude,and practice survey
2024-02-25BryaKwuCuCeSteffKarKeYueDaeeCasteaMareLaerWrawsHdaZaMaaruaCruveaWeCuaYeeYreTadrJeadeRsetteErqueVetMsraAyKraeDeaEteraBasarSaJereyYueCuTeVeetGauar
Brya Kwu-Cu Ce,Steff Kar-Ke Yue ,Daee Castea ,Mare Laer Wraws ,Hda Za ,Maarua Cruvea ,We-J Cua,H-Yee T,Yre Tadr,Jea de a Rsette,Erque R,Vet Msra,Ay Krae,Dea S.Etera,Basar K.Sa,Jerey Yue-Cu Te,Veet Gauar
a Department of Surgery,United Christian Hospital,Hong Kong,China
b S.H.Ho Urology Centre,Department of Surgery,Prince of Wales Hospital,The Chinese University of Hong Kong,Hong Kong,China
c Department of Urology,University Hospital “Ospedali Riuniti” and Polytechnic University of Marche Region,Ancona,Italy
d Hospital Israelita Albert Einstein,Sao Paulo,SP,Brazil
e BP-A Beneficencia Portuguesa de Sao Paulo,Sao Paulo,SP,Brazil
f Faculdade de Medicina do ABC,Santo Andre,SP,Brazil
g Department of Urology,Asian Institute of Nephrology and Urology,Hyderabad,TG,India
h Department of Urology,National University Hospital,Singapore
i Department of Urology,Marmara University School of Medicine,Istanbul,Turkey
j Department of Urology,Medipol Mega University Hospital,Istanbul Medipol University,Istanbul,Turkey
k Department of Urology,Hospital Quiron Barcelona,Barcelona,Spain
lDepartment of Urology,Clinique Pasteur,Toulouse,France
m Department of Urology,Indiana University School of Medicine,Indianapolis,IN,USA
n Division of Urology,Department of Surgery,University Health Network,University of Toronto,Toronto,Canada
o Department of Urology,University Hospital Southampton NHS Trust,Southampton,UK
p Department of Urology,Ng Teng Fong General Hospital,NUHS,Singapore
KEYWORDS Benign prostate hyperplasia;Minimal invasive surgical therapy;Surgery;Bladder outlet obstruction
Abstract Objective: To scrutinize the definitions of minimal invasive surgical therapy(MIST)and to investigate urologists’knowledge,attitudes,and practices for benign prostatic obstruction surgeries.Methods: A 36-item survey was developed with a Delphi method.Questions on definitions of MIST and attitudes and practices of benign prostatic obstruction surgeries were included.Urologists were invited globally to complete the online survey.Consensus was achieved when more than or equal to 70% responses were “agree or strongly agree” and less than or equal to 15% responses were “disagree or strongly disagree”(consensus agree),or when more than or equal to 70% responses were “disagree or strongly disagree” and less than or equal to 15% responses were “agree or strongly agree” (consensus disagree).Results: The top three qualities for defining MIST were minimal blood loss(n=466,80.3%),fast post-operative recovery (n=431,74.3%),and short hospital stay (n=425,73.3%).The top three surgeries that were regarded as MIST were Urolift® (n=361,62.2%),Rezum® (n=351,60.5%),and endoscopic enucleation of the prostate (EEP) (n=332,57.2%).Consensus in the knowledge section was achieved for the superiority of Urolift®,Rezum®,and iTIND® over transurethral resection of the prostate with regard to blood loss,recovery,day surgery feasibility,and post-operative continence.Consensus in the attitudes section was achieved for the superiority of Urolift®,Rezum®,and iTIND® over transurethral resection of the prostate with regard to blood loss,recovery,and day surgery feasibility.Consensus on both sections was achieved for EEP as the option with the better symptoms and flow improvement,lower retreatment rate,and better suitable for prostate more than 80 mL.Conclusion: Minimal blood loss,fast post-operative recovery,and short hospital stay were the most important qualities for defining MIST.Urolift®,Rezum®,and EEP were regarded as MIST by most urologists.
1.Introduction
Lower urinary tract symptoms related to benign prostatic obstruction (BPO) are common in elderly men [1,2].BPO surgery is usually offered to men who have failed medical treatment or have experienced complications from BPO[3].Transurethral resection of the prostate (TURP) has long been regarded as the gold standard for BPO surgery since its introduction almost a century ago.TURP was first introduced as a minimal invasive surgical therapy (MIST),as compared to simple prostatectomy being the only alternative option in the early 20th century.TURP has a perceived short learning curve and a reasonable safety profile;such merits have perpetuated its establishment as an important BPO surgical option even after a century [3,4].However,TURP is not without limitations and comorbidities.This has expedited the development of novel BPO surgeries throughout the recent two decades,which has acclaimed various advantages compared to TURP [5].These advantages include greater symptoms and flow improvement,better bleeding profile,complete adenoma removal,faster post-operative recovery,and shorter post-operative catheterization and hospital length of stay [5,6].New MIST and surgical techniques for BPO treatment may even preserve antegrade ejaculation and sexual function [7].
However,there has been no study undertaken benchmarking a procedure to be qualified as MIST.The potential advantages of faster recovery and better clinical outcomes by these new interventions have given rise to the need to define what specific outcomes a MIST procedure must fulfill.Despite the current wide range of BPO surgery options,their accessibilities to urologists and adoption rates vary globally.In order to further our understanding of urologists’ perspective on this and to reach a consensus on what defines MIST from a global perspective,we have conducted a worldwide knowledge,attitude,and practice survey amongst urologists.
2.Materials and methods
This is a cross-sectional study via a web-based self-administered survey.The study was performed in accordance with the Declaration of Helsinki.The objective of the global survey was to explore the definition of MIST,and investigate the knowledge,attitudes,and practices on BPO surgeries of urologists.The survey was developed by the steering committee using a Delphi method.The structured survey consisted of 36 questions,including questions on demographics,definitions of MIST,and the knowledge,attitudes,and practices in BPO surgeries.Multiple answers were allowed for the two questions on definition of MIST.For questions on knowledge and attitude,a 5-point Likert scale ranging from “strongly disagree” to “strongly agree”,and “not familiar” were included as options of answers.All questions were structured to compare against the reference standard TURP in the knowledge and attitude sections.The surgical options of interest included convective water vapor energy ablation (Rezum®,Boston Scientific,Natick,MA,USA),endoscopic enucleation of the prostate(EEP),image-guided robotic waterjet ablation (Aquablation®,PROCEPT BioRobotics,Redwood Shores,CA,USA),prostatic arterial embolization(PAE),prostatic urethral lift(Urolift®,Teleflex Interventional Urology,PA,USA),robotic or laparoscopic simple prostatectomy (RASP),temporary implantable nitinol device (iTIND®,Medi-Tate,Israel),and photoselective vaporization of prostate.The questionnaire is shown in the appendix (Appendix file 1).The survey was uploaded and conducted via an online platform,Survey Monkey (SVMK Inc.,San Mateo,CA,USA).
The urology community was invited globally to participate via social media (#UroSoMe platforms in Twitter) and the fellow mailing list of international urological associations(Appendix file 2).The link to the online survey(www.surveymonkey.com/MISTKAPSurvey) was provided and respondent could complete the survey online.Internet protocol restriction was implemented,where one internet protocol address could complete the survey once only.All data were only accessible to investigators.
In order to facilitate the interpretation on the knowledge,attitude,and practice questions with Likert scale,the investigators decided on the definition of a consensus concerning the respective responses.Consensus was achieved when ≥70% responses were “agree or strongly agree” and≤15% responses were “disagree or strongly disagree”(consensus agree),or when ≥70% responses were “disagree or strongly disagree” and ≤15% responses were “agree or strongly agree”(consensus disagree)[8].In questions without Likert scale,the numbers and percentages were summarized and tabulated.Descriptive statistical analyses were performed for the survey results.
3.Results
A total of 755 participants responded to the survey.The demographics and their experiences of BPO surgeries are shown in Table 1.Majority of the participants were male,aged 30-39 years old.Majority of them are urology consultants.Most participants come from Europe,followed by Asia and South America.The complete survey responses are shown in the appendix (Appendix file 3).Aquablation®was the most common treatment option which was reported as “not familiar” in all questions.
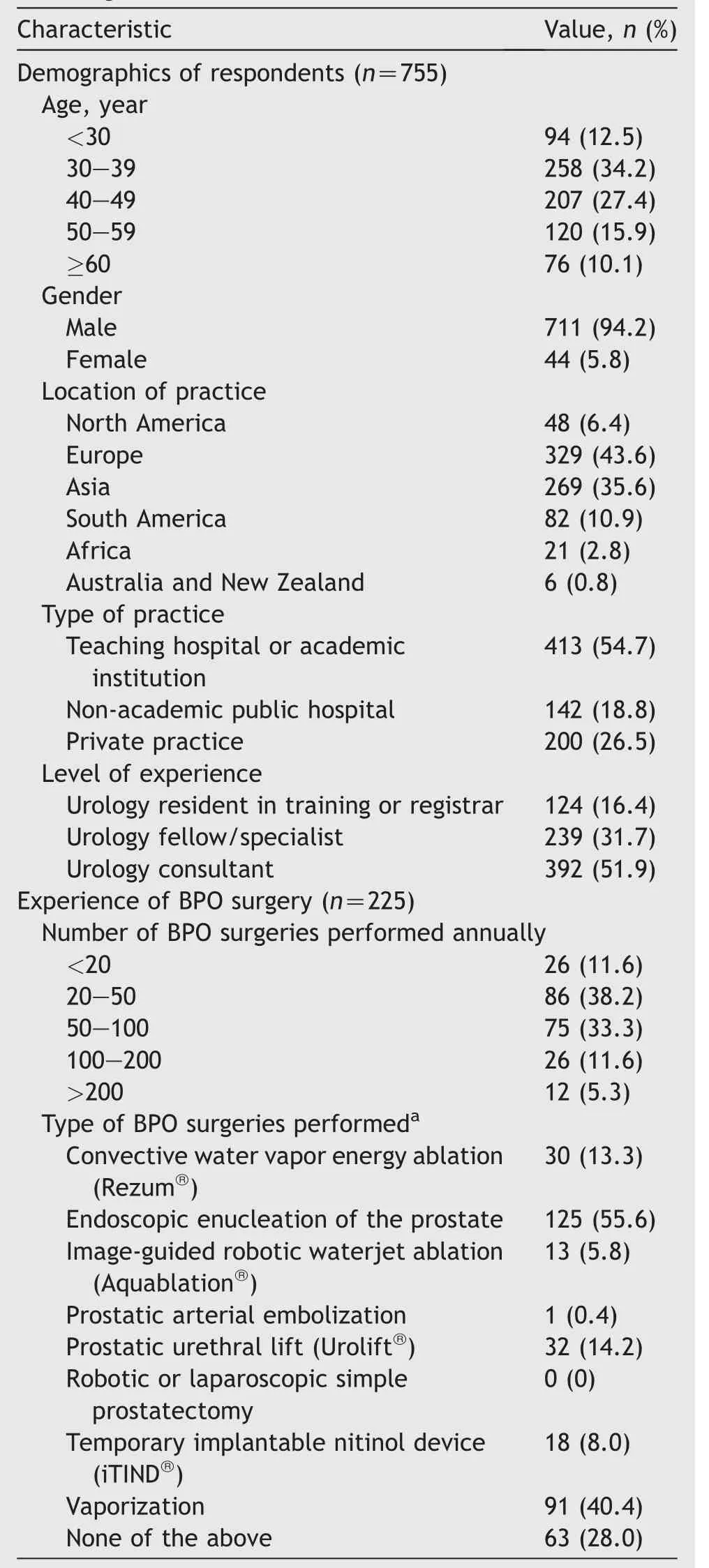
Table 1 Demographics of respondents and experiences of BPO surgeries.
3.1.Definition of MIST
Totally 580(76.8%)participants responded to the questions on definition of MIST.The top three important qualities in defining MIST were minimal blood loss(n=466,80.3%),fast post-operative recovery (n=431,74.3%),and short length of hospital stay (n=425,73.3%).The top three surgical options that were regarded as MIST were Urolift®(n=361,62.2%),Rezum®(n=351,60.5%),and EEP (n=332,57.2%).
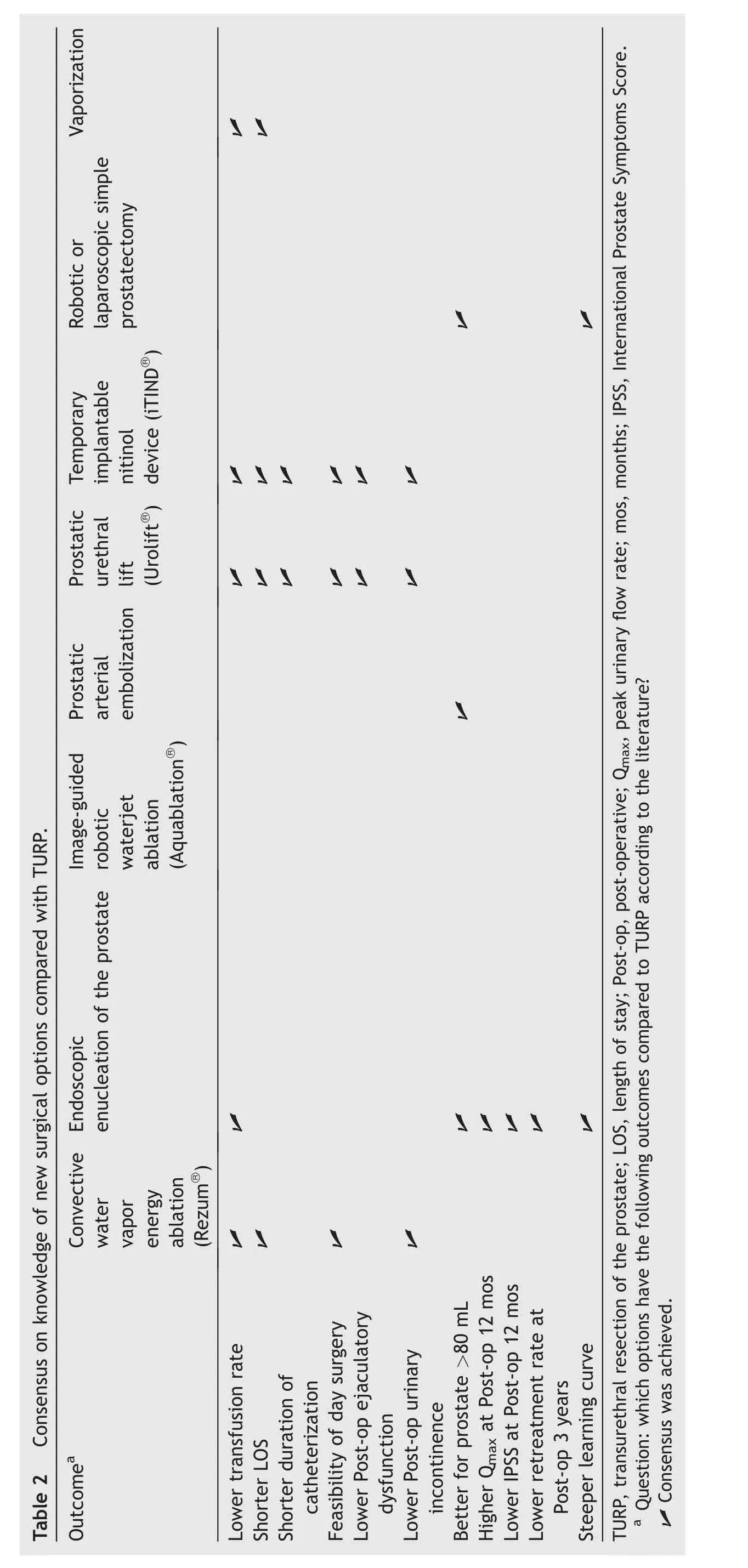
3.2.Knowledge in BPO surgeries
Three hundred and twelve (41.3%) participants responded to the questions in knowledge section (Table 2).Consensus agreement was achieved for the superiority of Urolift®,Rezum®,and iTIND®over TURP with regard to lower blood loss,faster recovery,feasibility of day surgery,and lower post-operative incontinence.Urolift®and iTIND®had additional benefits of shorter duration of catheterization and lower post-operative ejaculatory dysfunction.EEP was chosen as the option with better symptoms and flow improvement,lower retreatment rate,and better suited for prostate more than 80 mL.EEP was also the only option chosen to have a steeper learning curve than TURP.Except for Aquablation®,PAE,and RASP,all other options were reported to have a lower transfusion rate compared to TURP.
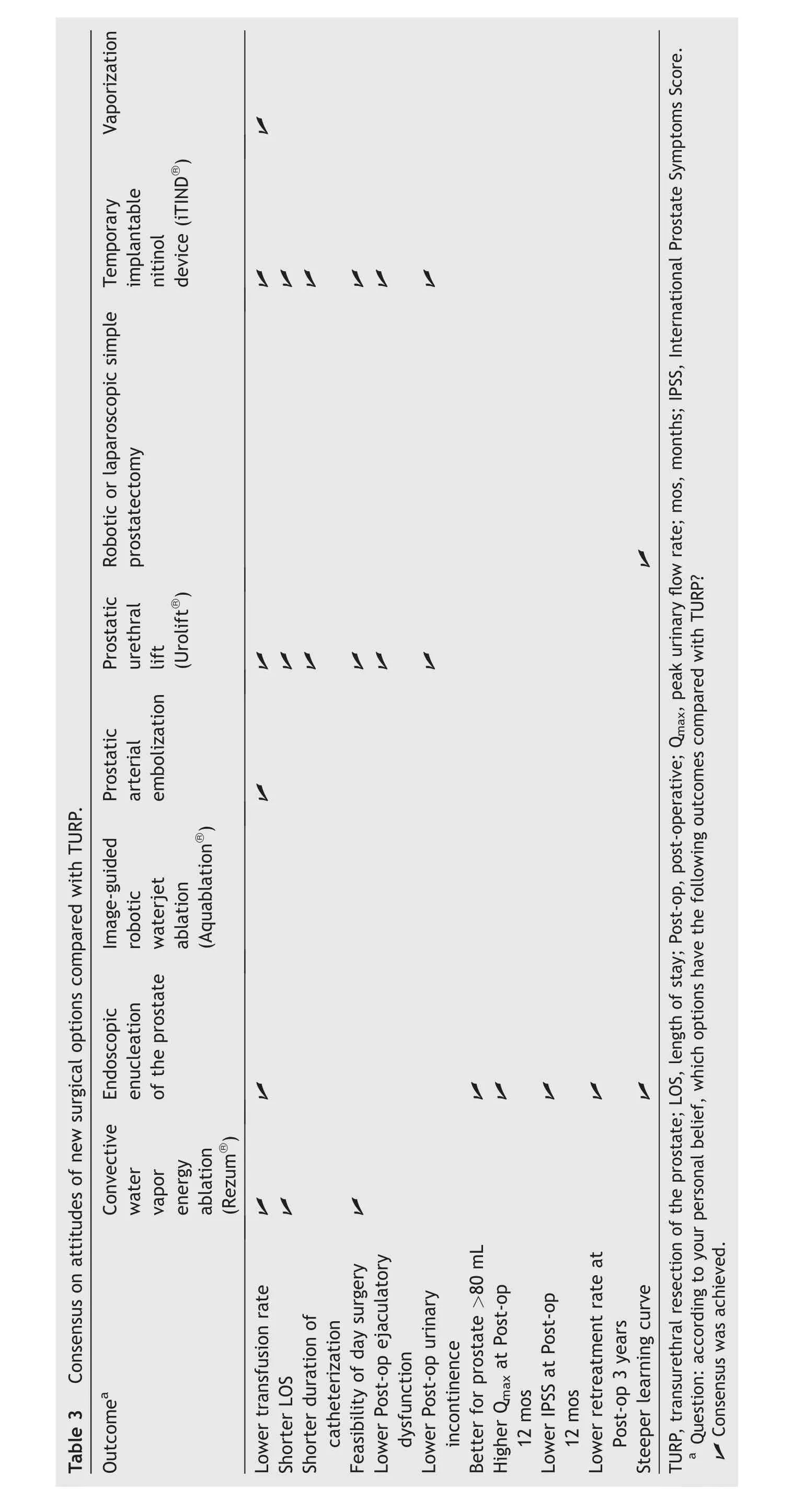
3.3.Attitudes in BPO surgeries
Two hundred and twenty-eight (30.2%) participants responded to the questions in attitude section (Table 3).Consensus agreement was achieved for the superiority of Urolift®,Rezum®,and iTIND®over TURP for lower blood loss,faster recovery,and feasibility of day surgery.Urolift®and iTIND®had additional benefits of shorter duration of catheterization,lower post-operative ejaculatory dysfunction,and lower post-operative urinary incontinence.EEP was also regarded as the option with better symptoms and flow improvement,low retreatment rate,and better for prostate more than 80 mL.Except for Aquablation®and RASP,all other options were believed to have a lower transfusion rate compared with TURP.Both EEP and RASP were believed to have a steeper learning curve than TURP.
3.4.Practices in BPO surgeries
Two hundred and twenty-five (29.8%) participants responded to the questions in practice section (Table 4).Majority of them performed 20-50 BPO surgeries per year.EEP and vaporization were the most commonly performed BPO surgeries (excluding TURP).No participants had reported performing RASP,and few had performed experience in Aquablation®(n=13),iTIND®(n=18),and PAE (n=1)(Table 1).Equipment availability was a major issue in adopting most BPO surgical techniques.Learning curve was a major issue in mastering both EEP and RASP,as well as PAE.Cost was a major concern in Rezum®and Aquablation®.Spinal anesthesia was most commonly chosen for BPO surgeries,whilst local anesthesia was believed to be feasible for Urolift®and iTIND®.Ambulatory surgery was believed to be feasible for Rezum®,Urolift®,and iTIND®(Table 5).
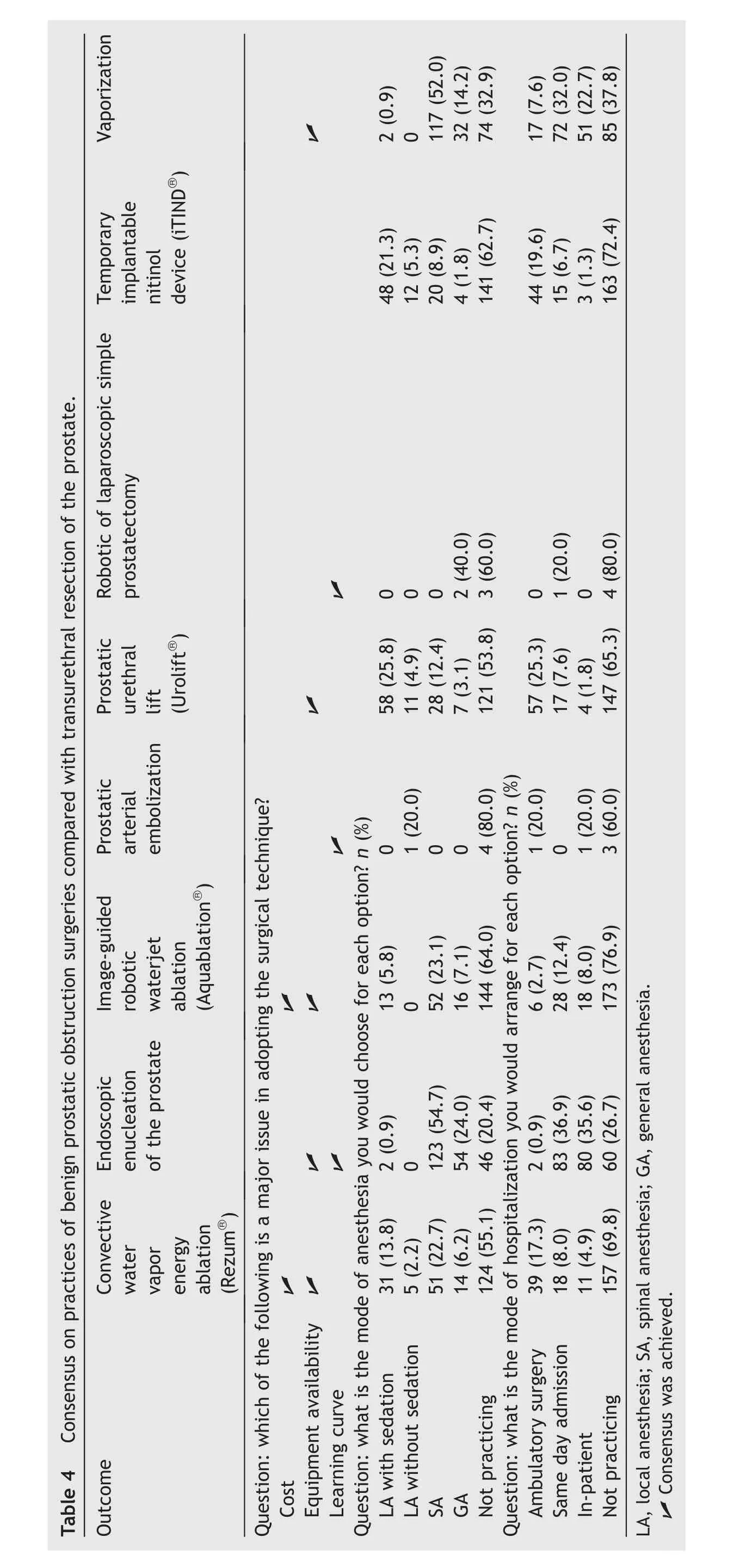
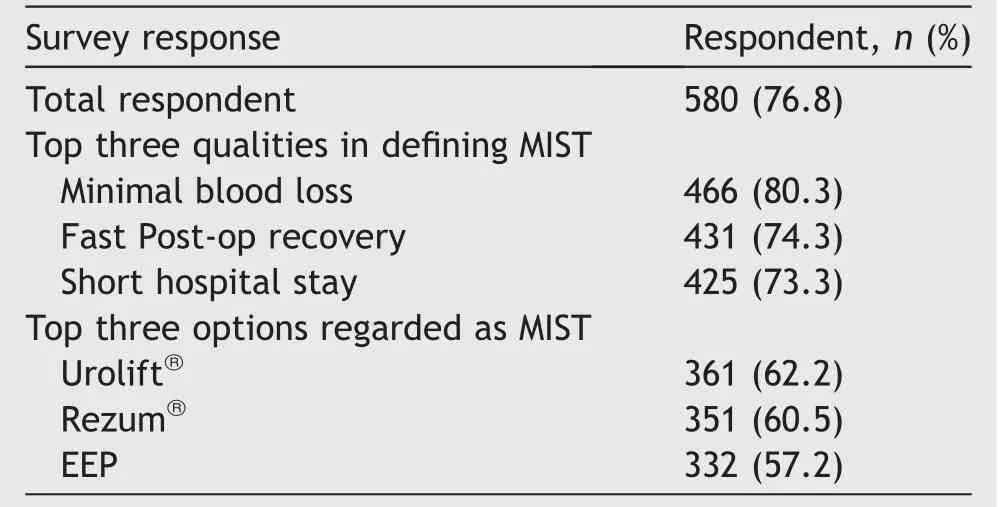
Table 5 Summary of responses on MIST definitions.
4.Discussion
As the reference standard of BPO surgeries,TURP has continuously been challenged by new surgical approaches.The size limitation,peri-operative morbidities,and sexual complications of TURP have triggered the development of novel interventions as technology advances.These new treatments advocate faster recovery,lower complications,better uroflow,and symptom improvement in comparison to TURP [5].To the best of our knowledge,this is the first study investigating the knowledge,attitudes,and practices of urologists towards various types of BPO surgical treatments on a global scale.It provides valuable insights in the understanding,beliefs,and practices of worldwide urologists on the wide spectrum of surgeries.
The term “MIST” in BPO surgeries was used initially to describe the minimally invasive options that emerged near the end of 20th century [9,10].These included transurethral needle ablation of prostate (TUNA) and transurethral microwave thermotherapy,which had once demonstrated a good short-term efficacy in symptoms and flow improvement.They have also been advocated previously as feasible for day surgery.However,they were both removed from European Association of Urology guidelines since 2019.In American Urological Association (AUA) guidelines,TUNA was not recommended while transurethral microwave thermotherapy could be offered to men with lower urinary tract symptoms at a Grade C evidence level[11].For TUNA,AUA guidelines stated that the prostatic volume was reduced less than expected and the tissue was replaced with scar.There was also no consensus on the mechanism of action.Since 2003 little new evidence on effectiveness and safety had been published on TUNA,thus it was no longer recommended[11].It was clear that the definition and the components of MIST have changed over time,and a global consensus should be reinstated in the contemporary era with the newest array of treatments.
AUA guidelines referred MIST to Rezum®,Urolift®,and PAE [11].It disregarded Aquablation®as MIST because it requires general anesthesia.The guidelines stated that a successful MIST should include tolerability,rapid,and durable relief of symptoms,short recovery time with rapid return to life activities,minimal adverse events,and affordability.From urologist’s perspective,MIST should also have the capacity for performance in an ambulatory setting under reduced anesthesia,fast learning curve,generalizability from randomized controlled trials,and ease of performance [11].However,it did not provide scientific basis and evidence for these classifications.On the contrary,European Association of Urology guidelines did not include the term MIST.
One important objective of the survey was to explore the quality of a surgery needed to be defined as MIST from a global consensus.In our results,the three most important components for MIST were minimal blood loss,fast post-operative recovery,and short length of hospital stay.These are all important parameters related to the early recovery and return to normal activities after surgery.These preferred qualities of MIST were reflected in the chosen MIST options,Rezum®,and Urolift®-all were proven to possess excellent peri-operative morbidity profile and concurred with the opinions from AUA guidelines[11,12].EEP was voted by 57.2% of participants as the third chosen MIST.Doubtless to say,the nature of EEP was remarkably different from the other two chosen options,which require general or spinal anesthesia and very often require overnight hospitalization.However,the choice of EEP as MIST could still be justified as it was more established,and truly superior to TURP in terms of blood loss,shorter catheterization time,and shorter hospital stay,which were all important components for MIST [6].In addition,day surgery for EEP was actually proven feasible in high volume center [13].To address the differences between those office procedures and more invasive transurethral surgeries,Elterman et al.[14]have proposed the term “true minimally invasive therapy”.On the other hand,while iTIND®was chosen as possessing numerous advantages in terms of peri-operative morbidities,it was contradictorily not regarded as MIST by the participants.The lack of randomized trials compared with the reference standard TURP might have influenced the confidence of urologists for this option [15].
In general,the participants demonstrated good knowledge in accordance with the literature.The current evidence on EEP and Urolift®was mostly reflected in the consensus obtained [6,16].One important result was a universal consensus on the steep learning curve of EEP and RASP as compared to TURP in both knowledge and attitude sections[17].It was also reiterated in the practice section as a major issue.A recent systematic review showed 30-40 cases were needed to overcome the learning curve for holmium laser enucleation of prostate [18].A good mentorship and training programme was needed in promulgation of the technique [19].Overall,the results of knowledge section were remarkably similar to attitude section,which represented the wide acceptance of literature and transformation into personal beliefs of the surgical options concerned.However,results from scientific evidence may not always be translated into the results seen in daily clinical practices.A recent systematic review showed the association of conflicts of interest and industrial sponsorship with favorable surgery outcomes[20].On the other hand,surgeon experience and preferences,training,and patient selections all need to be considered in the final performance of surgery and outcomes.These might explain some of the differences between the knowledge and attitude section.For example,participants achieved a consensus on the shorter length of stay for vaporization in knowledge section,which concurred with the literature [6].However,no consensus was reached in attitude section,which might reflect their real-life experiences.Similarly for RASP,consensus was only reached in knowledge but not in the attitude section in terms of “better for prostate >80 mL”.This could likely be explained by the absence of experience in RASP by the participants.
Despite a versatile and wide range of new treatment modalities that offer a chance for personalized and tailored management of BPO,the adoption and acceptance of different treatments vary greatly.Our survey conveyed that 30% of the participants had no clinical experience in any of the surgical options on the study list,and most participants reported that they were unfamiliar with Aquablation®.This indeed reflects the reality in surgical technique dissemination and adoption globally.Various factors could be responsible for this.One important factor was equipment availability,and this was vetted as a major issue even in our survey.Other factors might include perceived clinical effectiveness,cost,learning and adoption,patient demand,manufacturer promotion,and surgeon preferences[21].In the long run,this could increase the gap between scientific evidence and clinical practices,which was indeed reflected from our study results.Despite an overwhelming agreement on the superiority of Urolift®and iTIND®in perioperative morbidities and recovery,only 14% and 8% of the participants respectively had experience in performing these procedures,corroborating the aforementioned statements.
This study presented several limitations.Owing to the great variety of available BPO surgical treatments and the numerous peri-operative parameters measured,the length of this structured survey was long.These could have hindered the responses and completion rate to the survey.Less than 30% participants completed the whole survey,rendering the results less representative than expected.Also,responses from Australia and New Zealand,North America,and Africa were limited.These undermined the representation and generalizability of the survey results.Since most of the new techniques were launched and widely practiced in America and Australia,this could skew the result on these new techniques.Since the academics were more interconnected through social network and urological associations,they were more readily engaged in this global survey.As a result,more than half of the participants come from academic institutions.This could render the urologists working in public hospital or private sectors underrepresented.Most participants had limited experience in procedures such as Aquablation®(n=13),iTIND®(n=18),RASP (n=0),and PAE (n=1).This should not affect the credibility of the result in knowledge,as one could get a solid understanding of a procedure from literature.However,it could affect the attitude section,which might be influenced by operating experience.This might create a less balanced view on the overall judgment of surgical options and skew the answers to those questions.Moreover,questions on the rate of bladder neck obstruction were not included in the survey.A recent systematic review showed a pooled incidence of 1.3% for bladder neck stenosis after TURP,0.7% after enucleation,and 1.2% after ablation.There were no statistical differences between the different treatment modalities [22].Lastly,there could be some misinterpretation of the questions by the respondents.In the questions on mode of anesthesia and mode of hospitalization,the original idea was to record their own practices of hands-on experience.Although only 30 participants had reported experience in Rezum®,101 participants had reported on the choices of anesthesia and 68 participants had reported on the mode of hospitalizations.Therefore,it was likely some respondents had answered these questions based on their knowledge from literature,own beliefs,instead of from their clinical practices.Moreover,certain options in the questions have very few participants answered.For instance,only five participants have answered to those questions on PAE and RASP.These unavoidably undermined the significance of the results on these two techniques.
5.Conclusion
Based on our survey,an ideal MIST procedure could be defined as any BPO surgery which has minimal blood loss,fast post-operative recovery,and short length of hospital stay.Urolift®,Rezum®,and EEP were chosen by most participants to fulfil the criteria of MIST.However,the experience of respondents in new BPO surgeries was limited and there were difficulties with equipment availability.These may undermine the adoption of novel surgeries and deprive our patients of a better TURP alternative.
Author contribution
Study concept and design: Bryan Kwun-Chung Cheng,Steffi Kar-Kei Yuen,Daniele Castellani,Marcelo Langer Wroclawski,Jeremy Yuen-Chun Teoh,Vineet Gauhar.
Data acquisition: Bryan Kwun-Chung Cheng,Jeremy Yuen-Chun Teoh.
Data analysis: Bryan Kwun-Chung Cheng,Steffi Kar-Kei Yuen,Daniele Castellani,Marcelo Langer Wroclawski,Jeremy Yuen-Chun Teoh,Vineet Gauhar,Jean de la Rosette.Drafting of manuscript: Bryan Kwun-Chung Cheng,Steffi Kar-Kei Yuen.
Critical revision of the manuscript: Hongda Zhao,Mallikarjuna Chiruvella,Wei-Jin Chua,Ho-Yee Tiong,Yiloren Tanidir,Jean de la Rosette,Enrique Rijo,Vincent Misrai,Amy Krambeck,Dean S.Elterman,Bhaskar K.Somani.
Conflicts of interest
Dr.Dean S.Elterman is the investigator and advisor for Boston Scientific,Medeon,Meditate,Medtronic,Procept,Urotronic,and Zenflow.The other authors declare no conflict of interest.
Appendix A.Supplementary data
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ajur.2022.02.011.
杂志排行
Asian Journal of Urology的其它文章
- Transurethral resection of bladder tumor:A systematic review of simulator-based training courses and curricula
- Etiology and management of urethral calculi:A systematic review of contemporary series
- Oncologic outcomes with and without amniotic membranes in robotic-assisted radical prostatectomy: A propensity score matched analysis
- Single nucleotide polymorphism within chromosome 8q24 is associated with prostate cancer development in Saudi Arabia
- The risk of prostate cancer on incidental finding of an avid prostate uptake on 2-deoxy-2-[ 18F]fluoro-D-glucose positron emission tomography/computed tomography for non-prostate cancer-related pathology:A single centre retrospective study
- Prevention of thromboembolic events after radical prostatectomy in patients with hereditary thrombophilia due to a factor V Leiden mutation by multidisciplinary coagulation management
