Transurethral prostate surgery in prostate cancer patients: A population-based comparative analysis of complication and mortality rates
2024-02-25MiheleMrhioniGiuliPrimieriAlessndroVeiMrtDiNiolUmertoCronrFioCroerossUgoFlgrioAmrRizzoliRirdoAutorinoLuigiShips
Mihele Mrhioni,Giuli Primieri ,Alessndro Vei ,Mrt Di Niol ,Umerto Cronr ,Fio Croeross ,Ugo Flgrio,Amr Rizzoli,Rirdo Autorino,Luigi Ships
a Laboratory of Biostatistics,Department of Medical,Oral and Biotechnological Sciences,“G.d’Annunzio” University of Chieti,Chieti,Italy
b Urology Unit,Department of Medical,Oral and Biotechnological Sciences,“G.d’Annunzio” University of Chieti,Chieti,Italy
c Division of Urology,VCU Health,Richmond,VA,USA
KEYWORDS Prostate cancer;Transurethral surgery of the prostate;Prostate surgery;Population-based analysis;Benign prostatic hyperplasia;Laser surgery
Abstract Objective: Prostate cancer (PCa) patients might experience lower urinary tract symptoms as those diagnosed with benign prostatic hyperplasia (BPH).Some of them might be treated for their lower urinary tract symptoms instead of PCa.We aimed to test the effect of PCa versus BPH on surgical outcomes after transurethral prostate surgery,namely complication and mortality rates.Methods: Within the American College of Surgeons National Surgical Quality Improvement Program database (2011-2016),we identified patients who underwent transurethral resection of the prostate,photoselective vaporization,or laser enucleation.Patients were stratified according to postoperative diagnosis(PCa vs.BPH).Univariable and multivariable logistic regression models evaluated the predictors of perioperative morbidity and mortality.A formal test of interaction between diagnosis and surgical technique used was performed.Results: Overall,34 542 patients were included.Of all,2008 (5.8%) had a diagnosis of PCa.The multivariable logistic regression model failed to show statistically significant higher rates of postoperative complications in PCa patients (odds ratio: 0.9,95% confidence interval:0.7-1.1; p=0.252).Moreover,similar rates of perioperative mortality (p=0.255),major acute cardiovascular events (p=0.581),transfusions (p=0.933),and length of stay of more than or equal to 30 days(p=0.174)were found.Additionally,all tests failed to show an interaction between post-operative diagnosis and surgical technique used.Conclusion: Patients diagnosed with PCa do not experience higher perioperative morbidity or mortality after transurethral prostate surgery when compared to their BPH counterparts.Moreover,the diagnosis seems to not influence surgical technique outcomes.
1.Introduction
Transurethral resection or enucleation,as well as laser prostate surgery,represents elective treatments among unresponsive patients to medical therapy with lower urinary tract symptoms associated with bladder outlet obstruction[1,2].As a consequence of recommendation against prostate-specific antigen screening,the incidence rate of incidental and advanced prostate cancer(PCa)has increased[3-5].Importantly,those with very low-or high-risk disease might not benefit from radical prostatectomy[6-9],but still be affected by lower urinary tract symptoms[10].
To date,most literature has focused on the outcomes of transurethral prostate surgery for bladder outlet obstruction due to benign conditions[11].However,cancer patients are at higher risk of non-surgical complications,including cardiovascular ones,even after non-cancer-related surgical procedures,and thromboprophylaxis is highly recommended for those undergoing surgery [12,13].Current guidelines recommend specific caution in patients diagnosed with PCa undergoing major surgery [14],but no specific recommendations are available for transurethral prostate surgery in patients with PCa.In literature,there is a lack of studies extensively examining the risk of complications in PCa patients undergoing bladder outlet obstruction surgery.
We aimed to test the effect of PCa on surgical and medical complications after transurethral surgery.We hypothesized that PCa patients might experience higher complication rates compared to their benign prostatic hyperplasia (BPH) counterparts,due to inherent differences associated with PCa.To test this hypothesis,we assessed the outcomes of prostate surgery performed in patients with a diagnosis of PCa compared to those with BPH,by analyzing a large surgical quality national dataset.
2.Patients and methods
2.1.Data source and study population
Data extraction was performed through Current Procedural Terminology (CPT) codes for principal transurethral prostate procedures.Patients who underwent transurethral resection of the prostate(TURP)(CPT code:52601,52630),photo-selective vaporization of the prostate (PVP) (CPT code: 52648),and prostate enucleation (CPT code: 52649)between 2011 and 2016 were abstracted from the American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP) registry.Authors had the permission to use the ACS-NSQIP registry.
After exclusion of patients with missing information about principal anesthesia,age,and American Society of Anesthesiologists(ASA)score,only those who underwent elective surgery were included.Patients with a diagnosis of disseminated cancer were also excluded.The resulting cohort was stratified according to the International Classification of Diseases(ICD)-9 and ICD-10 in two groups namely BPH(ICD-9 codes: 600.xx and ICD-10 codes: N40.xx) and PCa (ICD-9 codes:185 and ICD-10 codes:C61)[11].Within the ACS-NSQIP the ICD codes capture information regarding the indication for the principal operative procedure defined as the diagnosis code which corresponds to the patient’s condition.
2.2.Covariates of interest
Baseline characteristics considered were: age at the time of surgery (≤75 years and >75 years),year of surgery(2011-2013 and 2014-2016),race (Caucasian,African-American,and other),body mass index (underweight,normal,overweight,obese,and unknown),functional status (independent,partially dependent,totally dependent,and unknown),and current smoker status.
Comorbidities of interest were diabetes (no diabetes,insulin-dependent,and non-insulin-dependent),hypertension,respiratory disorders,congestive heart failure,chronic steroid use,bodyweight loss of more than 10%,bleeding disorders,preoperative transfusions,preoperative systemic inflammatory response syndrome or sepsis,and renal disorders.
Perioperative covariates of interest were ASA score (≤2 and >2),anesthesia type (general,locoregional,and others),inpatient status,and operation time(≤90 min and>90 min).
2.3.Outcomes and complication definition
Postoperative complication rates represented our main outcome of interest.Secondary outcomes of interest were perioperative mortality,transfusion rates,prolonged hospital stay (>30 days),and major cardiovascular events,which were defined as a composite of cerebrovascular events,cardiac arrest,myocardial infarction,deep venous thrombosis,or pulmonary embolism as defined within the ACS-NSQIP database.
Moreover,we described the main complications that occurred after surgery [15],namely postoperative pneumonia,intubation,acute renal failure,urinary tract infection,intra-and post-operative transfusions,septic shock,and sepsis.All complications were recorded up to postoperative Day 30.
Hospital readmission and reoperation within the first 30 postoperative days were also recorded.Hospital admissions were divided into unplanned ones and those related to the principal procedure.
2.4.Statistical analysis
Descriptive statics relied on mean and standard deviation for continuous variables and frequency and percentage for categorical variables.After patients’ stratification,according to diagnosis (PCavs.BPH),differences in means were ascertained by Student’st-test,while differences in frequencies were determined with Pearson’s χ2test.
Multivariable logistic regression models tested differences in primary and secondary outcomes rates.Covariates selection for multivariable logistic regression model was performed with a stepwise selection of covariates in both directions (forward and backward).All the possible models were forced to include the diagnosis as a covariate.Possible covariates within the model were those that preoperatively showed a statistically significant difference between the two groups,namely surgery type,age at surgery,race,current smoker status,hypertension,chronic steroid use,preoperative transfusions,ASA score,inpatient status,and operative time.In the final multivariable logistic regression model,only variables that ensure a model performance improvement,as indicated by the Akaike Information Criterion,were included [16].
All tests were two-sided,and a level of statistical significance was set atp-value of less than 0.05.Analyses were performed using the R software environment for statistical computing and graphics (version 4.0.0;http://www.rproject.org/).
3.Results
Overall,34 542 patients were included in the analysis.Of these,2008 (5.8%) had a diagnosis of PCa.Most of the patients underwent surgery between 2014 and 2016 (65.9%),and the most performed procedure was TURP (63.6%).Moreover,patients were more frequently aged less than or equal to 75 years (66.6%),Caucasian (69.4%),and overweight (41.8%).Included patients were generally healthy and classified as independent (96.7%);the most frequent comorbidity was hypertension (60.2%).
Compared to BPH patients,PCa patients were more frequently older than 75 years (44.9%vs.32.7%,p<0.001),African-American race(9.2%vs.5.3%,p<0.001),and with a smoking history (12.0%vs.10.3%,p=0.014).Furthermore,PCa patients had more frequently hypertension (62.4%vs.60.0%,p=0.036) and needed preoperative transfusions(0.3%vs.0.1%,p=0.002).No statistically significant differences in most of the examined comorbidities were found between PCa and BPH patients.However,PCa patients were more frequently classified as ASA score of more than 2(58.6%vs.50.1%,p<0.001) and underwent inpatient recovery (40.1%vs.31.8%,p<0.001).TURP was more frequently performed in PCa than BPH patients (78.4%vs.62.7%,p<0.001).Operative time over 90 min was also more common in PCa than BPH patients (17.5%vs.14.7%,p<0.001) (Table 1).
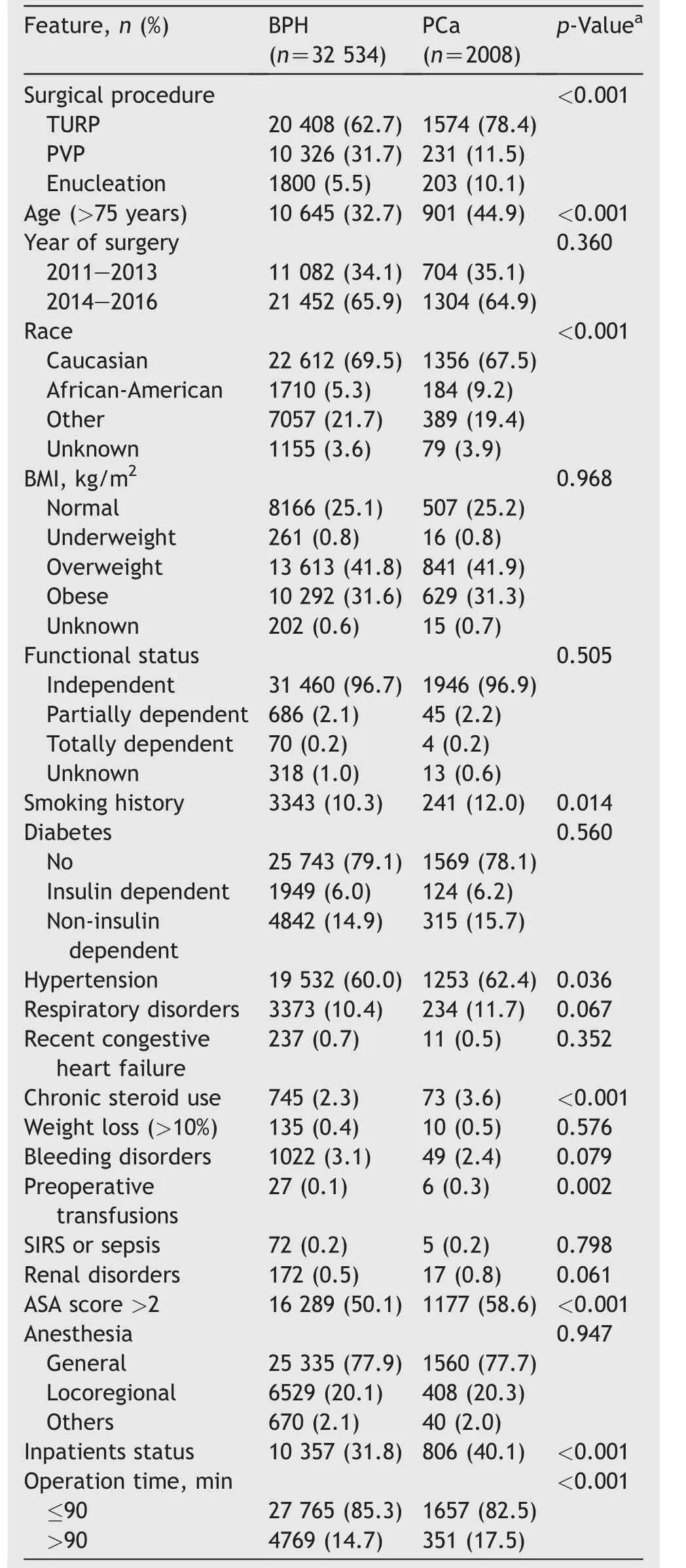
Table 1 Descriptive pre-and intra-operative characteristics of patients undergoing transurethral surgery of the prostate stratified according to diagnosis (BPH vs. PCa).
PCa patients required longer hospitalization (1.4vs.1.1 days in mean,p<0.001) and had more frequently intra-and post-operative transfusions (1.3%vs.0.8%,p=0.027).However,no statistically significant differences were found in terms of other complications (Table 2).Readmission rates were similar between the two groups.About 3.5% of patients required at least one readmission related to the procedure.The cause of readmission related to the procedure was available in 821(67.8%)cases.The most frequent reason for readmission related to the procedure was hematuria or bleeding,in 416 (50.7%) cases.Readmission-related diagnoses,coded according to the ICD-9 and ICD-10 classification,are reported in Supplementary material 1.Reoperation rates were also similar between the two groups.Of 598 patients readmitted for unplanned surgery,343 (57.4%) had a related diagnosis.The most frequent reason for reoperation was hematuria,in 193 (56.3%) cases.Related diagnoses,coded according to the ICD-9 and ICD-10 classifications are reported in Supplementary material 2.
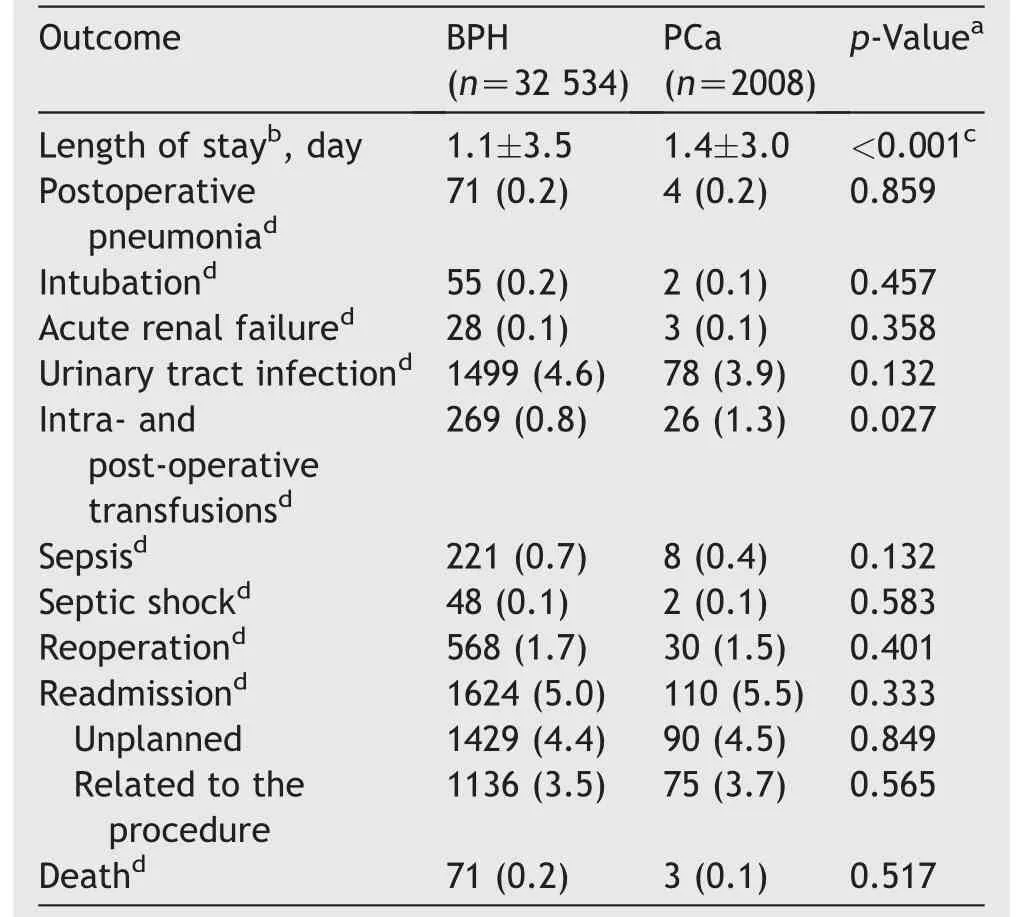
Table 2 Descriptive post-operative outcomes and complications in patients who underwent transurethral surgery of the prostate stratified according to diagnosis (BPH vs. PCa).
After multivariable adjustment,no statistically significant differences were found in terms of postoperative complication rates between PCa and BPH patients (odds ratio: 0.9,95% CI: 0.7-1.1;p=0.252).Similarly,comparable rates of perioperative mortality (p=0.255),major acute cardiovascular events (p=0.581),transfusions(p=0.933),and length of stay of more than or equal to 30 days (p=0.174) were shown in multivariable logistic regression models (Table 3).
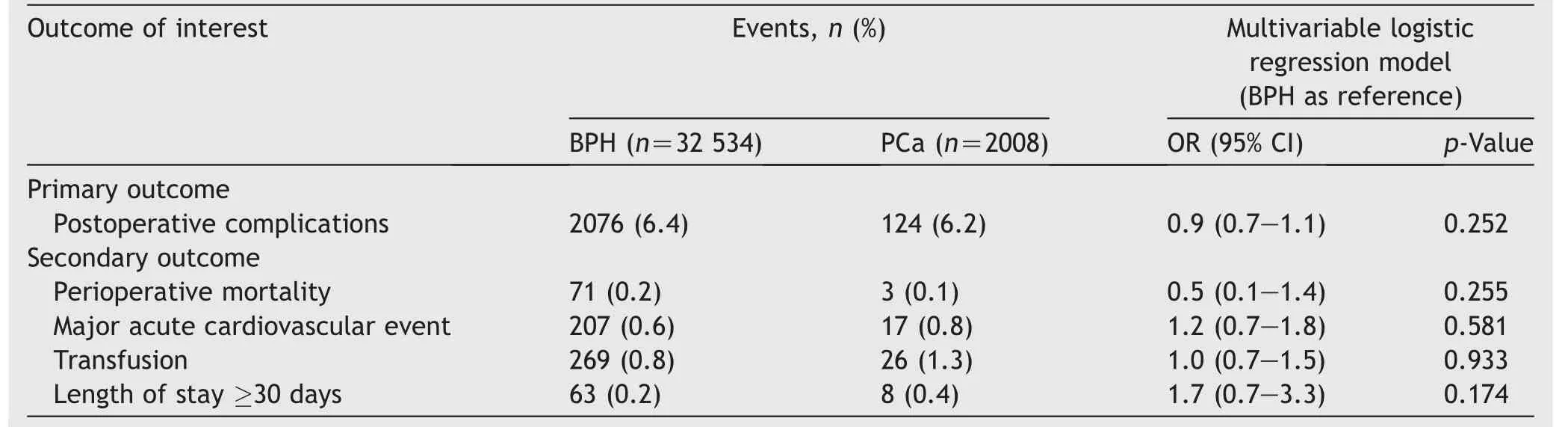
Table 3 Multivariable logistic regression model comparing event rates between BPH and PCa patients.
After stratification according to the surgical technique used (Supplementary material 3),enucleation showed the lowest complication rate(5.1%)compared to TURP and PVP(6.4% and 6.6%,respectively;p=0.043).Conversely,PVP showed the lowest transfusion rate(0.3%)compared to TURP and enucleation (1.1% and 1.2%,respectively;p<0.001).However,in logistic regression models,all interaction tests failed to find any statistically significant interaction between diagnosis and procedure type for all outcomes of interest(allp>0.05).
4.Discussion
We hypothesized that patients harboring PCa might experience higher surgical and non-surgical complication rates.We explored several outcomes,including composite outcomes namely major cardiovascular events.Our analysis,after adjusting for several possible confounders showed that this might not be the case and confirmed the safeness of transurethral surgery,even in PCa patients.Our results raise several interesting and clinically meaningful points of discussion.
First,within the ACS-NSQIP database up to 6% of transurethral prostate surgery procedures were performed in PCa patients.Most of the PCa patients were treated by TURP (78.4%) and TURP was more frequently used in those with PCa than BPH (78.4%vs.62.7%).These results reflect surgeon preference for TURP in presence of PCa corroborating results from more historical studies.Tan and colleagues [10]reported that 35% of patients diagnosed withde novometastatic PCa require local palliative treatments,and 13% are due to acute urinary retention.Authors also reported that the most frequently performed procedure,up to 89% of cases,is TURP [10].It is of note that Tan et al.[10]investigated the use of TURP in a palliative setting with no comparison to TURP performed for benign conditions.Differently,we excluded patients with a diagnosis of disseminated cancer to reduce inherent differences between patients with BPH and PCa.Indeed,patients with symptomatic metastatic PCa might also be affected by hematuria (27%),renal impairment (17%),and other conditions not-related to bladder obstruction [10].In these cases,TURP could be performed only for bleeding control and not to obtain satisfactory bladder outlet unblocking.Our aim was instead to explore the effect of PCa diagnosis on surgery safeness,avoiding the confounding effect of cancer complications.However,it is of note that also in our cohort,even after applying different selection criteria TURP was more frequently used in PCa patients.
Moreover,our analyses showed that PCa patients do not experience higher complication rates compared to their BPH counterpart (6.2%vs.6.4%).Lack of evidence of differences in complication rates after surgery was confirmed in multivariable models adjusting for baseline patients’characteristics.In addition,models including formal interaction test between diagnosis and surgical technique used failed to show any differential effect of surgical technique on outcomes of interest,based on the diagnosis.These findings are of crucial importance suggesting all techniques could apply to PCa patients,with no detrimental effect on complications.The latter allows a surgeon to choose the preferable technique also in these patients,based on their experience and patients’ characteristics.
In this regard,Jibara et al.[17]reported results of photoselective vaporization of the prostate with the GreenLight XPS 180 W Laser System.The authors included 71 patients in active surveillance for PCa in their analyses and reported only two cases of Grade III complications according to the Clavien-Dindo classification.Similarly,Choi et al.[18]reviewed data of 83 patients diagnosed with PCa who underwent palliative TURP,that were compared to those who did not.Investigators highlighted the feasibility of TURP in advanced PCa patients,with acceptable complication rates(about 17% at 90 days)and no death reported.The feasibility and safety of palliative TURP were also investigated by Pelletier et al.[19]in a cohort of 58 patients.The authors reported only four cases of Clavien-Dindo Grade III complications corroborating our results on transurethral prostate surgery safeness.Taken together all these results with ours suggest that transurethral surgery of the prostate is feasible even in PCa patients.Still,our analyses showed different safeness profile in terms of overall complications and transfusion rates and a more favorable profile of enucleation and PVP.Such results are in line with those by Kumar et al.[20]that showed an advantage of PVPin terms of perioperative blood loss,need for postoperative irrigation,duration of postoperative irrigation,and catheterization compared to TURP counterpart.These findings suggest that treatment type choice could be guided based on prostate size[21]and bleeding risk as for BPH[1].
Our analyses,along with previous studies,show that surgical outcomes of transurethral prostate surgery seem to be not influenced by the underlying disease.Nevertheless,we need to acknowledge several limitations such as the retrospective nature of this study and the intrinsic limits of a national database.Data granularity did not allow us to include important covariates and address several critical confounders namely baseline prostate-specific antigen,prostate size,tumor grade,and stage.Some of these covariates have been demonstrated to play an important role in surgical outcomes and could be important confounders [22].Moreover,ICD codes correspond to the condition noted as the postoperative diagnosis and might include diagnosis obtained after pathology report return.Therefore,a proportion of patients might have been diagnosed as incidental PCa.Unfortunately,ACS-NSQIP dataset does not include data about previous prostate biopsy;therefore,no adjustment or stratification could be performed to control such confounding bias.However,it is of note that the proportion of patients with diagnosis of PCa who underwent PVP or enucleation in our cohort is quite similar (11.5%vs.10.1%).Previous studies reported a significantly higher percentage of incidental PCa after enucleation than TURP (23.3%vs.8.3%) [23].In addition,pathology specimens after PVP,depending on the approach used,might be too scarce for obtaining a diagnosis [24].Thus,we might conclude that differences in technique use truly reflect surgeons’ choice and that the proportion of incidental PCa represents a minority of PCa arm.In addition,we must consider that the hypothesis tested was that PCa patients have higher complication rates due to the inherent nature of cancer.Such hypothesis test is not affected by the incidental nature of PCa diagnosis.In addition,lack of oncological data also does not affect the study design since we did not aim to test any oncological outcome.Therefore,even if we acknowledge that comprehensive analyses including oncological data are warranted,the present study did not aim to explore also that field.Still,the lack of data about previous,contemporary,or subsequent treatments for PCa represents a minor limitation of our study since our focus is still exploring surgical outcomes and not oncological ones.Previous studies exploring oncological safeness of transurethral prostate surgery showed controversial results.Indeed,in patients with localized disease few cases of progression were reported (7/71) and high probability of active surveillance persistence were recorded(up to 93% at 3-year) [17].Conversely,in more advanced disease TURP patients had shorter cancer-specific and overall survival,even after propensity score matching [18].Therefore,concerns about oncological safeness and cytoreductive effect of transurethral surgery remain,even if in wellselected patients such approach is feasible.
In addition,ACS-NSQIP granularity did not allow us to be specific about the energy source used during TURP or PVP(i.e.,monopolar,bipolar,and laser type).Finally,we could explore only perioperative complication,while studies with more mature follow-up are needed to test the effect of PCa on long-term complications,including bladder neck contracture [25].Nevertheless,to the best of our knowledge,this represents the largest study comparing surgical outcomes after transurethral prostate surgery between BPH and PCa which relied on thousands of patients.
5.Conclusion
Within a large national dataset,transurethral prostate surgery seems to provide comparable surgical outcomes either performed for BPH or PCa.Moreover,no effect of underlying diagnosis has been shown on surgical performance.As a consequence,surgeons are allowed to use the surgical technique that they repute more appropriate for every single patient or the one that they are more confident with.
Author contributions
Study concept and design: Michele Marchioni,Riccardo Autorino,Giulia Primiceri.
Data acquisition: Michele Marchioni.
Data analysis: Michele Marchioni.
Drafting of manuscript: Michele Marchioni,Riccardo Autorino,Alessandro Veccia.
Critical revision of the manuscript: Michele Marchioni,Giulia Primiceri,Alessandro Veccia,Marta Di Nicola,Umberto Carbonara,Fabio Crocerossa,Ugo Falagario,Ambra Rizzoli,Riccardo Autorino,Luigi Schips.
Supervision: Riccardo Autorino,Luigi Schips.
Conflicts of interest
The authors declare no conflict of interest.
Acknowledgment
The American College of Surgeons National Surgical Quality Improvement Program and the hospitals participating in the ACS NSQIP are the source of the data used herein;they have not verified and are not responsible for the statistical validity of the data analysis or the conclusions derived by the authors.
Appendix A.Supplementary data
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ajur.2022.05.008.
杂志排行
Asian Journal of Urology的其它文章
- Transurethral resection of bladder tumor:A systematic review of simulator-based training courses and curricula
- Etiology and management of urethral calculi:A systematic review of contemporary series
- Oncologic outcomes with and without amniotic membranes in robotic-assisted radical prostatectomy: A propensity score matched analysis
- Single nucleotide polymorphism within chromosome 8q24 is associated with prostate cancer development in Saudi Arabia
- The risk of prostate cancer on incidental finding of an avid prostate uptake on 2-deoxy-2-[ 18F]fluoro-D-glucose positron emission tomography/computed tomography for non-prostate cancer-related pathology:A single centre retrospective study
- Prevention of thromboembolic events after radical prostatectomy in patients with hereditary thrombophilia due to a factor V Leiden mutation by multidisciplinary coagulation management
