重症患者医院获得性血小板减少的预后因素分析
2023-11-01吕世进蒋镇宏张国虎夏金明郭亮赖登攀
吕世进,蒋镇宏,张国虎,夏金明,郭亮,赖登攀
重症患者医院获得性血小板减少的预后因素分析
吕世进,蒋镇宏,张国虎,夏金明,郭亮,赖登攀
杭州师范大学附属医院急诊科,浙江杭州 310015
探讨重症患者医院获得性血小板减少的预后影响因素。回顾性分析2020年1月至2021年12月杭州师范大学附属医院的急诊重症监护室(emergency intensive care unit,EICU)入院时血小板计数正常,入院后复查血小板计数低于正常值的患者的临床资料。分析患者的一般资料、实验室指标、是否有机械通气、住院时间及28d病死率的差异;采用多因素Logistic回归分析评价血小板减少的影响因素。共纳入141例医院获得性血小板减少患者。血小板减少在EICU中的发病率为21.04%(141/670),病死率为33.33%(45/135)。住院天数为15(9,22)d。单因素分析结果显示,脓毒症(=0.017)、血小板减少的程度(<0.001)、白细胞计数(=0.029)、中性粒细胞比例(=0.029)、乳酸水平(<0.001)、总胆红素水平(=0.025)、降钙素原(=0.012)、急性生理学和慢性健康状况评价Ⅱ(acute physiology and chronic health evaluation Ⅱ,APACHE Ⅱ)评分(=0.004)、血小板减少的天数(=0.006)、住院天数(=0.001)、机械通气(=0.001)是影响预后的相关因素。将上述因素纳入多因素Logistic回归分析结果显示,血小板轻度减少(=0.007,=4.932)、中性粒细胞比例(=0.044,=0.923)、血小板减少的天数(=0.031,=0.883)、住院天数(<0.001,=1.221)、机械通气(<0.001,=0.077)是影响血小板减少重症患者预后的独立因素。血小板轻度减少、中性粒细胞比例、血小板减少天数、住院天数、机械通气是影响血小板减少重症患者预后的独立因素。
医院获得性;血小板减少;危险因素;预后
人体血液细胞成分,除了红细胞、白细胞,还有一种重要的成分——血小板。血小板是一种形状多样、无细胞核的胞质小体,由骨髓巨核细胞裂解而来,具有聚集、黏附、激活和释放功能。大量临床研究证明,血小板在凝血、止血及炎症细胞调节方面起着重要作用。患者在应激状态下,常常出现功能障碍和细胞过度活化,一旦内皮细胞功能不全时,血小板发挥其促凝、抗纤、黏附、募集及活化等作用[1]。白细胞、血小板及内皮细胞三者之间互相协同作用增加了内皮细胞功能不全,进而引发明显的炎症反应和血栓形成,在整个过程中血小板起着非常重要的作用[2]。
血小板减少是临床患者常见并发症之一,重症患者更容易发生血小板减少。血小板减少严重威胁着重症患者的生命安全[3]。据文献报道,成人重症监护病房(intensive care unit,ICU)患者血小板减少发生率为8.3%~67.6%[4-5]。影响血小板减少的因素多种多样,包括原发性因素和继发性因素。发生血小板减少的重症患者其组织器官出血风险和机体需要的输血量也显著增加,甚至死亡率也明显增加[6-7]。但影响医院获得性血小板减少(入院时血小板计数≥100×109/L,入院后血小板计数<100×109/L)的重症患者预后因素仍不明确,目前临床研究表明,医院获得性血小板减少的病因有创伤、严重感染、营养障碍、免疫紊乱等多种疾病,病因复杂[8]。本研究旨在探讨医院获得性血小板减少症患者的发病原因及预后情况。
1 资料与方法
1.1 临床资料
采用回顾性研究方法,选取2020年1月至2021年12月杭州师范大学附属医院急诊重症监护室(emergency intensive care unit,EICU)收治的141例血小板减少患者为研究对象。纳入标准:①年龄18~75岁;②入院时血小板计数(platelet count,PLT)≥100×109/L,入院后复查PLT低于正常值。排除标准:①1个月内发生血栓类似疾病;②再生障碍性贫血等原发性骨髓增生异常;③近3个月接受过免疫治疗、放疗、化疗;④系统性红斑狼疮等免疫相关性疾病。本研究符合医学伦理学标准,通过杭州师范大学附属医院伦理委员会批准(伦理审批号:202211211559000157124),获得患者本人或者家属知情同意。
1.2 诊断标准
PLT<50×109/L为严重血小板减少;PLT<100×109/L且>50×109/L为轻度血小板减少。PLT正常范围为≥100×109/L。
1.3 观察指标
①一般资料:记录患者的年龄、性别、急性生理学和慢性健康状况评价Ⅱ(acute physiology and chronic health evaluation Ⅱ,APACHE Ⅱ)、基础疾病(包括高血压、冠心病、慢性阻塞性肺疾病、糖尿病、肾功能不全等)、住院天数、是否有机械通气;②引起血小板减少的原因:脓毒症、非脓毒症的因素;③实验室检查的结果:首次出现血小板减少时,是否PLT>50×109/L、白细胞计数、中性粒细胞比例、血红蛋白、C反应蛋白、乳酸、总胆红素、血白蛋白、肌酐、降钙素原等指标;④预后相关指标:住院时间、住院费用及28d结局。
1.4 统计学方法
2 结果
2.1 血小板减少发生率、病死率、住院天数和发生恢复时间
血小板减少在EICU中的发病率为21.04%(141/670),患者的病死率为33.33%(45/135)。患者住院天数为15(9,22)d,入院至出现血小板减少的中位数时间为2d,出现血小板减少至恢复正常中位数时间为5d,28d存活率为68.09%。
2.2 血小板减少患者的28d生存情况
141例患者中,28d内病死45例(31.91%)。图1可见血小板轻度减少组(PLT<100×109/L且>50×109/L)患者的生存时间明显更长,差异有统计学意义(<0.05)。
2.3 28d生存相关因素的单因素分析
单因素分析结果显示,脓毒症(=0.017)、血小板减少的程度(<0.001)、白细胞计数(=0.029)、中性粒细胞比例(=0.029)、乳酸水平(<0.001)、总胆红素水平(=0.025)、降钙素原(=0.012)、APACHEⅡ评分(=0.004)、血小板减少的天数(=0.006)、住院天数(=0.001)、机械通气(=0.001)是影响预后的相关因素,见表1。
2.4 28d生存相关因素的多因素Logistic分析
将上述因素纳入多因素Logistic分析结果显示,血小板轻度减少(=0.007,=4.932)、中性粒细胞比例(=0.044,=0.923)、血小板减少天数(0.031,=0.883)、住院天数(=0.000,=1.221)、机械通气(<0.001,=0.077)是影响血小板减少重症患者预后的独立因素,见表2。其中血小板轻度减少、住院天数是保护性因素。

表1 28d生存相关因素的单因素分析
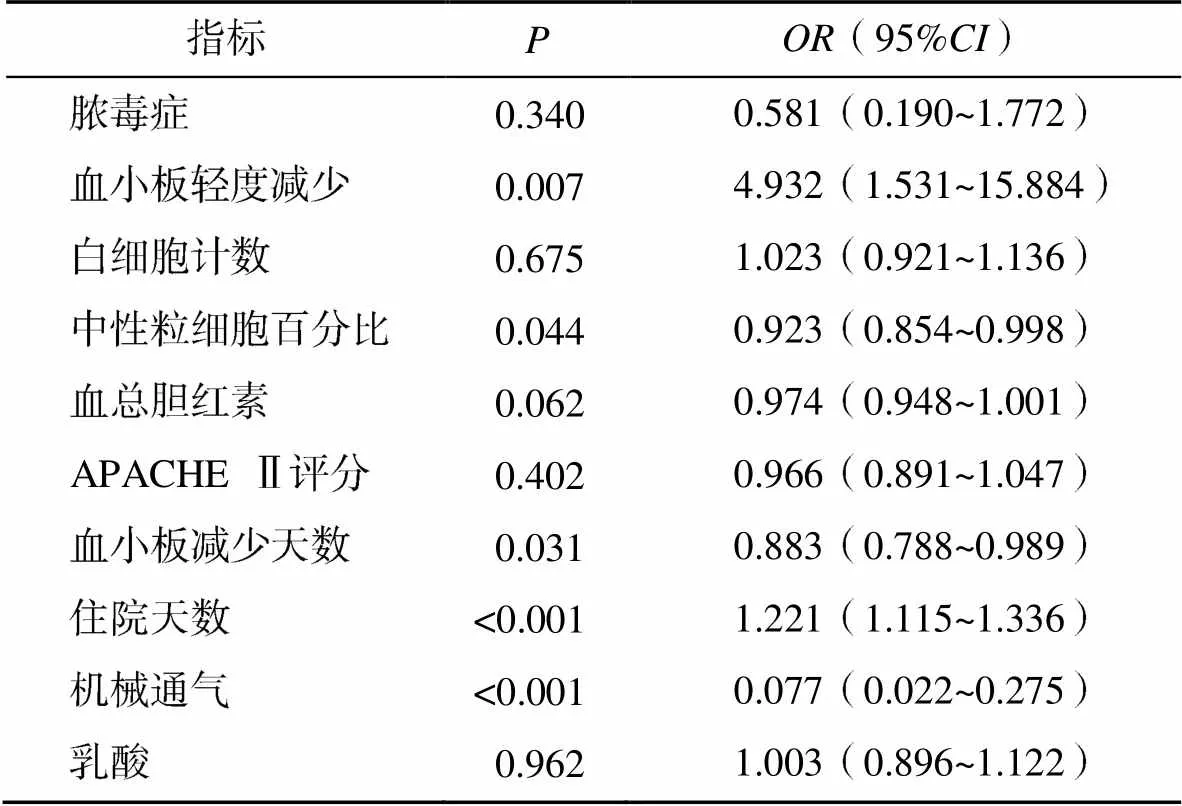
表2 28d生存相关因素的多因素Logistic分析
3 讨论
血小板减少在重症患者中十分常见,文献报道,在治疗期间血小板减少患者的发生率为14%~44%[4-5]。本研究中,血小板减少的发病率为21.04%,与文献报道相符。患者血小板减少可分为原发性和获得性血小板减少[9]。原发性血小板减少影响因素多为血液系统疾病、感染性疾病、严重创伤、免疫系统功能紊乱、营养缺乏等多种疾病。临床上依据病理生理学进行分类,分为血小板生成减少、血小板消耗增加、血小板破坏增多、血小板分布异常以及各种输液致血液稀释5种机制[10]。重症患者发生获得性血小板减少通过2种或2种以上机制引起血小板减少,如严重肝病患者发生血小板减少原因有骨髓抑制血小板生成减少和自身抗体形成致血小板破坏增多,也可因凝血功能异常出血消耗[11-12]。原发性血小板减少有3种及以上发病机制,获得性血小板减少也有2种以上发病机制[13-14]。研究报道,发生获得性血小板减少重症患者的病因依次为:脓毒症、弥散性血管内凝血、稀释性血小板减少、叶酸缺乏、药物相关性血小板减少[15-17]。药物相关血小板减少常见于肝素诱导的血小板减少。本研究中,脓毒症导致医院获得性血小板减少占血小板减少因素的47.52%。脓毒症致血小板减少原因包括严重感染致骨髓抑制、巨噬细胞吞噬作用、补体激活、微小血栓形成、组胺类物质释放等[18-19]。临床鉴别假性血小板减少,包括实验室检查误差及采血所致的异常[20-21]。脓毒症患者一旦出现血小板减少,其住院时间延长,脏器功能恢复需更长时间,出血事件发生率增加,导致病死率上升[22-23]。PLT越低,释炎症因子就越多,激活内皮细胞和补体信号通路更多,各种炎症反应、器官损害增多,病死率增加[24]。脓毒症患者血小板减少具有双向性,脓毒症早期(1~4d)出现PLT下降,之后很快升至正常,该患者预后相对较好;一类患者持续性PLT降低或持续PLT不升,提示预后不良[25]。早期预防血小板减少和促进PLT恢复可降低脓毒性休克患者的病死率[26]。研究报道,脓毒症合并血小板减少的患者应用升血小板药物可降低此类患者的病死率[27-28]。本研究中,患者28d生存相关单因素分析结果显示,脓毒症合并血小板减少与非脓毒症患者比较差异有统计学意义,死亡风险增加,血小板轻度减少患者预后较好,两组比较差异有统计学意义;代表炎症指标的白细胞计数、中性粒细胞百分比、降钙素原水平,两组比较差异有统计学意义,死亡组明显高于生存组;乳酸水平和APACHEⅡ评分两组比较差异有统计学意义,患者乳酸水平和APACHEⅡ评分越高其死亡风险越高。28d生存相关多因素Logistic回归分析结果显示,血小板减少持续的天数、住院天数及机械通气时间与患者的生存相关,差异有统计学意义。轻度血小板减少患者预后较重度血小板减少的生存率高,血小板轻度减少者,原因是原发疾病对患者血液系统损伤轻或者对治疗效果好、恢复快,因而预后较好。住院天数是保护因素,在疾病严重程度相似的情况下,患者对治疗反应明显,治疗效果好,因此,住院天数越少,患者预后越好。Dominique等[29]研究发现,机械通气持续的天数是影响血小板减少患者预后的独立危险因素。
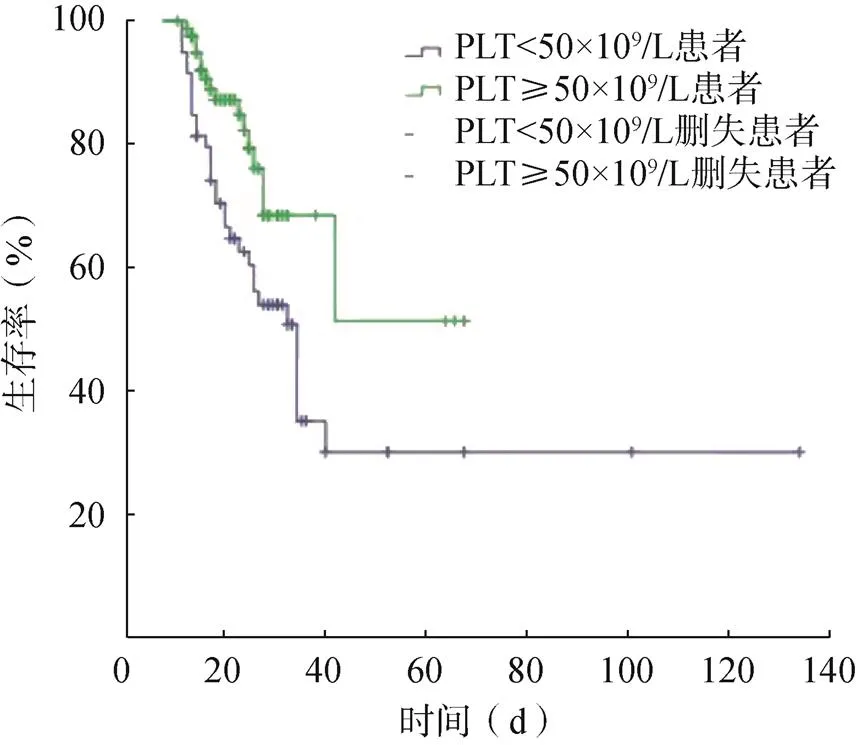
图1 累积生存分析的Kaplan-Meier曲线
目前本研究尚有一定局限性,危重症是一个动态的实体,包括各种混杂因素,本研究没有调查输血、连续性肾脏替代治疗、体外膜肺氧合等干预措施的影响或药物的影响,是一项单中心观察性研究,因此研究结果可能会有偏倚。
综上所述,医院获得性血小板减少在重症患者中十分常见,尤其是脓毒症患者,预防脓毒症发生和及时救治非常重要。监测PLT水平、血小板减少持续天数、住院天数、机械通气时间等,有助于临床上更好地判断血小板减少重症患者的病情严重程度和预后。
[1] JOFFRE J, HELLMAN J, INCE C, et al. Endothelial responses in sepsis[J]. Am J Respir Crit Care Med, 2020, 202(3): 361–370.
[2] IBA T, LEVY J H. Inflammation and thrombosis: roles of neutrophils, platelets and endothelial cells and their interactions in thrombus formation during sepsis[J]. J Thromb Haemost, 2018, 16(2): 231–241.
[3] HUI P, COOK D J, LIM W, et al. The frequency and clinical significance of thrombocytopenia complicating critical illness: a systematic review[J]. Chest, 2011, 139(2): 271–278.
[4] SONG J C, LIU S Y, ZHU F, et al. Expert consensus on the diagnosis and treatment of thrombocytopenia in adult critical care patients in China[J]. Military Med Res, 2020, 7(1): 15.
[5] WILLIAMSON D R, LESUR O, TÉTRAULT J P, et al. Thrombocytopenia in the critically ill: prevalence, incidence, risk factors, and clinical outcomes[J]. Can J Anaesth, 2013, 60(7): 641–651.
[6] WILLIAMSON D R, ALBERT M, HEELS-ANSDELL D, et al. Thrombocytopenia in critically ill patients receiving thromboprophylaxis: frequency, risk factors, and outcomes[J]. Chest, 2013, 144(4): 1207–1215.
[7] LAUZIER F, ARNOLD D M, RABBAT C, et al. Risk factors and impact of major bleeding in critically ill patients receiving heparin thromboprophylaxis[J]. Intensive Care Med, 2013, 39(12): 2135–2143.
[8] HASAN M J, RABBANI R, HUQ S. The use of high dose eltrombopag in the management of sepsis- associated thrombocytopenia in critically ill patients[J]. J Crit Care Med (Targu Mures), 2019, 5(4): 123–129.
[9] ZHANG J, LU Z, XIAO W, et al. Efficacy and safety of recombinant human thrombopoietin on sepsis patients with thrombocytopenia: a systematic review and meta-analysis[J]. Front Pharmacol, 2020, 11: 940.
[10] THACHIL J, WARKENTIN T E. How do we approach thrombocytopenia in critically ill patients[J]. Br J Haematol, 2017, 177(1): 27–38.
[11] GIUSTOZZI M, EHRLINDER H, BONGIOVANNI D, et al. Coagulopathy and sepsis: pathophysiology, clinical manifestations and treatment[J]. Blood Rev, 2021, 50: 100864.
[12] SMITH L. Disseminated intravascular coagulation[J]. Semin Oncol Nurs, 2021, 37(2): 151135.
[13] ANTIER N, QUENOT J P, DOISE J M, et al. Mechanisms and etiologies of thrombocytopenia in the intensive care unit: impact of extensive investigations[J]. Ann Intensive Care, 2014, 4: 24.
[14] WU X H, LI Y, TONG H S. Research advances in the subtype of sepsis-associated thrombocytopenia[J]. Clin Appl Thromb Hemost, 2020, 26(1): 107–116.
[15] TORUN E G, YAZICI M U, AZAPAGASI E, et al. Thrombocytopenia-associated multi-organ failure due to diabetic ketoacidosis and viral infection: a case report [J]. Klin Padiatr, 2021, 233(3): 149–151.
[16] NGUYEN T C. Thrombocytopenia-associated multiple organ failure [J]. Crit Care Clin, 2020, 36(2): 379–390.
[17] IBA T, WARKENTIN T E, CONNORS J M, et al. Therapeutic strategies in patients with coagulopathy and disseminated intravascular coagulation: awareness of the phase-dependent characteristics[J]. Minerva Med, 2021, 112(6): 701–712.
[18] ZARYCHANSKI R, HOUSTON D S. Assessing thrombocytopenia in the intensive care unit: the past, present, and future[J]. Hematol-Am Soc Hemat, 2017, 2017(1): 660–666.
[19] MENARD C E, KUMAR A, HOUSTON D S, et al. Evolution and impact of thrombocytopenia in septic shock: a retrospective cohort study[J]. Crit Care Med, 2019, 47(4): 558–565.
[20] 尹春琼, 白志瑶, 王玉明, 等. 外周血细胞假性危急值标本分析[J]. 实用检验医师杂志, 2019, 11(1): 45–48.
[21] TUFAN-PEKKUCUKSEN N, GAZZANEO M C, AFONSO N S, et al. Thrombocytopenia-associated multi- organ failure secondary to hyperglycemic, hyperosmolar non-ketotic syndrome: a case report [J]. Pediatr Diabetes, 2018, 19(3): 574–577.
[22] DHUNPUTH P, ACHARYA R, UMAKANTH S, et al. Clinical profile of thrombocytopenia in acute febrile illnesses; a hospital-based study[J]. Kathmandu Univ Med J, 2021, 19(74): 248–252.
[23] LEE H H, HONG S J, AHN C M, et al. Clinical implications of thrombocytopenia at cardiogenic shock presentation: data from a multicenter registry[J]. Yonsei Med J, 2020, 61(10): 851–859.
[24] CLAUSHUIS T A, VAN VUGHT L A, SCICLUNA B P, et al. Thrombocytopenia is associated with a dysregulated host response in critically ill sepsis patients[J]. Blood, 2016, 127(24): 3062–3072.
[25] AKCA S, HAJI-MICHAEL P, DE MENDONÇA A, et al. Time course of platelet counts in critically ill patients[J]. Crit Care Med, 2002, 30(4): 753–756.
[26] XIANG B, ZHANG G, GUO L, et al. Platelets protect from septic shock by inhibiting macrophage-dependent inflammation via the cyclooxygenase 1 signalling pathway[J]. Nat Commun, 2013, 4: 2657.
[27] XIE Y, TIAN R, XIE H, et al. The clinical significance of thrombocytopenia complicating sepsis: a meta- analysis[J]. J Infect, 2019, 78(4): 323–337.
[28] ZHOU X, TANG G. Some doubts on the meta-analysis of the clinical significance of thrombocytopenia complicating sepsis[J]. J Infect, 2019, 79(3): 277–287.
[29] VANDIJCK D M, BLOT S I, DE WAELE J J, et al. Thrombocytopenia and outcome in critically ill patients with bloodstream infection [J]. Heart Lung, 2010, 39(1): 21–26.
Prognostic factors for hospital-acquired thrombocytopenia in severe patients
Department of Emergency, Hangzhou Normal University Affiliated Hospital, Hangzhou 310015, Zhejiang, China
To investigate the relevant factors affecting prognosis of hospital-acquired thrombocytopenia in severe patients.The clinical data of patients with normal platelet count at admission and lower platelet count after admission in Emergency Intensive Care Unit (EICU), Hangzhou Normal University Affiliated Hospital from January 2020 to December 2021 were retrospectively analyzed. The differences of general data, laboratory indexes, whether there was mechanical ventilation, hospitalization time and 28 d mortality were analyzed. The influencing factors of thrombocytopenia were analyzed by multivariate Logistic regression.A total of 141 patients with hospital-acquired thrombocytopenia were included. The incidence of thrombocytopenia in EICU was 21.04% (141/670), and the mortality was 33.33% (45/135). The hospitalization time was 15(9, 22) d. Univariate analysis showed that sepsis (=0.017), degree of thrombocytopenia (<0.001), white blood cell count (=0.029), neutrophil ratio (=0.029), lactate level (<0.001), total bilirubin level (=0.025), procalcitonin (=0.012), Acute Physiology and Chronic Health Evaluation Ⅱ (APACHE Ⅱ) score (=0.004), days of thrombocytopenia (=0.006), hospitalization time (=0.001), and mechanical ventilation (=0.001) were relevant factors affecting prognosis. Multivariate logistic regression analysis of the above factors showed that mild thrombocytopenia (=0.007,=4.932), neutrophil ratio (=0.044,=0.932), days of thrombocytopenia (=0.031,=0.883), hospitalization time (<0.001,=1.221), and mechanical ventilation (<0.001,=0.077) were independent factors affecting the prognosis of severe patients with thrombocytopenia.Mild thrombocytopenia, neutrophil ratio, days of thrombocytopenia, hospitalization time, and mechanical ventilation were independent factors affecting the prognosis of severe patients with thrombocytopenia.
Hospital-acquired; Thrombocytopenia; Risk facors; Prognosis
R558.2
A
10.3969/j.issn.1673-9701.2023.29.017
浙江省卫生和计划生育委员会中医药管理局项目(2020ZB200)
蒋镇宏,电子信箱:1169847664@qq.com
(2023–04–01)
(2023–09–15)